Table of Contents
Thermal Injuries
Introduction
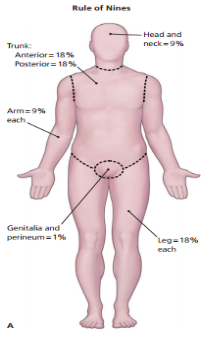
Skin is comprised of three anatomical layers: the epidermis, dermis, and subcutaneous tissue with each layer losing their function following a burn injury (Llyod et al., 2012)v. The epidermis layer acts as a barrier to bacteria and moisture loss, while the dermis provides elasticity and protection from trauma. The dermis also contains blood vessels that supply all the skin layers. When skin gets damaged, epidermal cells regenerate cells from deep within the dermal appendages, causing scarring (Llyod et al., 2012).
The International Society of Burn Injuries defines a burn as an injury sustained to the skin or any other organic tissue that is caused mainly by thermal or other acute trauma (Anandani, 2010). A burn occurs when some of all of the cells in the skin or other tissues get destroyed by contact with hot liquids (scalds), hot solids (contact burns) or through flames (flame burns). Other ways to receive burn injuries include radioactivity, friction, radiation, and contact with chemicals or electricity.The degree of tissue damage that is sustained through an injury depends on various factors (Anandani, 2010). These factors include the duration of contact with the source of the heat, the site of contact, the amount of heat energy, and sometimes also the agent itself which causes the burn.
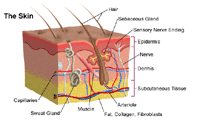 Figure 1- Anatomy of the skin. Retrieved from:http://www.hopkinsmedicine.org/healthlibrary/conditions/dermatology/burns_85,P01146/
Figure 1- Anatomy of the skin. Retrieved from:http://www.hopkinsmedicine.org/healthlibrary/conditions/dermatology/burns_85,P01146/
Epidemiology
Globally, burns are a serious public health problem. Burns are the fourth most common type of trauma worldwide, following traffic accidents, falls, and interpersonal violence. An estimated 265 000 deaths occur each year from fires alone, with more deaths from scalds, electrical burns, and other forms of burns, for which global data are not available. Incidence varies by geographic location, socio-economic status, ethnic group, age and sex. Over 96% of fatal fire-related burns occur in low- and middle-income countries. In addition to those who die, millions more are left with lifelong disabilities and disfigurements, often with resulting stigma and rejection. High-income countries have made considerable progress in lowering rates of burn deaths, through combination of proven prevention strategies and through improvements in the care of burn victims. According to the World Health Organization, the highest mortality rates are observed in low and middle income countries with most cases seen in Southeast Asia. Mortality rate among low-income countries is 11 times higher than in high-income countries. For example: In India, over 1 000 000 people are moderately or severely burnt every year. Children under 5 and the elderly have the highest burn mortality worldwide.
