This is an old revision of the document!
Table of Contents
CHRONIC MYELOID LEUKEMIA
Introduction
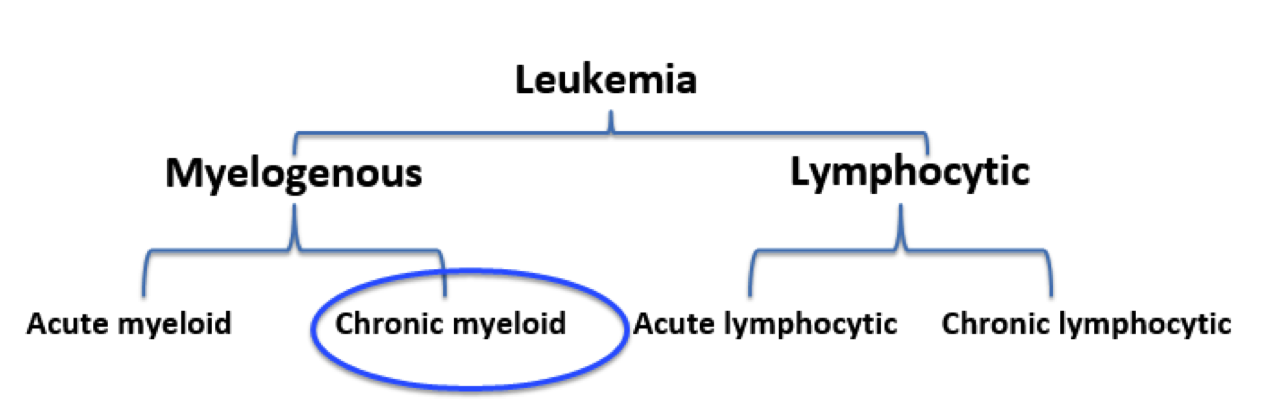
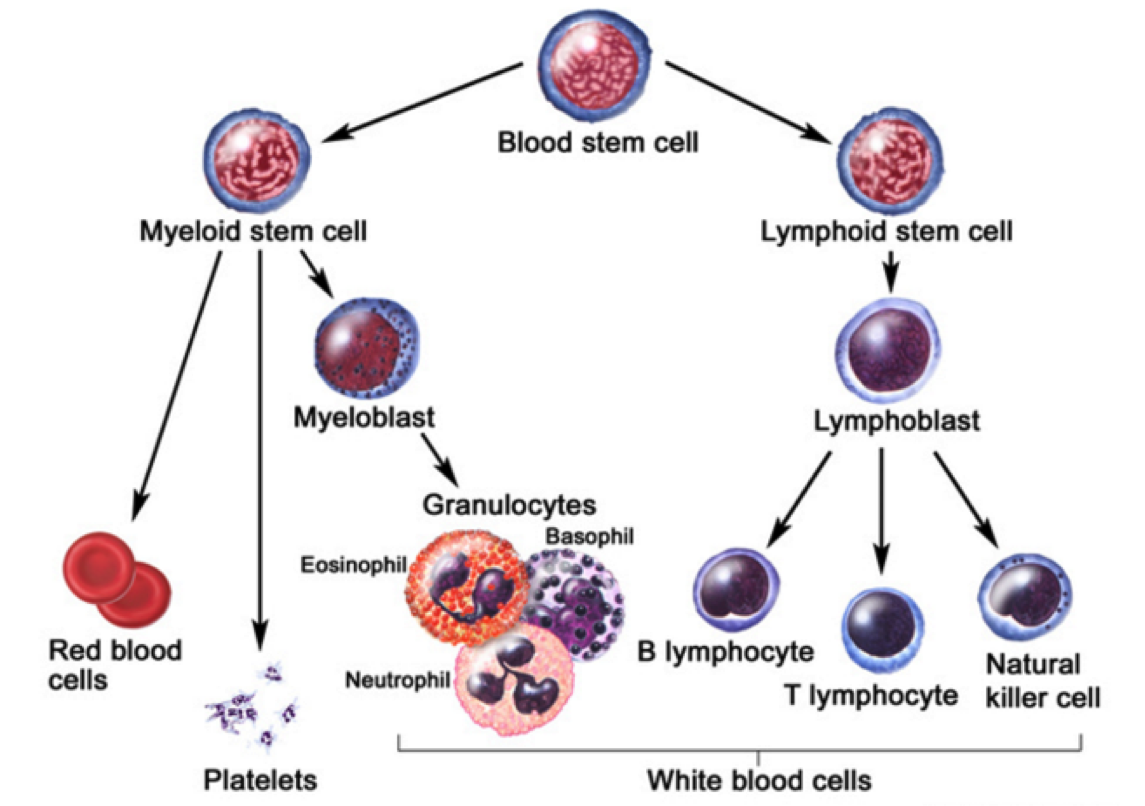
Leukemia is the eleventh-most prevalent cancer worldwide, with over 350,000 patients diagnosed each year worldwide (Siegel, Miller, & Jemal, 2015). Leukemia can generally be defined as a non-tumorous cancer of the blood, developing exclusively in the bone marrow of an individual (Apperley, 2015). It is at this stage where leukemia is further classified into varying types. The first distinction made for diagnosed patients is whether the leukemia is myelogenous or lymphocytic (Apperley, 2015). While lymphocytic leukemia occurs specific to blood stem cells predetermined to differentiate into lymphocytes, myelogenous leukemia targets blood stem cells destined to produce red blood cells (RBCs) and platelets (Vardiman et al., 2009). Both lymphocytic and myelogenous leukemia can also be sub-classified into acute and chronic leukemia. Acute leukemia patients display a rapid increase in immature myeloid or lymphocytic cells while chronic leukemia patients display increased numbers of more relatively mature cells (Vardiman et al., 2009). Based on the unique characteristics displayed by both acute and chronic leukemia, acute patients require a more immediate response to the disease.
