This is an old revision of the document!
Table of Contents
Osteoporosis
Introduction
The adult human skeleton is composed of 206 bones, where there is continuous breaking down and replacing of these bones (Morrison, 2016). The remodeling of these bones occurs with the help of two special bone cells that include osteoclast and osteoblast (Morrison, 2016). Osteoclasts help break the bone down, while the osteoblasts help create the new bone (Morrison, 2016). The coordination between the osteoclast and osteoblast is really important for the well being of the human body (Morrison, 2016). Osteoporosis occurs when osteoclast starts to break down bones faster than the osteoblast can create (Morrison, 2016).
Osteoporosis is a common disorder that gets characterized by the deterioration of bone tissues and low bone density (Christodoulou and Cooper, 2003). This bone disease leads to an increase in fracture risks and a decrease in the strength of bones (Christodoulou and Cooper, 2003). Osteoporosis is most commonly associated with vertebral, wrist, and hip fractures and is seen to affect both male and females (Christodoulou and Cooper, 2003).
Morrison, W. (2016). Osteoporosis Causes: Remodeling, Balance, and Hormones. Retrieved from https://www.healthline.com/health/osteoporosis-causes
Christodoulou, C., & Cooper, C. (2003). What is osteoporosis?. Postgraduate medical journal, 79(929), 133-138.
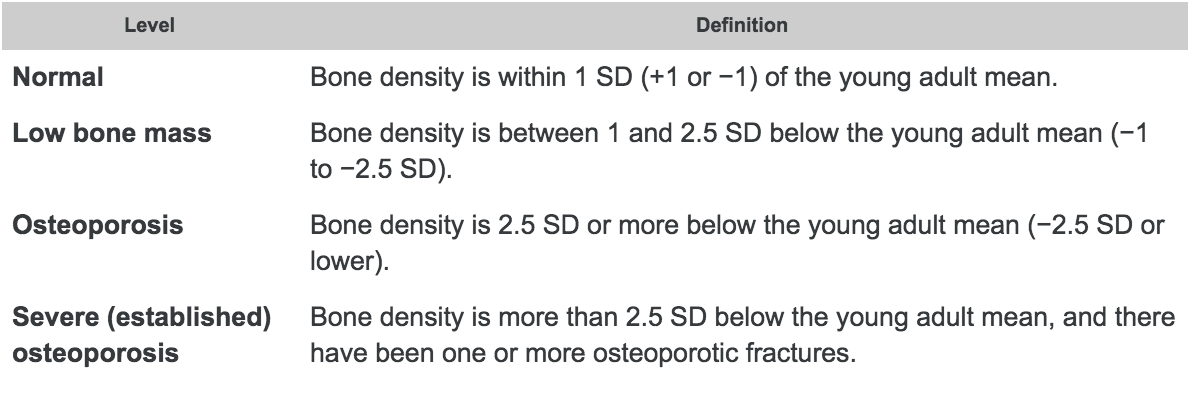
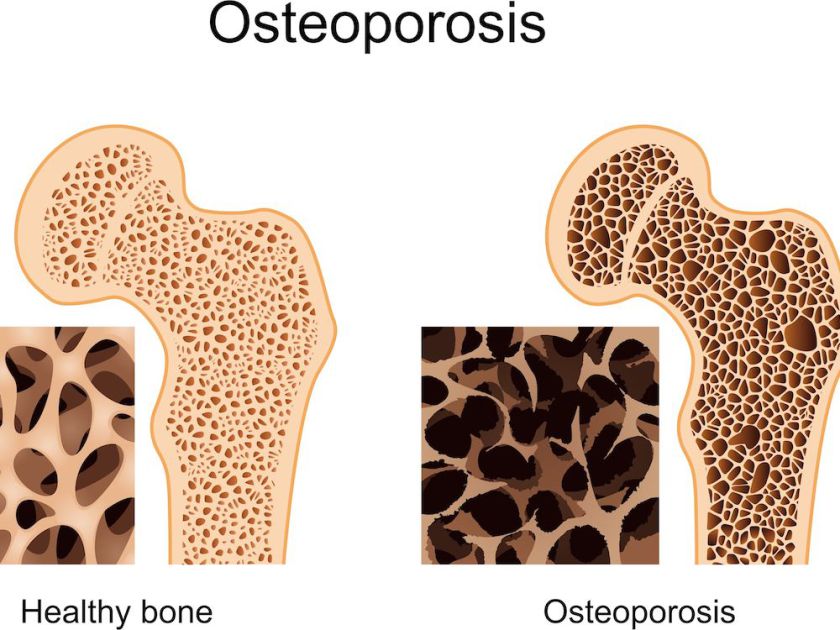 Figure 1: Healthy bone vs. bone with osteoporosis as identified by porous quality.