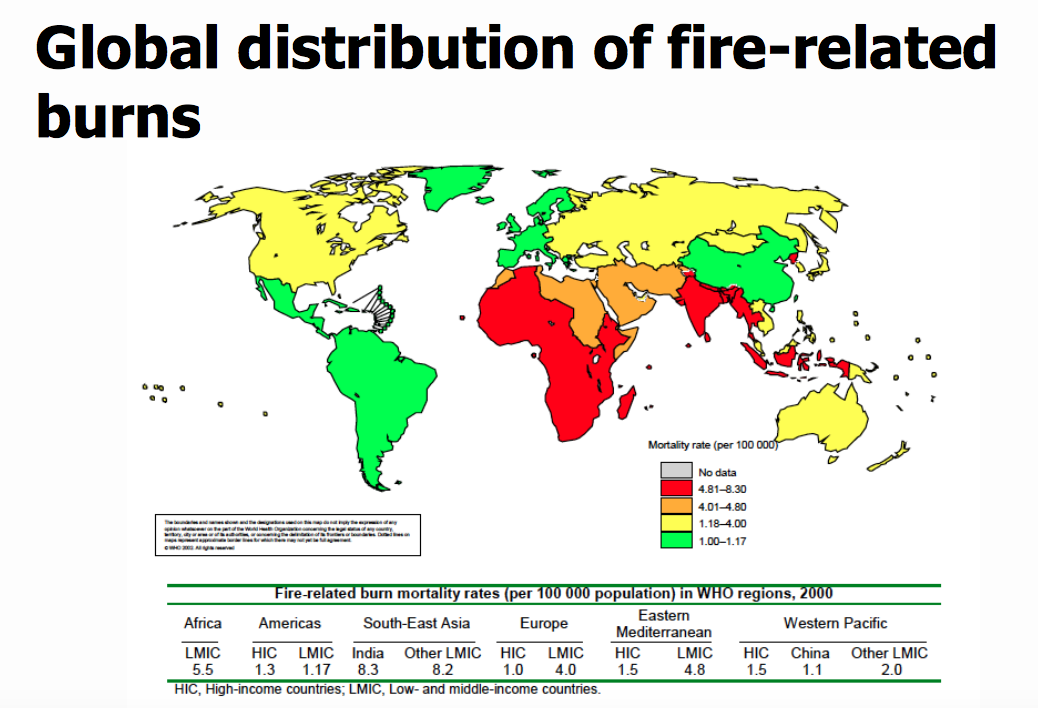
Figure 2- Injury related mortality rates (per 100,000 population) in WHO regions (Peden, 2002)
Risk Factors
Factors that influence the incidence of burns injuries include age, sex, the home environment and economic status. Poverty is one of the main demographic factors associated with high risk of burns. It has been reported that children of low-income families are reported to have more than eight times the risk of sustaining burns compared to those children from higher income families (Edelman,2007). Furthermore, those children from the most deprived social class have burn-related death rates that are 25 times greater than children from affluent social classes (Edelman,2007). Limited education, illiteracy, family patterns and the type of residence are other risk factors associated with burn injuries. Housing locations in high-density areas such as slums have been reported as significant risk factors for childhood burns in countries such as Bangladesh and Pakistan (Daisy et al.,2007).
Pathophysiology
The body responds to a burn injury in two ways: local response and systemic response. Locally, there is tissue damage and systemically, organ systems are affected as a result of the burn (DeSanti, 2005).
Local Response: Three Zones of a Burn
There are 3 zones of a burn, as described by Jackson’s Thermal Wound Theory.
- Zone of Coagulation: This is the most central location of the burn, where the damage is maximum and irreversible. This occurs due to coagulation of constituent proteins.
- Zone of Stasis: In this area there is decreased tissue perfusion (flow of blood). The tissue here can potentially be salvaged if it is not subject to additional damage such as an infection.
- Zone of Hyperemia: This is the peripheral area of the burn where there is an increased flow of blood and decreased cell injury. This area generally recovers unless there is additional damage such as an infection. (Hettiaratchy 2004).
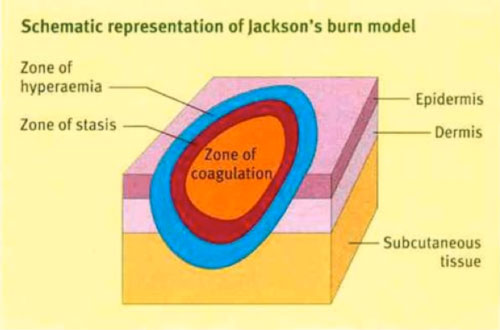 Figure 3- Jackson's burn zones (Hettiaratchym, 2004)
Figure 3- Jackson's burn zones (Hettiaratchym, 2004)
Three Zones of a Burn
Systemic Responses
Cardiovascular Response
There are 2 stages of cardiovascular response following a burn injury: acute/resuscitative phase, which lasts about 48 hours and a hypermetabolic phase. During the acute phase, there is decreased blood flow to tissues and organs due to the direct effect of heat. In this phase, there is an increase in capillary permeability, which further induces fluid and protein loss. During the hypermetabolic phase, there in an increase in internal temperatures and blood flow to tissues and organs. In this phase, there is formation of an edema as well as increased water permeability. This can lead to cardiac instability, hypotension and decrease in myocardial contractility. It may dispose an individual to myocardial infarction (Cakir 2004) (Hettiaratchy 2004).