The most notable characteristic of CML patients is the increased growth of myeloid cells which are unregulated can be observed in the bone marrow (Pui et al., 1989). This highly-proliferated stem cell fails to differentiate into its intended functional cell, thus failing to produce red blood cells and platelets required by the body (Deininger, Goldman, & Melo, 2000). The abundancy of myeloid cells in leukemic patients result in an accumulation within the individual’s bloodstream.
Risk Factors, Diagnosis, Signs and Symptoms
Notable risk factors associated with CML include age, gender, and exposure to radiation. The average recorded age of a CML patient is 65 years, implying that individuals are more prone to CML at an older age (Siegel, Miller, & Jemal, 2015). Recent studies also suggest men having a higher genetic predisposition to CML as opposed to their female counterparts (Siegel, Miller, & Jemal, 2015). In addition, individuals that have been exposed to high dosages of radiation throughout their lifetime have also been contingent with the disease.
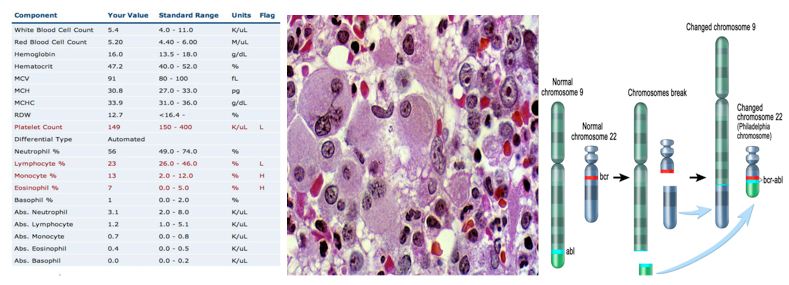
Clinical diagnosis of CML include various methods of approach. The most prevalent method of diagnosis is a complete blood count (CBC) of an individual. An increased level of granulocytes revealed during a CBC is indicative of CML, thus requiring further testing to verify the cause (Deininger, Goldman, & Melo, 2000). A more invasive study requires a bone marrow biopsy, which helps identify CML by gathering physical data at the locus of the disease. A less common, but more in-depth approach includes a genetic screening of the patient in order to display the source of the disease on a chromosomal level (Deininger, Goldman, & Melo, 2000).
