Table of Contents
Seasonal Affective Disorder
Seasonal Affective Disorder (SAD) is classified as a sub-type of Major Depressive Disorder which is primarily related to the changing seasons. The onset of SAD varies predictably over the course of the year; usually during the fall and winter months and less rarely in spring and summer. The reduced level of sunlight in the fall and winter seasons has been highly associated with SAD which essentially disrupts the body's internal clock and lead to feelings of depression. Changes in levels of neurotransmitters such as Serotonin and Melatonin also affect the mood and sleep patterns of the affected individual (Winkler et al., 2006).
Signs & Symptoms
The nature and severity of SAD varies from person to person. The symptoms usually start in the autumn or winter and tend to improve in the spring. The classic symptoms of SAD include oversleeping, daytime fatigue, carbohydrate craving, and weight gain (Burgo, 2014).
- Oversleeping: People with SAD tend to feel the need to sleep more during the wintertime.
- Daytime Fatigue: Individuals with SAD often lack energy and motivation and feel hopeless and agitated. They feel depressed most of the day, lose interest in daily activities and have a greater tendency of nodding off at work.
- Carbohydrate Craving: SAD can produce a strong craving for complex carbohydrates such as bread and pasta which eventually causes the levels of an amino acid, tryptophan to rise in the brain. This in turn causes the release of serotonin, which boosts mood. In effect, people with SAD use carbohydrates as a kind of medication—and a bigger waistline is a common side effect.
- Weight Gain: Like depression in general, SAD increases appetite in most people. Sixty-five percent of people with the disorder report being hungrier during the colder, darker months. This voracious appetite is speculated to be a biological response to a seasonal drop in serotonin, a neurotransmitter that’s associated with mood and helps to control hunger. The increased appetite and a higher carbohydrate consumption often lead to weight gain in most individuals.
Some people may also experience other symptoms of depression including decreased sexual desire, lethargy, hopelessness, suicidal thoughts, and lack of interest in normal activities or social interactions. Most importantly, unlike Major Depressive Disorder, the symptoms of SAD come and go with the change in seasons (Winkler et al., 2006).
Epidemiology
Community-based studies approximate the prevalence of SAD to be about 10% in northern latitudes (Kurlansik & Ibay, 2013). If the application criteria are followed using the DSM-IV-TR, the prevalence of SAD in the United States is estimated to be about 1-2%, while it is around 2% in Canada (Rohan et al., 2009). The incidence of SAD increases in populations that live further north as shown using studies involving populations in Alaska and areas close the Artic. A study conducted by Rosen et al. (2002) found that the prevalence of SAD in a group of U.S Army soldiers was found to be 6.5% and 13.1% in women and men respectively. Seasonal affective disorder affects women more than males as it is observed that the ratio of women to men who have SAD is 4:1 (Jepsen et al., 1999).It is difficult to determine SAD prevalence as often people will not report the symptoms they are experiencing, and thus the disorder goes undiagnosed.
Epidemiology of SAD is studied using diagnostic research tools such as the Seasonal Pattern Questionnaire (SPAQ) and the Structured Interview Guide for the Hamilton Depression Rating- Seasonal Affective Disorder (SIGH-SAD). SIGH-SAD helps determine whether the affected individual suffers from SAD or sub-syndromal SAD (S-SAD). Patients with S-SAD suffer from milder seasonal affective symptoms. A new diagnostic tool called the Seasonal Health Questionnaire (SHQ) was compared against SPAQ in a study in the United Kingdom involving 809 patients. Researchers found that the SQH method was found to be more sensitive and specific to diagnose patients with SAD. The SPAQ method had a SAD prevalence of 10. 7% compared to SHQ, which had an incidence of 5. 6% (Thompson et al., 2004).