Pulmonary Response
Within the first couple hours of a burn injury, lung inflammation and lipid peroxidation occurs, which increases oxygen radicals. This response persists for a minimum of 5 days following the burn. Mortality can occur among burn victims if there are respiratory difficulties from inhaling smoke. Inhalation injury after burn trauma includes bronchial obstruction, airway resistance and altered capillary permeability. In severe burns, adult respiratory distress syndrome can occur (Hiettiaratchy 2004).
Renal Response
The renal system of an individual responds by decreasing renal blood flow and glomerular filtration rate after a burn injury. Levels of stress hormones, such as catecholamine, angiotensin, aldosterone and vasopressin increase. These renal responses can result in acute renal failure, which can further result in mortality (Cakir 2004).
Gastrointestinal Response
The renal system of an individual responds by decreasing renal blood flow and glomerular filtration rate after a burn injury. Levels of stress hormones, such as catecholamine, angiotensin, aldosterone and vasopressin increase. These renal responses can result in acute renal failure, which can further result in mortality (Cakir 2004).
Immune Response
Thermal injury results in an immunosuppressed state. Following a burn, the body releases pro-inflammatory factors but there is a depression in the lines of defense. When the skin layers are damages, there can be microbial invasion and growth in the damaged skin. Neutrophil accumulation increases in tissues, phagocytic activity is inhibited, macrophage hyperactivity increases and T-cells cannot function properly. This results in an increase in reactive nitrogen intermediated which cause immune dysfunction. Due to this, there is an increased susceptibility to sepsis, the presence of bacteria and toxins in tissues, and this can result in multiple organ failure. Burn toxins and oxygen radicals are also produced, which further lead to peroxidation. Comprised immune function is a leading cause of morbidity and mortality in burn patients (Cakir, 2004) (Hettiaratchy, 2004).
Types of Burns
Thermal Burns
Thermal burns occur due to heat sources coming in contact with the skin and raising the temperature. They can be caused by exposure to hot charring liquids, flames, steam, hot metals etc. This can result in tissue cell death as well as charring.
Electrical Burns
Electrical burns occur through electrocutions, when an electric current travels through the body.
Chemical Burns
Chemical burns occur when the skin or eyes come in contact with chemical products that are corrosive agents. Alkalis, acids, detergents or solvents can cause this type of burn.
Radiation Burns
Radiation burns occur when the skin is exposed to sources of radiation, such as UV from the sun or X-rays, for a long time (John Hopkins Medicine 2007).
Classifications of Burns
First Degree (Superficial)
First-degree burns directly affect the outer layer of the skin (epidermis). The burn site appears to be dry and red. An example of a first-degree burn is a sunburn.
Second Degree (Partial Thickness)
Second-degree burns affect the epidermis and dermis layers of the skin. The burn site appears to be red, blistered and swollen. An example of a first-degree burn is a burn from scalding hot water.
Third Degree (Full Thickness)
Third-degree burns fully penetrate the epidermis and dermis layers. The burn site appears to be white or charred but there are no sensations of pain since the nerves are destroyed in these areas. An example of a third-degree burn is a flame burn from a fire.
Fourth Degree
Fourth-degree burns occurs when bones, muscles and tendons are burned in addition to the epidermis and dermis layers. They can occur from prolonged exposure to flame or an electrical injury from high voltage. (John Hopkins Medicine 2007).