In contrast to acute leukemia, which can be observed within days or weeks, the onset of symptoms cannot be observed in the early stages of the disease (Pui et al., 1989). The development of disease is very gradual in nature, thus making the diagnosis of CML occur in its later stages. CML is usually diagnosed during routine blood tests which later reveal an elevated white blood cell count. The physiological impact of CML primarily results in the lack of both RBCs and platelet count. Symptoms contingent to a lack of RBCs include both fatigue and anemia whereas a low platelet count is associated with widespread bleeding or bruising, frequent infections, bone pain, and weight loss due to loss of appetite (Baccarani et al., 2009).
Pathogenesis
Pathophysiology
Therapeutics
Options:
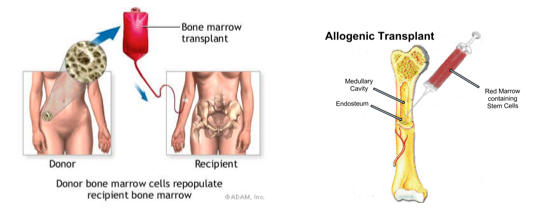
The only truly curative treatment is bone marrow transplant or allogeneic stem cell transplant. However, these treatments can be invasive and hence other treatment options include tyrosine kinase inhibitors.
Inhibiting Bcr-Abl as a potential drug target:
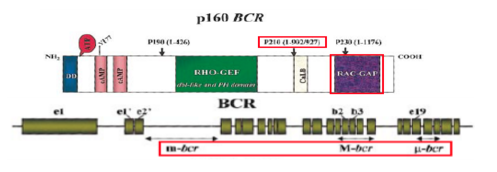
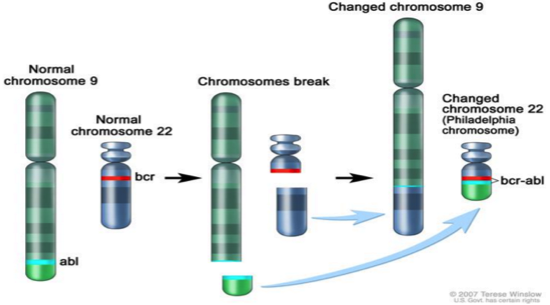
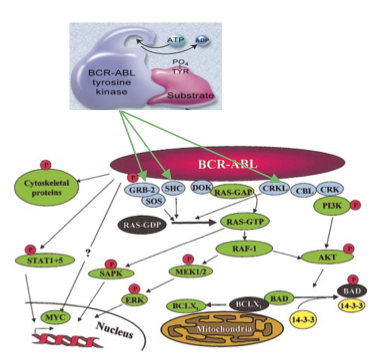
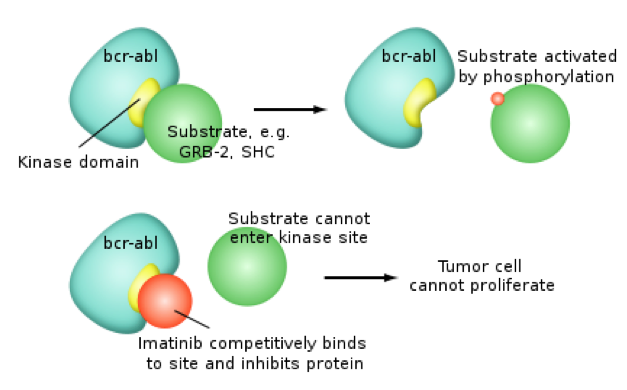
CML is caused by the reciprocal translocation between chromosome 9 (location of Abl1 gene) and 22 (location of BCR gene) which creates the Philadelphia chromosome. This molecular pathogenesis generates the Bcr-Abl fusion protein which has elevated tyrosine kinase activity. The Bcr-Abl fusion protein is found predominately in CML cells and thus provides the desired specificity (minimized systemic toxicity) for an inhibitor or therapeutic to interfere with this fusion protein’s function (Deininger, Goldman, Melo 2000). It is easy to target the ATP pocket of this fusion protein (something common to kinase proteins) than other protein-protein interactions as ATP pockets are well defined and mimicking ATP is an easy starting point for drug development (Deininger, Goldman, Melo 2000).