Figure 1: Healthy bone vs. bone with osteoporosis as identified by porous quality.
History
The discovery of the correlation between age-related deterioration in bone mass and density and the resulting risk in fractures can be dated back to the writings of 18th century British surgeon, Astley Cooper, who observed the “thin and spongy texture” of the bones of older patients (Grob, 2014). Furthermore, skeletal remains that have been studied by anthropologists have shown decreased bone density associated with chronic malnutrition, which is an identified risk factor of the bone disease (Grob, 2014).
Epidemiology
Osteoporosis is one of the most common bone diseases among elderlies in Canada, affecting more than 2 million Canadians(Lyda, 2014); costing more than 456 million dollars annually (Government of Canada, 2016). However, since patients are usually not aware of this disease at early stages, this number may exclude ones not yet diagnosed. In 2002, the WHO found that osteoporosis has the 6th highest DALY (Disability-adjusted life years) in Europe and Americas. DALY is measures the cost of burdened disability compared to the regular life expectancy; calculated by total years of disability plus the difference in years of early death compared to the local life expectancy. In Canada, one in every three female and one in five male will be diagnosed with osteoporosis (Osteoporosis Canada, 2018). Osteoporosis may begin as early as in the the mid-30s, however it is usually not diagnosed until late in life. The most common sites of osteoporosis include the vertebrae, the hip and wrists (Masi, 2008).
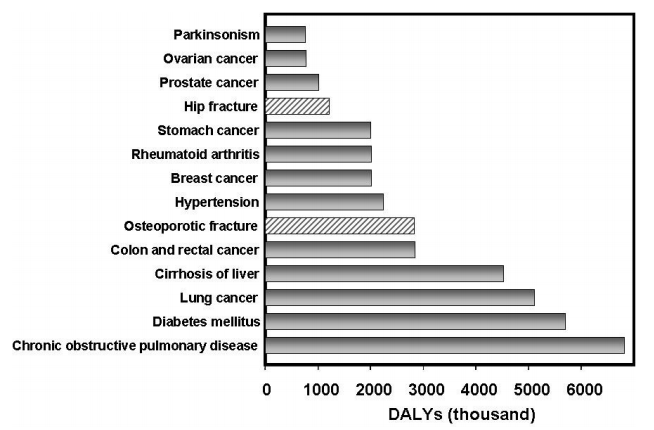 Figure 2: Disability-adjusted life year in thousands for varies chronic diseases.
Figure 2: Disability-adjusted life year in thousands for varies chronic diseases.
Risk Factors
Risk factors for osteoporosis differ between individuals under and over the age of 50.
Younger adults (age < 50 years):
- Experience with bone fracture
- Use of glucocorticoids (hormonal steroid as immune response suppressor)
- Lack of hormone production
Older adults (age > 50 years):
- Older than 65 years old
- Smoking
- Long term intake of large quantity of alcohol
- Underweight or rapid weight loss
- Having diseases that have complications leading to bone loss
(Public health agency of Canada, 2008)
Signs and Symptoms
For individuals that have osteoporosis, treating this disease early on is the best way to prevent more serious risks, but being able to detect bone loss signs early on is really unusual (Minnis, 2016). A couple signs that have been visible for individuals with osteoporosis in the early age include having a weaker grip strength, weaker fingernails, and receding gums (Minnis, 2016). As the individual enters a later stage of osteoporosis, an increase in bone loss is observed (Minnis, 2016). At this stage, the individual begins to observe more obvious signs (Minnis, 2016). These signs include neck and back pain, fractures that occur from a fall, getting a hunched back, and a loss of height (Minnis, 2016). For individuals with osteoporosis, areas of fracture include hip, wrist, and spine (Minnis, 2016).