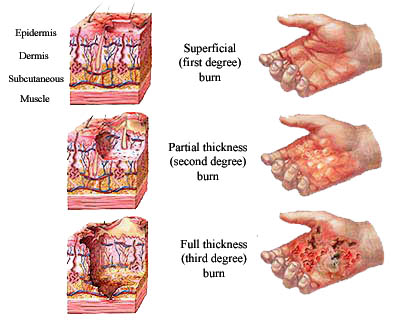 Figure 4- Burn injury classification. Retrieved from: http://www.burninjuryfirm.com/burn-injury-classification/
Figure 4- Burn injury classification. Retrieved from: http://www.burninjuryfirm.com/burn-injury-classification/
Assessment and Diagnosis
Physician conducts a thorough patient evaluation which includes getting a detailed description of the event that caused the thermal injury, any associated trauma that they may have acquired and pre-existing health conditions that they have. Physician will also ask whether they are having trouble breathing or are feeling pain anywhere else. In addition, he/she will ask whether the patient had lost consciousness at any point - this is a sign for potential inhalation injury (Alharbi et al, 2012).
There are two surveys that are conducted. The Primary Survey looks at A.B.C.D.E.F, which stands for Airway, Breathing, Circulation, Disability, Exposure and Fluid resuscitation. The primary survey is to help get an idea of how the patient can be potentially treated for his/her thermal injury. The Secondary Survey looks at the patient from head-to-toe. The physician will evaluate the burned area, measure the size, depth and surface area of wound. Tetanus shot given to all patients who have a greater than first-degree burn. A tetanus shot (tetanus prophylaxis is given to prevent bacterial infection from the exotocin produced by, Clostridium tetani. With infection, the disease tetanus results. Tetanus is a disease of muscle spasm and rigidity (Alharbi et al, 2012). The disease has a mortality rate of 20% due to spasm and rigidity of respiratory muscles). In the secondary survey, a burn assessment chart will be used to calculate the total body surface area (TSBA) of the burn. This chart is known is the Rule of Nines. Burns greater than 15% in adult, 10% children, and any in elderly is considered serious and would require further hospitalization care. Body is divided into regions of 9%. Morbidity and mortality arises with increased burned surface area (WHO, 2007).
A patient needs to be referred to a specialized burn care facility if the patient has partial thickness burns greater than 10% total body surface area (TSBA), if they have acquired an electrical burn (including lightning injury), if they have an inhalation injury, or if the patient has any pre-existing medical conditions (Alharbi et al, 2012).
Figure 5- Rule of Nines: Each body part is at 9% total body surface area (TBSA). The greater the body coverage due to thermal injury, the greater the risk of admittance to a specialized burn care facility (WHO, 2007).
Management
The objective of management involves rapid healing, pain control, return to full function and aesthetics (Lloyd et al., 2012).
Initial Management of Burns
Immediate treatment of minor thermal injuries includes cool running water exposed to wound area for 20 minutes (WHO, 2007). In animal studies, this was found to reduce depth of injury, increase re-epithelialization and improve cosmetic outcomes (WHO, 2007). Research of this nature is limited in humans, and benefits are known to have lasted for an hour. As a form of caution, it should be noted that ice water immersion can lead to injury and hypothermia (WHO, 2007).
Burns take time to heal, and this lengthy process can often be very painful. Due to the nature of this uncomfortable healing process, narcotic analgesics are often prescribed (WHO, 2007). The most common narcotics given are opioids (Enoch, Roshan & Shan, 2009). Typically, these analgesics are required during the process of wound healing and dressing application (WHO, 2007).
In the process of wound healing, do not scrub with povidone/iodine solution (Betadine), chlorhexidine (Peridex) or other cleaning agents (WHO, 2007). By doing so, the skin of the patient is more susceptible to itchiness, redness and burn. Sterile water is able to remove the debris. In the case of blisters, small blisters (<6 mm) in size can be left intact (WHO, 2007). Whereas large blisters with a thin wall should be debrided (WHO, 2007). A dressing should be applied on the wound. If the blister interferes with joint movement, it should be also debrided (WHO, 2007).