There are two conformation of Bcr-Abl that can be inhibited, the active and inactive conformation (Reddy and Aggarwal 2014). The open or active conformer is an active kinase in which ATP can bind. The kinase can use ATP to activate downstream proteins through phosphorylation. A possible inhibitor, and hence therapeutic for CML, would be an ATP mimetic of the open/active conformation. The second conformation is the closed/inactive conformation which is an inactive kinase in which ATP cannot bind and hence no downstream phosphorylation occurs (Reddy and Aggarwal 2014). It is harder to design an inhibitor/therapeutic for the closed conformer as the ATP pocket is not exposed.
Gleevec: a tyrosine kinase inhibitor
Gleevec (imatinib mesylate) is a therapeutic that was FDA approved for CML treatment in 2001. It is now used to treat gastrointestinal stroll tumours (Pray, 2008). Though at first the rationale was that Gleevec would compete with ATP in the active Bcr-Abl conformer, however that wasn't the case. Gleevec doesn’t compete with ATP, instead it just keeps the kinase in a closed state preventing ATP from binding to the conformer. There has been vast improvement seen for CML patient survival over other therapeutics. However, there is acquired drug resistance seen too. Drug resistance is common for chemotherapies due to prolonged exposure to drugs. In particular, some CML cell populations survive due to a genetic mutation in Bcr-Abl, giving rise to a new population of Bcr-Abl CML cells that are resistant to Gleevec. This mutation is at Thr315Ile location and it pushed Gleevec out of its pocket (Pray, 2008).
Results from tyrosine kinase inhibitors:
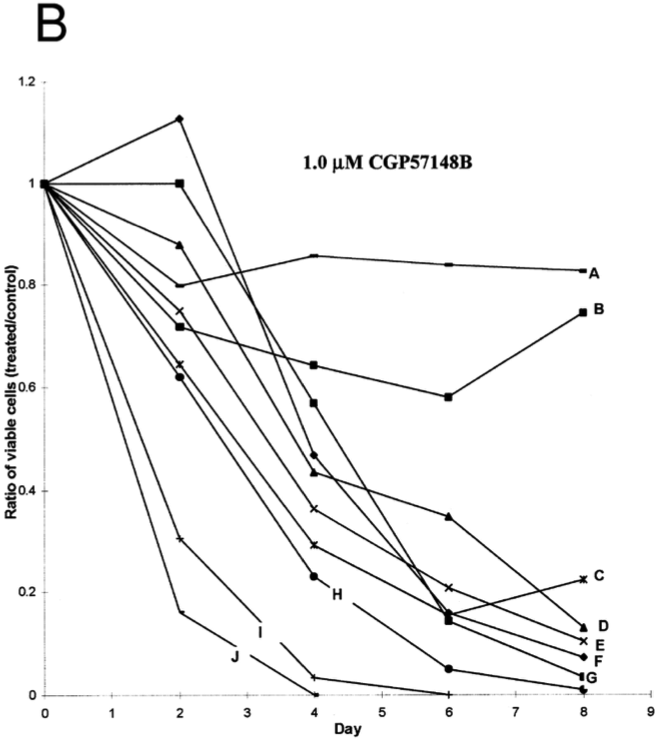
In the study by Deininger, Goldman, Lydon and Melo (1997), Bcr-Abl positive CML cells were exposed to tyrosine kinase inhibitor CGP57148B. Of all the cell lines examined, most showed a drastic reduction showing that tyrosine kinase inhibitors were effective in treating CML cells. Two cells that were resistant to the initial 1.0uM were treated with 10uM of the inhibitor.