Risk Factors
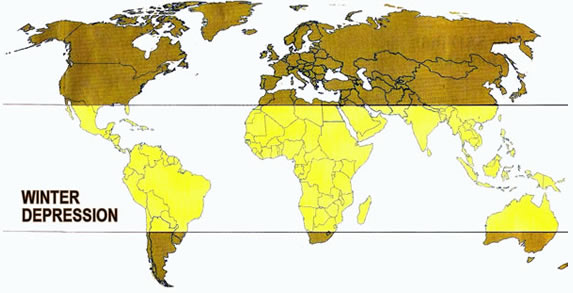
People who live in areas further away from the equator experience a greater risk of developing SAD especially those in the northern latitudes as shown in Figure 1. In the United States, SAD occurs in about 1% of the population but rises to about 9% in people living in Alaska (Horowitz,, 2008).. Those who have limited exposure to sunlight in their workplace such as those who do shift work face a greater risk of SAD (Melrose, 2015). Individuals who move from southern latitudes to northern areas face an increased risk of SAD development. Researchers in Maine used SPAQ, and the Beck Depression Inventory study the incidence rate of SAD and S-SAD in 76 college students. SAD rates were found to be 13.2%, and researchers speculated that the students who had moved to Maine from lower latitudes were more likely to experience winter depression compared to those who were native to New England (Low & Fessiner, 1998).
Miller (2005) described the idea of a latitude theory to explain the incidence of SAD. The theory asserts that reduced sunlight exposure in the winter months in northern climates increases an individual’s risk of SAD. However, Magnusson and Axelsson discerned that Icelandic people possibly had a genetic adaptation to low light in winter. The prevalence of SAD in native Icelandic and Canadian Icelandic individuals was found to be less than other populations (Magnusson & Axelsson, 1993). SAD typically occurs more frequently in individuals who have relatives who have experienced SAD. Thus a study by Madden et al. (1996) found that in 3, 331 Australian twins, genetic effects were involved in 29 of the observed variance in seasonality. SAD is seen more often in younger adults as the estimated onset is thought to be between the ages of 18 and 30 years (Melrose, 2015).
Pathophysiology
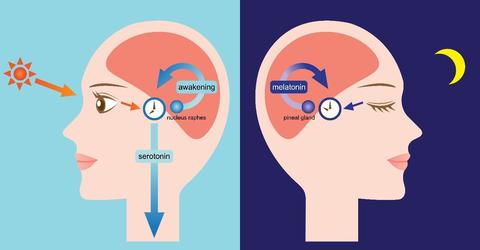
Seasonal affective disorder (SAD) primarily revolves around circadian rhythms. These are also known as the body’s intrinsic clock. In its simplest form, circadian rhythms deal with wake and sleep cycles. In the daytime, light is detected via photoreceptors in our eye (Hornung, 2003). These photoreceptors send neural signal to the brainstem via the retina. In the brainstem, there are structures referred to as the dorsal and medial nucleus raphe (Hornung, 2003). Within this nuclei, there is a cluster of serotonergic neurons (Hornung, 2003). With light stimuli, these neurons fire and increase the release of serotonin. This process can be observed on the left hand of Figure 2. Serotonin is associated with waking periods.
In the night, there is an absence of light. This absence is noted due to a lack of stimuli sent to photoreceptors within the eye (Benarroch, 2008). The lack of light is also recognized by the hypothalamus. Within the hypothalamus, there is a structure referred to as the suprachiasmatic nuclei (SCN) (Benarroch, 2008). The SCN regulates the secretion of melatonin via the pineal gland (Benarroch, 2008). This process can be observed on the right hand of Figure 2. Melatonin is secreted at high levels during sleep periods.
<style center>
</style>
Photoperiod and Melatonin
As previously noted, light suppresses melatonin secretion (Lam & Levietan, 2000). With light stimuli, the SCN will inhibit melatonin secretion from the pineal gland. As indicated in Figure 2, this implies a lack of melatonin secretion during daily activities and surge during sleep periods. A wide variety of research associates abnormal melatonin secretion with SAD patients. The exact causal mechanism behind this phenomenon still requires further research (Lam & Levietan, 2000).