Burn wounds heal in moist environments, not wet environments (WHO, 2007). In the moist environment, reepithelization occurs and cellular dehydration is prevented. Topical agents and occlusive dressings are able to further prevent fluid loss. A combination of both treatments is able to provide pain control, promote healing, and prevent wound infection and desiccation (WHO, 2007). Topical Treatments for Initial Management In the case of a superficial burn, topical treatments involve lotion, honey, aloe vera or antibiotic treatments (WHO, 2007). These treatments are mainly chosen due to their antimicrobial nature. Topical non-steroidal and anti-inflammatory drugs can be combined with aloe vera to reduce pain (WHO, 2007). For partial thickness burns, topical antimicrobial agents can be used. These are classified as absorptive occlusive dressings and can reduce pain, promote healing and prevent wound desiccation (Garner & Heppell, 2005). The gold standard for occlusive dressings is silver sulfadiazine. In part, this is due the commonality of its use and its antimicrobial properties (mainly due to silver). For patients who are pregnant/lactating women, newborns or have Sulphur allergies, alternate occlusive dressings (ex. cerium nitrate) can be used (WHO, 2007). These are known to have a quick healing process, decrease pain, have fewer dressing changes and improve patient satisfaction (Garner & Heppell, 2007).
Long-term Management of Burns
After a burn occurs, a scar will often result (WHO, 2007). Though throughout long-term patient care, these may go maturation. They are first noted to be red and raised, then hypertrophic with keloid formation, and in the end, flat and soft. Scars are expected to fade with time, but the process can take up to 2 years (WHO, 2007).
A facial burn scar is often associated with cosmetic deformities. Ectropion (where the eyelid turns away from the eyeball) often results. In this case, there can be exposure to keratitis (inflammation of eye cornea) and a possibility of blindness (Enoch, Roshan & Shan, 2009). Moreover, contractures about the lip can develop. In this case, there is restriction to eating and mouth care. Due to the complexity of a facial deformity, a skin graft is not conducted (Enoch, Roshan & Shah, 2009). In these cases, patients must be provided with specialized care (ex. reconstructive or restorative surgery).
Many infections can arise due to burns. Cellulitis is typically not common in burns, but can occur (Lloyd et al., 2012). The infection is noted by severe erythematous, exudative, painful and swollen skin. Burn wounds have similar symptoms, and healthcare workers might have difficulty differentiating the two. In order to prevent such infections, patients are often provided with tetanus shots (Lloyd et al., 2012).
Infections around burn wounds can progress rapidly. Common pathogens include, staphylococcus aureus, streptococcus pyogenes, pseudomonas aeruginosa, acinetobater and klebisella species (Lloyd et al., 2012). Post-burn pruritus (itchiness of skin) may also occur. A common treatment is a Histamine H1 receptor agonist such as, cetirizine (Zyrtec). Topical doxepin (a tricyclic antidepressant with potent antihistamine properties) can reduce burn pruritus and erythema (Lloyd et al., 2012). Pulsed laser eye treatment can also be effective for post-burn pruritus, but more research is required. Pregabalin (Lyrica) can reduce post-burn naturopathic pain in 69% of patients (Lloyd et al., 2012).
With long term care, the depth and thickness of a burn is often evaluated. When a skin graft is required, apply split thickness skin graft to a full-thickness burn after wound excision. This should only be carried out after the appearance of healthy granulation tissue (Enoch, Roshan & Shah, 2009).
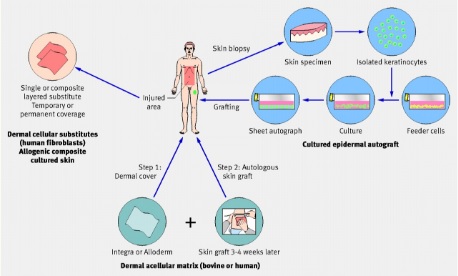 Figure 6 - Diagram Depicts the Process of Obtaining a Skin Graft (Enoch, Roshan & Shah, 2009)
Figure 6 - Diagram Depicts the Process of Obtaining a Skin Graft (Enoch, Roshan & Shah, 2009)
The American Burn Association (ABA) determined the criteria used by primary physicians when sending patients to burn centers. If there are facial burns, a referral is required due to the prospect of psychological and identity issues (Lloyd et al., 2012). Also, patients are sent if there are full-thickness burns or any burns to the hand, feet, perineum and genital area (due to anatomy and physiology of region). Moreover, circumferential burns must also be referred in order to reduce the risk of compartment syndrome (Lloyd et al., 2012).