Implications of treatment:
One strategy to overcome resistance is to develop new inhibitors of Bcr-Abl. For example, Dasatinib inhibits most Bcr-Abl mutants, except for the Thr351Ile mutant. Also Ponatinib is able to inhibit the T35I mutant (Shah, Tran, Lee, Chen, Norris, Sawyers 2004).
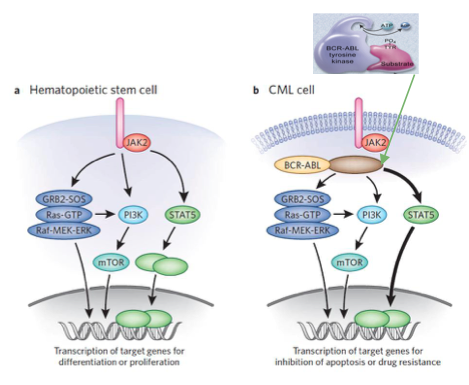
Numerous substrates and signaling pathways found to be influenced by Bcr-Abl. The result of this includes increased proliferation or decreased apoptosis of HSCs or progenitor cells. For example, Bcr-Abl constitutively phosphorylates STAT5, leading to transcription of target genes for proliferation/inhibition of apoptosis. As a result, this maintains CML. Finding inhibitors of the the STAT5 pathway is another possible alternative target for CML treatment (Cumaraswamy et al. 2014).
Conclusion
References
Apperley, J. (2015). Chronic myeloid leukaemia. The Lancet. 385: 9976, 1447–1459
Baccarani, M., Cortes, J., Pane, F., Niederwieser, D., Saglio, G., Apperley, J., & Hochhaus, A. (2009). Chronic myeloid leukemia: an update of concepts and management recommendations of European LeukemiaNet.Journal of clinical oncology, 27(35), 6041-6051.
CML Society of Canada. (2010, March 18). CML Animation. Retrieved from https://www.youtube.com/watch?v=3tu3CWKbb4M
Corey, S., Cortes, J. (2010). Chronic Myeloid Leukemia: Pathophysiology and Therapeutics.
Deniniger, M., Goldman, J., Melo, J. (2000). The Molecular Biology of Chronic Myeloid Leukemia. Blood, 96(10), 3343 - 3356.
Druker, B. (2008). Translation of the Philadelphia chromosome into therapy for CML. Blood, 12(13), 4808 - 4817.
Druker, B. J., Talpaz, M., Resta, D. J., Peng, B., Buchdunger, E., Ford, J. M., … & Sawyers, C. L. (2001). Efficacy and safety of a specific inhibitor of the BCR-ABL tyrosine kinase in chronic myeloid leukemia. New England Journal of Medicine, 344(14), 1031-1037.
Fabbro, D. (2012). BCR-ABL signaling: A new STATus in CML. Nature Chemical Biology, 8, 228-229.
Goldman, J. M., & Melo, J. V. (2003). Chronic myeloid leukemia—advances in biology and new approaches to treatment. New England Journal of Medicine, 349(15), 1451-1464.
Hurtado et al. (2007). Chronic Myeloid Leukemia Current Concepts in Physiopathology and Treatment. Cancerología, 2, 137-147.
Pui, C. H., Behm, F. G., Raimondi, S. C., Dodge, R. K., George, S. L., Rivera, G. K., & Crist, W. M. (1989). Secondary acute myeloid leukemia in children treated for acute lymphoid leukemia. New England Journal of Medicine, 321(3), 136-142.
Sawyers, C. L. (1999). Chronic myeloid leukemia. New England Journal of Medicine, 340(17), 1330-1340.
Siegel, R. L., Miller, K. D., & Jemal, A. (2015). Cancer statistics, 2016. CA: A cancer journal for clinicians.
Vardiman, J. W., Thiele, J., Arber, D. A., Brunning, R. D., Borowitz, M. J., Porwit, A., & Bloomfield, C. D. (2009). The 2008 revision of the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia: rationale and important changes. Blood, 114(5), 937-951.