Circadian Phase Shift
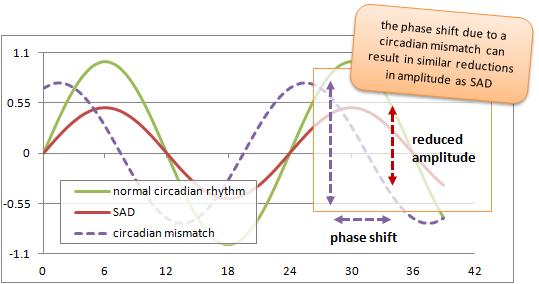
Light is the most significant factor associated with circadian rhythms. Often, a patient with SAD will note that their normal circadian rhythm is mismatched due to changing external factors such as, sunlight (Lam & Levietan, 2000). This is noted in the graph below as a phase shift (this is shown in purple - a shift between the natural and social clock of individuals) (Moussa, 2012). Moreover, there is also a shortening in the overall time length of circadian rhythms (noted as a decreased amplitude within the graph) (Moussa, 2012). As a result, it is hypothesized that the timing of the light cycle can dictate the magnitude of the circadian rhythm phase shift (Lam & Levietan, 2000).
<style center>
</style>
The Role of Neurotransmitters and SAD
A number of neurotransmitters have been associated with SAD. These neurotransmitters are referred to as monoamines (Lambert, Reid, Kaye, Jennings, & Esler, 2002). Due to their overlapping function, many of these neurotransmitters interact throughout the manifestation of SAD (Lambert et al., 2002).
Serotonin is a neurotransmitter mainly associated with mood regulation, waking cycles, appetite/digestion, memory and sexual desire (Hornung, 2003). The association between Serotonin and feeding behavior explains the increase of carb intake within SAD patients (Lam & Levietan, 2000). Serotonin (also referred to as, 5-hydroxytryptamine: 5-HT) activity fluctuates with seasons. Serotonin levels are lowest during the winter months such as, December and January. The metabolite of serotonin, 5-HIAA is also noted to be expressed in low levels during the spring. This further implies low serotonergic activity in the winter (Lam & Levietan, 2000). Within SAD patients, there are dysfunctional 5-HT (serotonin) receptors - indicating abnormally low baseline levels of serotonin (Hornung, 2003).
Norepinephrine, a catecholamine, accounts for the depressive symptoms of SAD (Lambert et al., 2002). Typically, norepinephrine functions as a stress hormone to regulate physiological functions such as heart rate and breathing rate (Lambert et al., 2002). Within SAD patients, norepinephrine is associated with hypersomnia (increased sleep) and increased eating (Lam & Levietan, 2000). This is believed to be attributed to the overall lower baseline level of norepinephrine within SAD patients (Lam & Levietan, 2000).
Last but not least, dopamine is a hormone also associated with SAD (Partonen, 1996). Typically, dopamine is associated with movement and reward-seeking behavior. In SAD patients, low prolactin levels have been noted. This indicates low functional activity of dopamine (dopamine regulates prolactin production). Low functional activity of dopamine (within SAD patients) is noted throughout all seasons. This is also manifested as decreased eye-blink rates within SAD patients (Partonen, 1996).