If a patient has a burn over their joint, they may be referred to an occupational and/or physical therapist (Lloyd et al., 2012). Throughout the phase of wound healing, patients are often prescribed long periods of bed rest. As a result, a loss of muscle function or limited range of motion is expected. Due to the nature of burn healing, patient activity is restricted. Hence, there is a stiffness and weakness surrounding joints. In this situation, patients should also be referred to occupational therapists (Lloyd et al., 2012).
Due to the catabolism of trauma, heat loss and demand of tissue regeneration, patient energy and protein requirements are quite high (Lloyd et al., 2012). If required, patients may be fed through nasogastric tube in order to obtain adequate amounts of energy. Burn patients typically require 6000 kcal per day. Anemia and malnutrition may also prevent wound healing (cause failure of skin graft). Hence, patients should be referred to nutritionists in order to ensure their diet collaborates with their healing process (Lloyd et al., 2012).
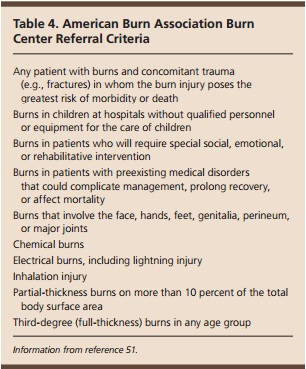 Figure 7 - American Burn Association Criteria for Referral to Burn Centres (Lloyd et al., 2012)
Figure 7 - American Burn Association Criteria for Referral to Burn Centres (Lloyd et al., 2012)
Paediatric Burn Management
Most of the burn management process between adults and children is similar, however there are slight differences.
Burn scars in children do not expand and keep up with body growth. As a result, children can experience contractures (Lloyd et al., 2012). This includes the shortening and hardening of muscles, tendons, and can result in deformed and rigid joints. Early surgical release from the contractures is required to prevent growth interference (Lloyd et al., 2012).
Due to the devastating nature of child burns, burn prevention is a common focus. The ABA attempts to educate the public of common burns. For instance, scalding results from contact with hot objects of liquids. Whereas, flame related injuries are common in patients older than six years (Lloyd et al., 2012).
Prevention
Providing adequate burn care in the Western world costs around $1000 US dollar per patient per day (Atiyeh et al.,2009).. This is not an ideal situation for those in developing countries and emphasizes the fact that prevention is a primary means to reduce burn-related death and disabilities. Barriers to prevention in developing countries also include having limited resources, limited knowledge in regards to first-aid treatment and inaccessibility to modern medicine (Atiyeh et al.,2009).. The primary target group of prevention efforts should be children from a lower socioeconomic status. This group is the largest and most vulnerable group for burn injuries. It is important to recognize that many of the risk factors associated with burn injuries cannot be modified easily or quickly and thus a multifaceted solution is needed for burns prevention. A multifaced solution requires the help of health workers to promote burn prevention along with programs implemented to help fight issues such as educational deficits, poverty, overcrowding, and poor housing (Atiyeh et al.,2009).
Atiyeh et al. (2009) highlight three main strategies that aim to reduce harm from injuries which include education, product design and environmental change, and legislation and regulation. In the strategies figure, strategies to reduce harm from injuries emphasize an active and passive approach. The educational strategy is an active approach focused on the individual (host) to help them avoid injury by modifying their environment to reduce the likelihood of injury. By knowing the environmental risks, it is more likely that preventative behavior will happen in an individual. Passive injury prevention involves product and environment modification. Product modification can be influenced by education the public to ask for safer products, and they can create pressure on authorities to produce prevention legislations (Atiyeh et al.,2009).
