This is an old revision of the document!
Table of Contents
Thermal Injuries
Introduction
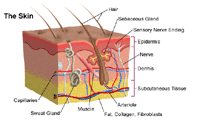
Skin is comprised of three anatomical layers: the epidermis, dermis, and subcutaneous tissue with each layer losing their function following a burn injury (Llyod et al., 2012)v. The epidermis layer acts as a barrier to bacteria and moisture loss, while the dermis provides elasticity and protection from trauma. The dermis also contains blood vessels that supply all the skin layers. When skin gets damaged, epidermal cells regenerate cells from deep within the dermal appendages, causing scarring (Llyod et al., 2012).
The International Society of Burn Injuries defines a burn as an injury sustained to the skin or any other organic tissue that is caused mainly by thermal or other acute trauma (Anandani, 2010). A burn occurs when some of all of the cells in the skin or other tissues get destroyed by contact with hot liquids (scalds), hot solids (contact burns) or through flames (flame burns). Other ways to receive burn injuries include radioactivity, friction, radiation, and contact with chemicals or electricity.The degree of tissue damage that is sustained through an injury depends on various factors (Anandani, 2010). These factors include the duration of contact with the source of the heat, the site of contact, the amount of heat energy, and sometimes also the agent itself which causes the burn.
Epidemiology
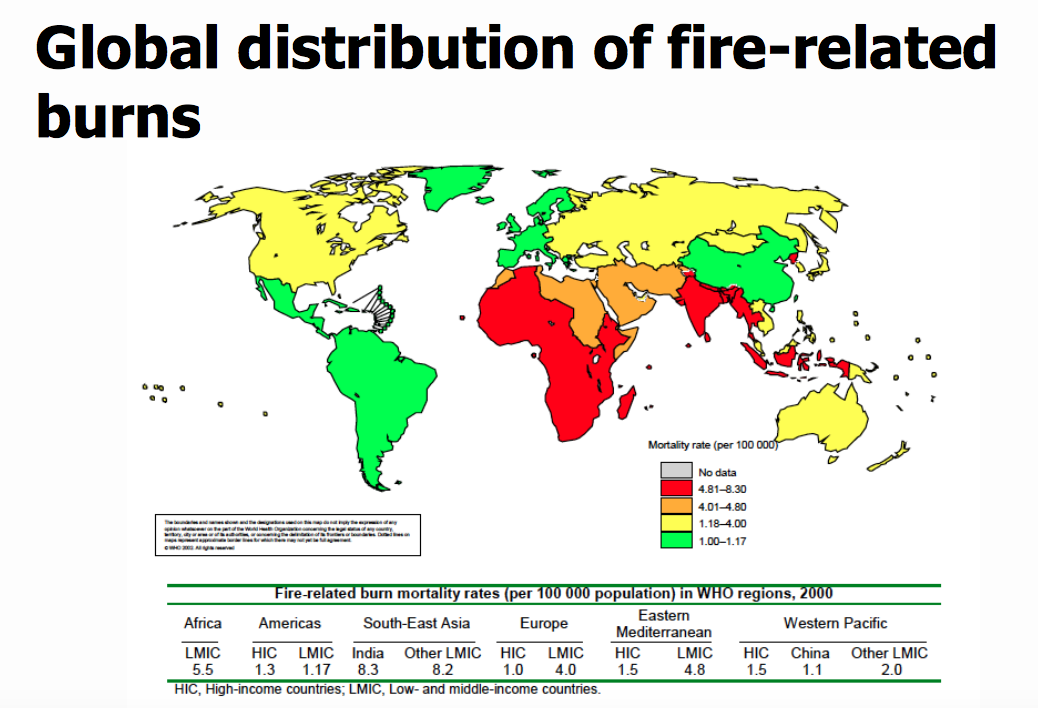
Globally, burns are a serious public health problem. Burns are the fourth most common type of trauma worldwide, following traffic accidents, falls, and interpersonal violence. An estimated 265 000 deaths occur each year from fires alone, with more deaths from scalds, electrical burns, and other forms of burns, for which global data are not available. Incidence varies by geographic location, socio-economic status, ethnic group, age and sex. Over 96% of fatal fire-related burns occur in low- and middle-income countries. In addition to those who die, millions more are left with lifelong disabilities and disfigurements, often with resulting stigma and rejection. High-income countries have made considerable progress in lowering rates of burn deaths, through combination of proven prevention strategies and through improvements in the care of burn victims.
Risk Factors
Factors that influence the incidence of burns injuries include age, sex, the home environment and economic status. Poverty is one of the main demographic factors associated with high risk of burns (Atiyeh et al.,2009).It has been reported that children of low-income families are reported to have more than eight times the risk of sustaining burns compared to those children from higher income families. Furthermore, those children from the most deprived social class have burn-related death rates that are 25 times greater than children from affluent social classes.Limited education, illiteracy, family patterns and the type of residence are other risk factors associated with burn injuries. Housing locations in high-density areas such as slums have been reported as significant risk factors for childhood burns in countries such as Bangladesh and Pakistan (Bishara et al.,2009).