Genetics
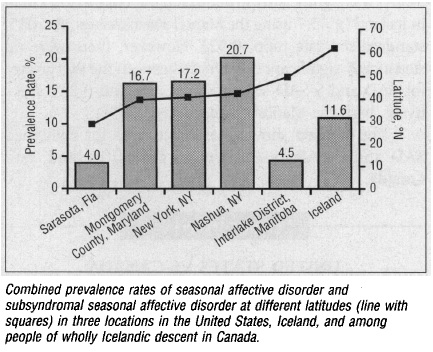
In one study, rates of SAD in native Icelanders (living in Iceland) were compared to native Icelanders who emigrated to Manitoba, Canada (Magnusson & Axelsson, 1993). Both populations had low rates of SAD. They also compared both native Icelandic populations (emigrated and non-emigrated) to individuals living along the east coast of the United States. Despite the fact all populations live in northern latitudes, individuals living across the east coast of the United States had higher rates of SAD. The implied genetic basis of SAD in Icelandic individuals is depicted on the graph below. It should be noted that the graph also shows SAD rates within Sarasota, Florida. This is a “control” because SAD rates are expected to be low within this location (With decreased latitude, there is more sunlight) (Magnusson & Axelsson, 1993).
<style center>
SAD Rates Amongst Icelandic Natives and Americans
Figure 4: SAD rates are significantly lower in Icelandic native populations (those living in Iceland and those who emigrated to Canada) compared to those along the east coast of the United States. The population living in Sarasota, Florida serves as a control. (Magnusson & Axelsson, 1993)
</style>
In another study, genetic effects of SAD were analyzed amongst twin pairs (Madden, Heath, Rosenthal, & Martin, 1996). In the largest study of SAD, 4639 twin pairs living in Australia filled a self-report questionnaire relative to SAD. The study noted a 29% genetic variance in SAD depressive symptoms (ex. Food intake, sleep, weight gain). This implies an interplay of genetic and environmental factors related to SAD (Madden et al., 1996).
Diagnosis
Seasonal affective disorder can be difficult to diagnose because it is very similar to other depression symptoms. The first ever diagnosis criteria in the DSM was made by psychiatrist, Dr. Rosenthal, to explain what winter seasonal affective disorder is (Rosenthal et al, 1984). However there have been revisions made and implemented in the DSM-IV. It is important to note that SAD does not have a unique diagnostic criteria. SAD is known as a specifier of recurrent major depressive episodes (Westrin & Lam, 2007). The most important factor of diagnosing SAD is to determine the time of onset and offset of depressive episodes and additional symptoms and to make sure that patients have full remission in the summer. Most individuals who experience non-seasonal depression such as chronic major depressive disorder (MDD) experience a worsening effect on their depressive symptoms during the winter but this can be differentiated from individuals with SAD because those patients with MDD will be symptomatic in the summer, whereas SAD individuals will not be (Westrin & Lam, 2007).
Criteria for Seasonal Pattern Specifier: (Reid & Wise, 1995)
A. Regular temporal relationship between the onset of major depressive episodes and a particular time of the year (unrelated to obvious season-related psychosocial stressors)
B. Full remissions (or a change from depression to mania or hypomania) also occur at a characteristic time of the year
C. Two major depressive episodes meeting criteria A and B in last two years and no nonseasonal episodes in the same period This means is that an individual can be diagnosed with SAD only if they have experienced depressive episodes that happen for two consecutive winters. However, this criterion is debated on because there isn’t enough evidence to support that it is indeed SAD. Psychosocial stressors must also be taken into account during the winter. People are stressed out because of holidays so they may go into a depression.
D. Seasonal major depressive episodes substantially outnumber the nonseasonal episodes over the individual's lifetime
Treatments
Phototherapy
Phototherapy is a type of bright-light therapy that is administered to patients with SAD, especially in the winter. Exposure to natural or artificial light suppresses the brain’s secretion of melatonin. The eyes are exposed to atleast 2500 lx of artificial visible light at eye level (distance of about 1 meter) first thing in the morning (Terman et al., 1989). This light is emitted in high intensity through specially designed light boxes. To give an estimate, there is around 100 lx in a house, 2000 lx outside on a rainy winter day or 10,000 lx in direct sunshine (Partonen, 1998). Patients receive daily administration of bright light therapy usually in their own homes (Terman et al., 1989). Generally, higher intensities and shorter exposures yielded best response rates. A patient shows response to this treatment within 1-2 weeks and after this point, exposure is maintained for 5 times a week for the duration of winter. Side effects of this treatment can include eyestrain and headaches, but they are usually not serious (Partonen, 1998).