Minnis, G. (2016). Osteopeorosis Symptoms: Early and Late Stages. Retrieved from https://www.healthline.com/health/osteoporosis-symptoms#complications
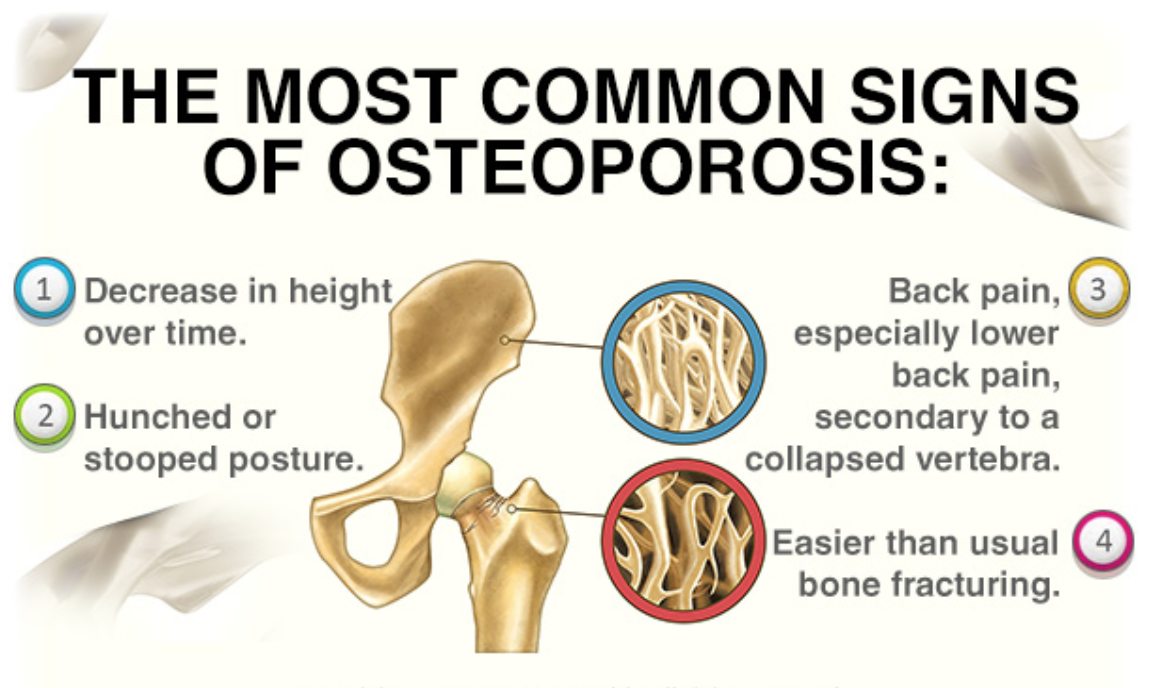 Figure 3: Four common signs of osteoporosis that is prevalent such as decrease in height overtime, hunched or stooped posture, back pain, and easier than usual bone fracturing.
Figure 3: Four common signs of osteoporosis that is prevalent such as decrease in height overtime, hunched or stooped posture, back pain, and easier than usual bone fracturing.
