This is an old revision of the document!
Table of Contents
Bipolar Disorder
Introduction
Bipolar disorder (BD) is also known as manic depression and is a mental illness that expresses extreme high and low moods. The onset of BD can also cause changes in sleep, energy, thinking and behaviour. Individuals who do suffer from BD experience periods where they feel very happy and energized and other periods where they feel very sad, hopeless, and down. There are times between these two phases where they feel normal. The highs and lows are like “poles” of mood, hence, “bipolar” disorder. The term “manic” are the times in which an individual would feel those “highs” of over excitement and confidence. Many times, these emotions can lead someone to making impulsive and reckless decisions. Sometimes, during the manic period, individuals can experience delusions, for example believing in things that aren’t true and it becomes hard to talk them out of these ideas, and hallucinations, like seeing or hearing things that aren’t there. Hypomania is a term used to describe mild symptoms of mania. During this time, an individual may not experience the delusions or hallucinations and their extreme high symptoms don’t stop them from completing everyday activities. Depressive phases are times when an individual feels very sad or depressed. Most people spend more time in the depressive phase rather than the hypomanic or manic phases (Bipolar Disorder, 2005).
Bipolar Disorder Type I & II
There are also two major classifications of BD which are known as Bipolar I disorder and Bipolar II disorder. BD I involve phases of extreme mood episodes ranging from mania to depression. BD II is a milder form of mood swings which consists milder episodes of hypomania and phases of extreme depression (Bipolar Disorder, 2005).
Cyclothymic Disorder
Cyclothymic disorder is classified as brief periods of hypomanic symptoms that can be described as short periods of depressive symptoms that aren’t as long-lasting that are expressed in hypomanic or depressive episodes (Bipolar Disorder, 2005).
Mixed Features
Mixed features is a term used when referring to simultaneous symptoms of opposite mood polarities during manic, hypomanic or depressive episodes. This can be identified as high energy, sleeplessness, and racing thoughts. However, at the exact same time, the individual the person may feel hopeless, despairing irritable, and suicidal (Bipolar Disorder, 2005).
Rapid-Cycling
Rapid-cycling is used to describe having four or more mood episodes within a 12-month time period. Episodes need to last for a certain number of days to be considered a distinct episode. Some individuals experience changes in polarity within a single week or even a day. In this case, this may be called ultra- rapid cycling, which can be argued in psychiatry that this isn’t a valid or well-established phenomenon in bipolar disorder. Rapid-cycling can happen at any time in the course of the disease, however, it is more prevalent later on in life and in the duration of the disease. This classification can increase the risk of severe depression and suicide attempts (Bipolar Disorder, 2005).
Diagnosis
The most important diagnostic method is to speak to a physician about the severity, length and frequency of changes in mood, lifestyle or behaviors. The physician bases the diagnosis on the severity of the symptoms as outlined by the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders or DSM-V. While making the diagnosis, the health practitioner will often ask questions about family history of bipolar disorder or other mental health illnesses since there is a genetic component to bipolar disorder (Bipolar Diagnosis, n.d.).
When speaking specifically about BD I and BD II there are specific criteria for the manic, hypomanic and depressed phases that need to be met in order to be diagnosed with one of the two mental illnesses. Criteria consist of the following:
Bipolar I: Manic
A. “A distinct period of abnormally and extreme mood and abnormally increase in activity or energy, lasting at least 1 week and present most of the day, nearly every day.
B. During the period of mood disturbance and increased energy or activity, three (or more) of the following symptoms:
· Inflated self-esteem or grandiosity.
· Decreased need for sleep (e.g., feels rested after only 3 hours of sleep).
· More talkative than usual or pressure to keep talking.
· Flight of ideas or subjective experience that thoughts are racing.
· Distractibility (i.e., attention too easily drawn to unimportant or irrelevant external stimuli), as reported or observed.
· Increase in goal-directed activity (either socially, at work or school, or sexually) or psychomotor agitation (i.e., purposeless non-goal-directed activity).
· Excessive involvement in activities that have a high potential for painful consequences (e.g., engaging in unrestrained buying sprees, sexual indiscretions, or foolish business investments).
C. The mood disturbance is severe enough to cause damage on social or occupational functioning
D. The episode is not attributable to the physiological effects of a substance or another medical condition (DSM fifth edition, n.a).”