Drug Therapies
Drug Therapies Antidepressants may be given to treat SAD. The antidepressant drugs administered for SAD include sertraline, fluoxetine and moclobemide, which are selective serotonin-reuptake inhibitors (SSRIs). Some studies suggest that since tryptophan is a precursor for serotonin and melatonin, it may be beneficial in conjunction with phototherapy (Rodin and Thompson, 1997)
Psychotherapy
Preliminary research suggests that cognitive behavioral therapy can be useful in improving cognitive and behavioral for individuals with seasonal affective disorder. This type of therapy aids in changing patients’ automatic thoughts, dysfunctional attitudes, withdrawal and rumination. CBT is also effective in preventing relapse since the effects of CBT persist even beyond formal sessions (Rohan et al., 2004).
Combined Treatment
Phototherapy, psychotherapy and drug therapies can be combined, but there remains the risk of over arousal. Combined treatment is ideal for patients who have no response to phototherapy or drug therapy alone (Rodin and Thompson, 1997).
Other Therapies/Prevention
- Aerobic exercise
- Sleep deprivation
- Increase the amount of light at home
- Meditation
- Stress management
- Relocate to area with more sun
Conclusion
Light therapy and antidepressants are the main lines of treatment for seasonal affective disorder. However, one of the best ways to deal with seasonal affective disorder is through preventative strategies by implementing therapies (such as light therapy) before the onset of symptoms. An interesting way of preventing the development of SAD symptoms is through virtual reality systems (Medeiros, 2017). We know that individuals who suffer from SAD not only face mental deterioration but they are also physically affected during the dark, gloomy days of winter months and one idea has been proposed and that is through the world of science and technology. It is by using virtual reality light therapy. VR would emulate the summer and expose the individual to warm, sunny tropical weather without the effect of harmful UV sun radiation (Medeiros, 2017). This could potentially improve and boost an individual’s mental health and reduce the effects of SAD during the winter.
Overview of Seasonal Affective Disorder
Presentation
group_5_presentation_3_-_seasonal_affective_disorder.pptx group_5_presentation_3_seasonal_affective_disorder.pdf
References
Benarroch, E.E. (2008). Suprachiasmatic nucleus and melatonin. Neurology, 71(8), 594-598. http://dx.doi.org/10.1212/01.wnl.0000324283.57261.37.
Burgo, J. (2014). Treating Seasonal Affective Disorder: How to Face Winter with a Smile. After Psychotherapy and Psychology Today. Retrieved from https://www.fix.com/blog/treating-seasonal-affective-disorder/
Hornung, J.P. (2003). The human raphe nuclei and the serotonergic system. Journal of Chemical Neuroanatomy, 26(4), 331-343. https://www.ncbi.nlm.nih.gov/pubmed/14729135.
Horowitz, S. (2008). Shedding light on seasonal affective disorder. Alternative and Complementary Therapies, 14(6), 282-287.
Jepson, Tracy L., Michael E. Ernst, and Michael W. Kelly. “Current perspectives on the management of seasonal affective disorder.” Journal of the American Pharmaceutical Association (Washington, DC: 1996) 39, no. 6 (1998): 822-9.
Kraft, U. (2005). Seasonal affective disorder- the winter blues- can be lifted with bright light, as long as treatment time properly. The Scientific American, 16, No.3. Retrieved from http://www.federaljack.com/ebooks/Consciousness%20Books%20Collection/SciAm%20Mind%2016.3%20-%20The%20Chaos%20of%20Consciousness.pdf
Kurlansik, S. L., & Ibay, A. D. (2013). Seasonal affective disorder. Indian Jour. of Clinical Practice, 24.