Pathophysiology
Assessment and Diagnosis
Management
Prevention
Providing adequate burn care in the Western world costs around $1000 US dollar per patient per day (Atiyeh et al.,2009).. This is not an ideal situation for those in developing countries and emphasizes the fact that prevention is a primary means to reduce burn-related death and disabilities. Barriers to prevention in developing countries also include having limited resources, limited knowledge in regards to first-aid treatment and inaccessibility to modern medicine (Atiyeh et al.,2009).. The primary target group of prevention efforts should be children from a lower socioeconomic status. This group is the largest and most vulnerable group for burn injuries. It is important to recognize that many of the risk factors associated with burn injuries cannot be modified easily or quickly and thus a multifaceted solution is needed for burns prevention. A multifaced solution requires the help of health workers to promote burn prevention along with programs implemented to help fight issues such as educational deficits, poverty, overcrowding, and poor housing (Atiyeh et al.,2009).
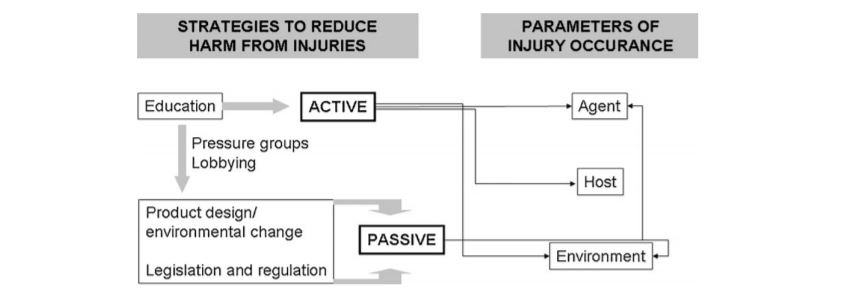
Atiyeh et al. (2009) highlight three main strategies that aim to reduce harm from injuries which include education, product design and environmental change, and legislation and regulation. In the strategies figure, strategies to reduce harm from injuries emphasize an active and passive approach. The educational strategy is an active approach focused on the individual (host) to help them avoid injury by modifying their environment to reduce the likelihood of injury. By knowing the environmental risks, it is more likely that preventative behavior will happen in an individual. Passive injury prevention involves product and environment modification. Product modification can be influenced by education the public to ask for safer products, and they can create pressure on authorities to produce prevention legislations (Atiyeh et al.,2009).
PowerPoint Presentation
References
Alharbi, Z., Piatkowski, A., Dembinski, R., Reckort, S., Grieb, G., Kauczok, J., & Pallua, N. (2012). Treatment of burns in the first 24 hours: simple and practical guide by answering 10 questions in a step-by-step form. World Journal of Emergency Surgery, 7(1), 13. Atiyeh, B. S., Costagliola, M., & Hayek, S. N. (2009). Burn prevention mechanisms and outcomes: pitfalls, failures and successes. Burns, 35(2), 181-193. Anandani, J.H. (2010). Impact of thermal injury on hematological and biochemical parameters in burnt patients. Bioscience Biotechnology Research Communications: 3(1): 97-100. “Burns.” John Hopkins Medicine. Retrieved January 22, 2017. http://www.hopkinsmedicine.org/healthlibrary/conditions/dermatology/burns_85,P01146/ Cakir, Baris and Berrak Yegen (2004). Systemic Responses to Burn Injury. Turk J Med Sci: 34: 215-226. http://journals.tubitak.gov.tr/medical/issues/sag-04-34-4/sag-34-4-1-0405-1.pdf DeSanti, Leslie (2005). Pathophysiology and Current Management of Burn Injury. Advances in Skin & Wound Care: 18(6):323-332. Hettiaratchy, Shehan and Peter Dziewulski (2004). Pathophysiology and Types of Burns. BMJ: 328(7453):1427-1429. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC421790/ Lloyd, E.C.O., Rodgers, B.C., Michener, M., & Williams, M.S. (2012). Outpatient burns: Prevention and care. American Family Physician, 85(1), 25-32. Peck, M. D. (2011). Epidemiology of burns throughout the world. Part I: Distribution and risk factors. Burns, 37(7), 1087-1100. Peden M., McGee K., Sharma G. (2002). The injury chart book: a graphical overview of the global burden of injuries. Geneva, World Health Organization. WHO. (2016). Fact Sheet on Burns. Violence and Injury Prevention, World Health Organization. Retrieved January 20, 2017 from http://www.who.int/mediacentre/factsheets/fs365/en/ WHO. (2007). Management of burns. Retrieved from http://www.who.int/surgery/publications/Burns_management.pdf