Bipolar I: Hypomanic
Bipolar I: Depression
Bipolar II: Hypomanic
Bipolar II: Depression
Epidemiology
Societal Impact
Family Impact
Physiological Effects
Causes/Risk Factors
Symptoms
Pathophysiology
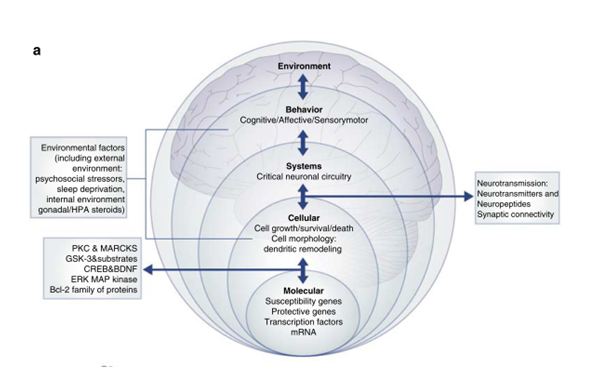
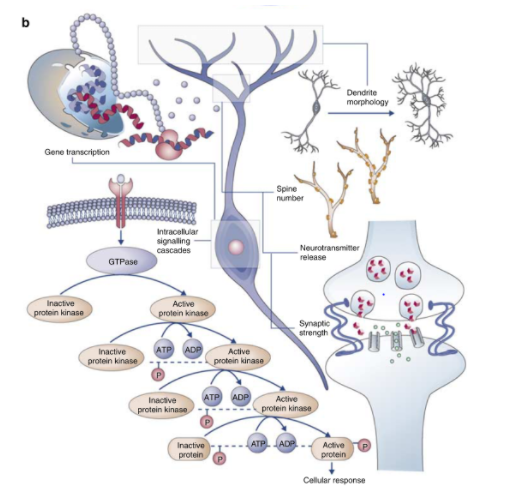
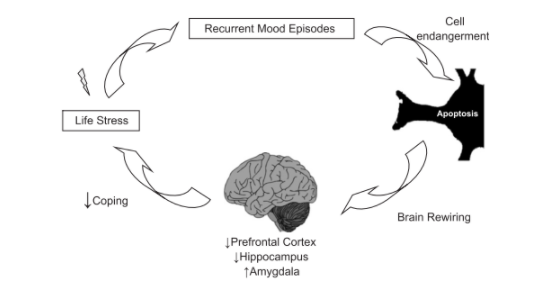
Abnormalities in the synaptic and cellular plasticity
Figure 3: Different physiological levels contributing to the pathophysiology of BD. Retrieved from Schloesser et al., 2008.
Figure 4: Cellular signaling cascades that regulate diverse physiologic functions have shown to be disrupted in patients with BD. Retrieved from Schloesser et al., 2008.
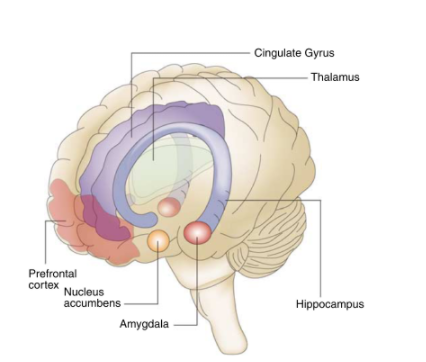
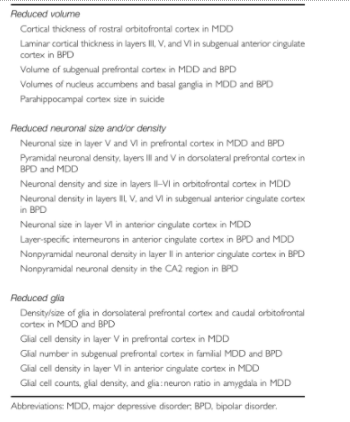
Structural Neuroimaging Findings
Figure 5: Neuroanatomical regions which are implicated in the perception and control of mood states and emotions are affected in patients with BD. Retrieved from Schloesser et al., 2008.
Table 1: Studies using post-mortem brains with mood disorders show cellular atrophy and/or loss. Retrieved from Schloesser et al., 2008.
Allostatic load in Bipolar Disorder
HPA axis and circadian rhythm disturbances
Amygdala and emotional processing
Prefrontal cortex and coping
Figure 6: The image summarizes the cycle of brain rewiring in patients with BD. Retrieved from Kapczinski et al., 2008.