Lam, R.W. & Levitan, R.D. (2000). Pathophysiology of seasonal affective disorder: A review. Journal of Psychiatry & Neuroscience, 25(5), 469-480. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1408021/pdf/jpn00088-0055.pdf.
Lambert, G.W., Reid, C., Kaye, D.M., Jennings, G.L., & Esler, M.D. (2002). Effect of sunlight and season on serotonin turnover in the brain. The Lancet, 360(9348), 1840-1842. http://dx.doi.org/10.1016/S0140-6736(02)11737-5.
Low, K. G., & Feissner, J. M. (1998). Seasonal affective disorder in college students: prevalence and latitude. Journal of American College Health, 47(3), 135-137.
Madden, P.A., Heath, A.C., Rosenthal, N.E., & Martin, N.G. (1996). Seasonal changes in mood and behavior. The role of genetic factors. Archives of General Psychiatry, 53(1), 47-55. https://www.ncbi.nlm.nih.gov/pubmed/8540777.
Magnusson, A. & Axelsson, J. (1993). The prevalence of seasonal affective disorder is low among descendants of Icelandic emigrants in Canada. Archives of General Psychiatry, 50(12), 941-946. https://www.ncbi.nlm.nih.gov/pubmed/8250680.
Mayoclinic. (2017). Seasonal Affective Disorder. Mayoclinic Health Newsletter. Retrieved from http://www.mayoclinic.org/diseases-conditions/seasonal-affective-disorder/basics/definition/con-20021047
Medeiros, D.M. (2017) Your VR Health Report. VR Fitness Insider. Retrieved from http://www.vrfitnessinsider.com/your-vr-health-report/
Melrose, S. (2015). Seasonal affective disorder: an overview of assessment and treatment approaches. Depression research and treatment, 2015.
Moussa, A. (2012, Aug 12). Circadian Rhythmicity. Retrieved from http://suppversity.blogspot.ca/2012/08/circadian-rhythmicity-sunlight-la-carte.html.
Partonen, T. (1996). Dopamine and circadian rhythms in seasonal affective disorder. Medical Hypotheses, 47(3), 191-192. https://www.ncbi.nlm.nih.gov/pubmed/8898318.
Partonen, T. (1998). Seasonal affective disorder. The Lancet, 352(9137): 1369-1374.
Puniewska, M. (2016, Nov 4). 10 Things you didn’t know about your circadian rhythm. Retrieved from http://www.prevention.com/health/10-things-you-didnt-know-about-your-circadian-rhythm.
Reid, W. H., & Wise, M. G. (1995). DSM-IV training guide. Psychology Press.
Rodin, I. and Thompson, C. (1997) Seasonal Affective Disorder. Advances in Psychiatric Treatment, 3: 352-359.
Rohan et al. (2004). Cognitive-behavioral therapy, light therapy, and their combination in treating seasonal affective disorder. Journal of Affective Disorders, 80: 273-283.
Rosen, L. (2002). Prevalence of seasonal affective disorder among US Army soliders in Alaska. Military medicine, 167(7), 581.
Rosenthal, N. E., Sack, D. A., Gillin, J. C., Lewy, A. J., Goodwin, F. K., Davenport, Y., … & Wehr, T. A. (1984). Seasonal affective disorder: a description of the syndrome and preliminary findings with light therapy. Archives of general psychiatry, 41(1), 72-80.
Terman et al. (1989). Light Therapy for Seasonal Affective Disorder: A Review of Efficacy. Neuropsychopharmacology, 2(1): 1-22.
Thompson, C., Thompson, S., & Smith, R. (2004). Prevalence of seasonal affective disorder in primary care; a comparison of the seasonal health questionnaire and the seasonal pattern assessment questionnaire. Journal of affective disorders, 78(3), 219-226.
Winkler, D., Pjrek, E., Iwaki, R., & Kasper, S. (2006). Treatment of seasonal affective disorder. Expert review of neurotherapeutics, 6(7), 1039-1048.