Diagnosis
The bone mass density, also known as BMD, is the primary test that can be used to determine the bone strength using a dual X-ray absorptiometry. The scanned bone from either the hip or spine from an individual can determine the bone density to determine the diagnosis as well as any future fracture risks (Sozen, Ozisik, and Calik 2017). The World Health Organization (WHO) presents that osteoporosis is determined when an individual has 2.5 standard deviation below the average using a T-score. This can be performed from knowing the difference between the patient’s BMD and the average to compare with the severity of the diagnosis (Sozen, Ozisik,and Calik 2017). The results are usually compared to a healthy 30-year old adult’s bone mineral density. Therefore, a lower BMD number will indicate a higher risk of a fracture (National Resource Center, 2015).
Figure 5: A table demonstrating the comparison of standard deviations created by the World Health Organization (WHO).
Screening & Measuring Tools
Dual-energy x-ray absorptiometry (DEXA) is a method that can be performed on different areas to determine osteoporosis with a low radiation dose. This method consists of two energies where the x-ray goes across the desired area. Areas often included are the lumbar spine and proximal femur. However, if these areas are unavailable, the forearm can also be used to scan for BMD measurement (Ramos et al., 2011).
Another method used to determine osteoporosis is determined using blood tests or bone biopsies. Blood tests are able to indicate certain proteins such as alkaline phosphatase. An individual with a higher amount of alkaline phosphatase has a higher indication with certain bone diseases. Calcium levels in the blood can also indicate if an individual has enough calcium intake (Institute for Quality and Efficiency in Health Care, 2017).
Pathophysiology
Osteoporosis is a systemic disease of the bones characterized by a low skeletal bone density and mass, as well as deterioration of bone tissues. Together, these cause an individual with osteoporosis to have an increased risk of bone fracture (Garnero, 2008).
Around the ages between 40 and 50, bone mass starts to decrease in both men and women at a yearly rate of 0.3 to 0.5 percent. In fact, postmenopausal women experience an increase in the loss of bone mass by as much as 10 times. Similarly, this increased rate also occurs in men after castration, when there is loss of function of the testicles.
Osteoporosis is known defined as having a low bone mass and the deterioration of bone tissue which leads to a high incidence of bone fracture for individuals. The likelihood of obtaining osteoporosis usually increases with age. The mechanism and rate for which older individuals lose bone, positively correlates with calcium deficiency (NIH, 2018).
There are two main types of osteoporosis; primary and secondary. Primary osteoporosis is caused by an age-related bone loss, typically occurring to men that are above the age of 70. Secondary osteoporosis is when bone mass is lost due to onset of certain diseases, bad lifestyle, etc. Some common causes of secondary osteoporosis include cigarette smoking, alcoholism, and low testosterone levels in men (NIH, 2018).
This calcium deficiency leads to secondary hyperparathyroidism; elevated PTH levels in the blood. This stimulates osteoclast activity within the bone resulting in more bone resorption than normal.
The reason for why osteoporosis is usually seen in older individuals is due to a couple of factors. Aging skin along with decreased sun exposure, reduces the conversion of a precursor of vitamin D (7-dehydrocholesterol) to Vitamin D3. Ultimately, this causes Vitamin D insufficiency which reduces the amount of calcium being absorbed (Kenny et al., 2000).
In females, menopause usually leads to the loss of bone mass. When menopause occurs, the hormone progesterone is deficient. Some supporting data from 1990 suggests that progesterone plays the role of being a bone formation-stimulating hormone. Although supported, nothing is concrete as this hormone regulated by estrogen, thereby including multiple confounding variables (Wark, 1993).
In males studies have been done linking bone mineral densities to testosterone levels. When comparing the estrogen level of males, the group of males with the highest levels had the highest bone mineral density, while the group of males with the lowest estrogen levels had the highest risk of a hip fracture. In contrast, when measuring levels of testosterone, there was no significant difference in hip fracture risk when looking at hypogonadal men versus eugonadal men. This supports the fact that the hormone estrogen plays more of a role in bone health in comparison to testosterone (Golds et al., 2017).
Treatments - Prevention & Management
Unfortunately, there is no cure for osteoporosis as it is a symptom from ageing, however there are many prevention and management methods to reduce its severity. Thus, the current treatment methods are targeted at preventing the progression of osteoporosis, which include changes to one's lifestyle and drugs that reduce bone loss, increase bone strength and bone formation (Kling, Clarke, & Sandhu, 2014).