Treatments
Types of Care
Primary and Secondary Care
When assessing the care that individuals with BD seek, the following statistical analyses provide key insight:
- ¾ of individuals with BD do not receive the optimal care
- ¼ of individuals with BD do not seek for primary/secondary care for issues pertaining to mood
Primary care attenders attend a large portion of individuals with BD, therefore this form of support allows for an effective form of detection and diagnosis. The diagnosis and treatment plan for patients can take up to 8 years for individuals to receive secondary care services. There is a great amount of misdiagnosis of BD due to the numerous consultants and care providers involved in the process of diagnosis. Primary caregivers are responsible for managing the physical and mental health care of individuals with BD, while ensuring that their own health is intact. BD can cause caregivers to develop depression and anxiety, therefore primary care must constantly be assessed and monitored (National Collaborating Centre for Mental Health, 2006).
Figure 7: Visual representation of diagnosis between a primary care attender, such a physician, and a BD patient. Retrieved from https://s.sharecare.com/img/video/stills/2538422639001_bipolar_treated.jpg
Self-management
It is imperative for individuals with BD to develop a systematic approach at managing their symptoms over a long-term. The ability to make informed decisions regarding their treatments allows individuals with BD to develop a stronger grasp and increased confidence in their ability to be independent. The extent to which these individuals take responsibility must be carefully monitored through coping mechanisms, as they may not understand the diagnosis completely, thus resulting in risky behaviour or abandoning the use of medications. Individuals with BD are able to monitor their moods by documenting it in a diary and assessing the triggers that onset manic or depressive episodes. An organization called ‘The BiPolar Organization’ provides individuals with BD and their caregivers self-management training programs in the UK. It is important to note that the optimal form of care comes from the collaborative approach of diagnosis, treatment and management through consultations between the patient, caregiver and medical professional (National Collaborating Centre for Mental Health, 2006).
Psychological Therapy
The primary goal of psychological therapy is to prevent and minimize relapses in mood swings for individuals with BD. Therapeutic techniques assess mood changes, coping mechanisms, enhance the effects of pharmacotherapy and ensure better communication within family members (National Collaborating Centre for Mental Health, 2006). Psychotherapy can be categorized into short-term and long-term treatments. Short-term therapies are led by the therapist and focus on current issues that the patient faces. Long-term therapy lasts for a year or longer, and the therapist minimizes their involvement in carrying out conversation. Instead, the patient seeks to understand underlying issues that they may have experienced in the past and/or presently. Current combination therapies consisting of psychological and medical treatments are most effective in preventing relapses for individuals who are out of acute episodes or for stable patients (Centre for Addiction and Mental Health, n.d.).
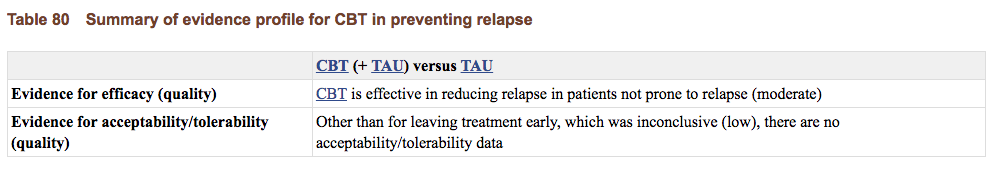
Cognitive Behavioural Therapy
This common form short-term psychotherapy is applicable to managing and treating numerous mental illnesses. Individuals with BD work with the therapist in identifying their thoughts, feelings, symptoms and areas of conflict. This part of CBT allows the individual to be cognizant of their mood transitions, thus allowing them to develop the necessary skills to assess, monitor and combat the manic and depressive states. The therapist and the patient are able to develop goals and design a management routine that is effective and pertains to the individual’s concerns and symptoms. In a RCT of 457 individuals between the ages of 39-52 diagnosed with Bipolar Disorder I or II were assessed for the effectiveness of CBT. An overall summary of evidence for CBT preventing relapse shows that CBT is effective in comparison to no psychological therapy. Furthermore, the addition of CBT to standard care practises was more effective than the care on its own, because individuals in the CBT group had significantly fewer acute bipolar episodes in comparison to the control group over 12 months and 30 months (National Collaborating Centre for Mental Health, 2006).
Figure 8: Results from RCT of CBT of individuals with BD show that CBT is effective in preventing relapses. Retrieved from National Collaborating Centre for Mental Health, 2006.
Group/Family Therapy
For individuals with BD, the environment in which they surround themselves in is crucial for managing their symptoms. In group and family therapy, issues that may have existed prior to the diagnosis of BD may be uncovered, thus allowing individuals to communicate and provide a strong support network. It is important for family members to be aware of and educated of the ways in which they should approach an acute episode. Peer support groups allow individuals with BD to share their experiences with one another, and ensure that they are not alone in this process towards coping positively. Members develop strong attachments to one another, as they are able to understand themselves through understanding each other (Centre for Addiction and Mental Health, n.d.).