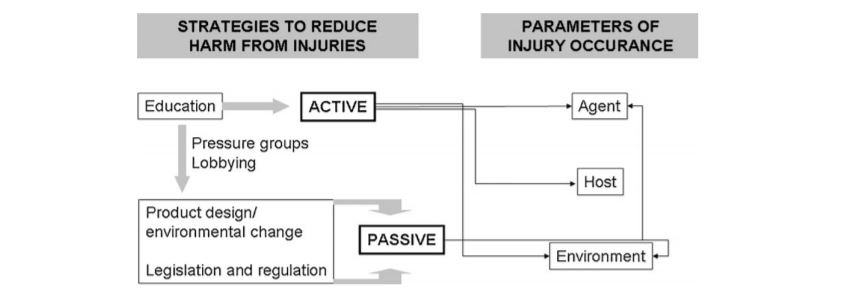 Figure. 8 – Strategies to reduce harm from injury (Atiyeh et al., 2009)
Figure. 8 – Strategies to reduce harm from injury (Atiyeh et al., 2009)
Presentation
References
Alharbi, Z., Piatkowski, A., Dembinski, R., Reckort, S., Grieb, G., Kauczok, J., & Pallua, N. (2012). Treatment of burns in the first 24 hours: simple and practical guide by answering 10 questions in a step-by-step form. World Journal of Emergency Surgery, 7(1), 13.
Atiyeh, B. S., Costagliola, M., & Hayek, S. N. (2009). Burn prevention mechanisms and outcomes: pitfalls, failures and successes. Burns, 35(2), 181-193.
Anandani, J.H. (2010). Impact of thermal injury on hematological and biochemical parameters in burnt patients. Bioscience Biotechnology Research Communications, 3(1), 97-100.
“Burns.” John Hopkins Medicine. Retrieved January 22, 2017. http://www.hopkinsmedicine.org/healthlibrary/conditions/dermatology/burns_85,P01146/
Cakir, Baris and Berrak Yegen (2004). Systemic Responses to Burn Injury. Turk J Med Sci: 34: 215-226. http://journals.tubitak.gov.tr/medical/issues/sag-04-34-4/sag-34-4-1-0405-1.pdf
Daisy, S., Mostaque, A. K., Bari, S., Khan, A. R., Karim, S., & Quamruzzaman, Q. (2001). Socioeconomic and cultural influence in the causation of burns in the urban children of Bangladesh. Journal of Burn Care & Research, 22(4), 269-273.
DeSanti, Leslie (2005). Pathophysiology and Current Management of Burn Injury. Advances in Skin & Wound Care: 18(6):323-332.
Edelman, L. S. (2007). Social and economic factors associated with the risk of burn injury. Burns, 33(8), 958-965.
Enoch, S., Roshan, A., & Shah, M. (2009). Emergency and early management of burns and scalds. BMJ, 338, b1037.
Garner, J.P., & Heppell, P.S.J. (2005). Cerium nitrate in the management of burns. Burns, 31(5), 539-547.
Hettiaratchy, Shehan and Peter Dziewulski (2004). Pathophysiology and Types of Burns. BMJ, 328(7453), 1427-1429. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC421790/
Lloyd, E.C.O., Rodgers, B.C., Michener, M., & Williams, M.S. (2012). Outpatient burns: Prevention and care. American Family Physician, 85(1), 25-32.
Peck, M. D. (2011). Epidemiology of burns throughout the world. Part I: Distribution and risk factors. Burns, 37(7), 1087-1100.
Peden M., McGee K., Sharma G. (2002). The injury chart book: a graphical overview of the global burden of injuries. Geneva, World Health Organization.
WHO. (2016). Fact Sheet on Burns. Violence and Injury Prevention, World Health Organization. Retrieved January 20, 2017 from http://www.who.int/mediacentre/factsheets/fs365/en/
WHO. (2007). Management of burns. Retrieved from http://www.who.int/surgery/publications/Burns_management.pdf