Lifestyle
There are many lifestyle modifications that individuals can engage in to reduce the detriments of osteoporosis and prevent its progression. Since one component of bones is calcium, one recommendation is to include more foods rich in calcium in one’s diet. Some examples of calcium rich foods are dairy products like milk or yogurt, leafy dark green vegetables, nuts and calcium-fortified foods. Additionally, there are calcium supplements available like calcium citrate and calcium carbonate that an individual can take. Together, these foods and supplements will aid in building bone strength and reducing the progression of osteoporosis (NYU Langone Health, n.d.).
Another vitamin that will help in preventing osteoporosis from progressing is vitamin D. Similar to calcium, there are foods and supplements available that an individual with osteoporosis can take. Examples include fatty fish like tuna or salmon, beef liver, cheese and egg yolks, as well as vitamin D supplements one can obtain over the counter. That being said, vitamin D works by promoting calcium absorption in the intestines and aids in the maintenance of balanced calcium levels. Moreover, vitamin D supplements can be taken in combination with calcium rich foods or supplements to increase the efficiency of calcium absorption (NYU Langone Health, n.d.).
Lastly, a healthy and physically active lifestyle is highly recommended for someone with osteoporosis, especially exercises involving the use of small weight. Some examples of exercises individuals can partake in are dancing, walking, jump rope, hiking, and stair climbing. These exercises can aid in increasing bone strength and stimulating bone growth. In addition, health practitioners recommend that individuals suffering from osteoporosis should avoid smoking and consume no more than two alcoholic drinks per day as both decrease bone density and increase fracture risk (NYU Langone Health, n.d.).
Drugs and Medication
As of now, the most effective drugs for osteoporosis are antiresorptive agents, meaning they decrease the amount of calcium removed from bones. Since bones are dynamic and constantly being remodelled, and osteoporosis results when bone resorption is higher than bone rebuilding, these medications inhibit the removal of bone so bone rebuilding is favoured. Many antiresorptive agents are available including alendronate, risedronate, raloxifene and others (Lewiecki, 2004).
Bisphosphonates are a class of antiresorptive drugs that are used to decreases risks of fractures of hip, wrist, and spine. These class of drugs are all administered orally to reduce adverse side effects, and to enhance the absorption of the medicine. They are taken in the morning and are taken with water to increase absorption. They can also be administered intravenous to avoid possible stomach problems (Lewiecki, 2004).
Alendronate (Fosamax) is an example of a bisphosphonate drug. It is effective treatment for postmenopausal osteoporosis as well as with glucocorticoid induced osteoporosis. This drug, similar to other bisphosphonates increases bone density and reduces various possible fractures. It is taken orally once a week for postmenopausal osteoporosis and is also the first drug used for increasing bone density in males with osteoporosis. This drug as all others does have a few side effects. This includes irritation of the esophagus or even inflammation of the esophagus. Differences in the chemical makeups of the other bisphosphonate drugs is what allows for certain side effects to be avoided (Gronholz, 2008).
Zoledronate (Reclast) is an intravenous administered bisphosphonate that is given once a year. It is able to effectively strengthen bones along with preventing both spinal and non-spinal fractures. As with all medications, side effects of this drug may result in muscle and joint aches, and so mild pain killers are given following treatment. This drug is used mainly to prevent postmenopausal osteoporosis and to increase bone mass in males suffering the disease (Gronholz, 2008).
Conclusion
Osteoporosis is set to become a major health concern with an ageing population. Scientists have identified human stem cells that develop into the bone, cartilage, and other tissues that make up the body’s skeleton (Price et al., 2018). This will one day help doctors repair or replace joint cartilage, heal broken bones more quickly, and build up bone in osteoporosis patients. Additionally, a new genetic screen may predict a person’s future risk of osteoporosis and bone fracture and may allow for more preventative measures (University of Stanford, 2018).