Psychoeducation
Psychoeducation is a form of CBT that delivers modes of intervention to patients and their families for managing BD. It is important that psychoeducation is catered to the needs of each individual. Information can be given to the patients in a one-on-one basis or group basis, or to the families and caregivers. Psychoeducation can be presented in various forms, such as written work, audio, and video, to accommodate the patient’s needs (Smith, Jones, & Simpson, 2010).
Numerous RCTs that have been conducted within the last 10 years publish data that supports the theory that psychoeducation is effective for individuals with BD. In a study done by Colom et al. (2003), group psychoeducation sessions took place over the course of 21 sessions. Information pertaining to the illness, adhering to treatment, early detection of symptoms and recurrences of symptoms were discussed with the individuals. A control group with participants who took the same pharmacotherapy and psychiatric care were not presented with specific psychoeducational material. In comparison to the control group, individuals gaining educational support has fewer relapsed patients, a decreased number of recurring symptoms and increased time in the transition periods from depressive to manic to hypomanic stages (Colom et al., 2003).
Pharmacotherapy
Once a diagnosis has been made, the first line of treatment involves the use of pharmacological agents. Usually, effective treatments combine medication and psychotherapy due to the long term nature of this disease. Therefore, medications allow individuals to have symptomatic recovery. The goal is to essentially prevent relapse and enhance social and occupational functioning. Treatment of both phases of the illness can be extremely difficult because the same treatments that alleviate depression can exacerbate mania, hypomania or rapid cycling (Mayo Clinic, 2017).
Unfortunately due to our scarce knowledge of the disease mechanism and of pharmacological targets, there are few treatments that are truly effective for bipolar disorder. Most medications are based on an extension of use from other psychiatric disorders (Mayo Clinic, 2017). However, lithium is unique because its main therapeutic use is in bipolar disorder and its mechanism of action is an important place for the identification of future targets.
Additionally, it is important to understand that different types of medication help control different symptoms. That is why it is not uncommon for individuals to try various medicines to find the ones that work for them at the right dosages. Evidently, this can be very frustrating for patients.
Generally, there are three classifications of medications:
Mood Stabilizers
These are medicines that treat and prevent highs (manic or hypomanic episodes) and lows (depressive episodes). They also help to minimize the negative effects of mood fluctuations on functioning. Not all drugs have equal ‘anti-manic’ and antidepressant effects and their primary use is to treat full episodes of mania or depression, episodes that each can last for several days or weeks.
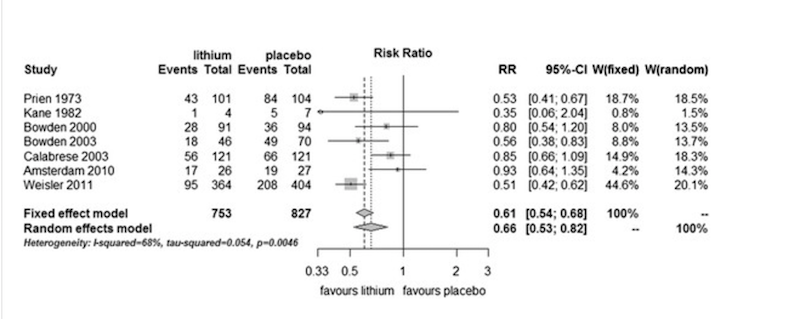
- Lithium
This is one the the oldest and least expensive mood-stabilizing drugs on the market. This drug is more effective at treating mania than depression. According to the literature, it is effective in reducing symptoms and frequency of episodes with a response rate of up to 70% to 80% for the initial manic phase of bipolar. However, it also requires regular blood test and monitoring for kidney and thyroid function. According to the APA, first line therapy is lithium with an anticonvulsant such as valproate (Mayo Clinic, 2017). To solidify the evidence supporting lithium use, a meta-analysis of randomized controlled trials comparing lithium with placebo as a long-term treatment in bipolar disorders was conducted. The study showed that lithium was more effective than placebo in preventing overall mood episodes , manic episodes, and dependent on the type of analyses applied, depressive episodes [Figure 9](Severus et al., 2014).
Figure 9: Prevention of any episodes in bipolar patients in RCTs comparing lithium with placebo. All trials show that placebo is inferior to lithium. Retrieved from: http://journalbipolardisorders.springeropen.com/articles/10.1186/s40345-014-0015-8
- Lamotrigine
This is classified as an anticonvulsant (or antiepileptic) and is more useful for depressive symptoms than manic. There are a variety of anticonvulsants on the market, as one does not work for everyone. Some common ones are: Carbamazepine (Tegratol), Lamotrigine (Lamictal) and Valproic acid (Depakote). Some of these medications also work for other psychiatric symptoms like anxiety, or binge eating (Mayo Clinic, 2017).
A meta-analysis of individual patient-level data from five trials of lamotrigine in bipolar depression reported a modest treatment effect, but one of the trials reviewed showed statistically significant benefits of treatment with lamotrigine in comparison with placebo. Therefore, the place of lamotrigine in acute treatment remains uncertain (Geddes, & Miklowitz, 2017).
Atypical Antipsychotics
These medications are used alone or in combination with other mood stabilizers in patients with bipolar mania. They can reduce or eliminate symptoms of psychosis, like delusions and hallucinations. They used to be referred to as major tranquilizers. They are the main class used to treat schizophrenia (“CAMH: Antipsychotic Medication”, 2017).
- Antipsychotic medications
These are used as a short-term treatment for bipolar disorder to control psychotic symptoms such as hallucinations, delusions, or mania symptoms. Commonly used medications include: haloperidol (haldol), loxapine (Loxitane) or risperidone (Risperdal). Newer drugs that have been added to this category are: aripiprazole (Abilify), asenapine (Saphris), cariprazine (Vraylar), olanzapine (Zyprexa) quetiapine fumarate (Seroquel), and ziprasidone (Geodon) (Mayo Clinic, 2017).
- Benxodiazepines
These are to help patients with acute mania and relieve insomnia.These drugs belong to a group of medications called central nervous system (CNS) depressants, which act on neurotransmitters to slow down normal brain function. CNS depressants are commonly used to treat anxiety and sleep disorders and are sometimes prescribed as adjunctive therapy with bipolar disorder.Benzodiazepines affect the neurotransmitter gamma-aminobutryic acid (GABA). By increasing GABA in the brain, these drugs have a sedative effect (“Benzodiazepines”, 2017).
Commonly used benzodiazepines include alprazolam (Xanax), clonazepam (Klonopin), diazepam (Valium), and lorazepam (Ativan). These drugs all carry the risk of being addictive (Mayo Clinic, 2017).
Antidepressants
These are controversial due to the fact that their effectiveness has not been proven yet are commonly prescribed to patients.
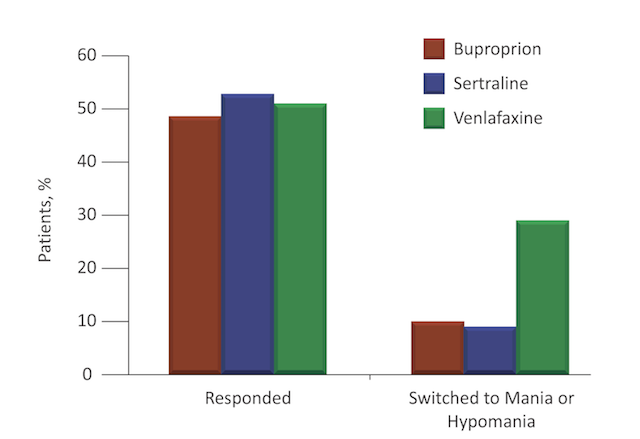
Earlier clinical trials suggested that when SSRIs (Selective Serotonin Reuptake Inhibitors) were given with antimony treatments, the SSRIs were more effective and more likely to induce mania than placebo. A study by Post et al. found that different antidepressants appear to have different propensities for triggering an affective switch, possibly because of their differing mechanisms of action. They found that the antidepressant venlafaxine, conferred the greatest risk (Post et al., 2006) [Figure 10]. Essentially, no antidepressant is proven to be effective in bipolar depression but it seems to work for some patients but not others (Mayo Clinic, 2017).
Figure 10: Response and Manic/Hypomanic switch rates for different antidepressants. Retrieved from: http://www.cmeinstitute.com/psychlopedia/Pages/bipolardisorder/9iddt/sec3/section.aspx
Antidepressants used in the treatment of bipolar depression include bupropion (Wellbutrin), fluoxetine (Prozac), and sertraline (Zoloft). Side effects for these medications include: nausea, tremors, sexual dysfunction, weight gain and liver failure. Regular monitoring of these individuals is recommended but the side effects subside in a few weeks (Mayo Clinic, 2017).