This is an old revision of the document!
Table of Contents
Burns
Introduction
What are Burns?
Burns are a common household and workplace injury, especially prevalent among children. The name does not only refer to the burning sensation characterized by the injury, but is also characterized by severe skin damage that causes necrosis of the affected skin tissue cells (Khan & Solan, 2016). Damage to the body tissues may be caused by heat, chemicals, electricity, sunlight or radiation. Inhalation burns may also develop from concentrated inhalation of smoke (Khan & Solan, 2016).
Most burns are recoverable without serious health consequences, however some severe burns require immediate medical attention to prevent further injury and complications.
There are three main types of burns, categorized by degree (first to third). The type of burn is not based on the cause, rather each degree is based on the severity of skin damage and cell death, as well as how long the contact of the burn is exposed to the skin (Khan & Solan, 2016).
How Can Burns Be Acquired?
A burn is acquired through contact with the cause of the heat on the skin or other organs. Burn injuries often occur either in the home or at work and are the cause of the most non-life threatening morbidities to the body. Unlike uncontrollable life threatening injuries burns can be easily preventable through proper protection, knowledge and training. Knowing the forms and causes of heat you can potentially be exposed to is very important to limit the amount of burns people acquire. Also, knowing the risk factors pertaining to different areas can be helpful to know what forms and causes are more common in that area (World Health Organization, 2017).
Figure 1 - This image shows the common cooking conditions in developing countries.
Forms of Heat:
- Hot liquids
- Hot solids
- Flames (World Health Organization, 2017)
Causes of Burns:
- Heat
- Radiation
- Radioactivity
- Electricity
- Chemicals (World Health Organization, 2017)
Figure 2 - Image of a mechanic near a heat source.
- Gender
- Age
- Regional factors
- Socioeconomic factors
- Other (World Health Organization, 2017)
Epidemiology
The incidence of burn injuries varies across age groups, gender, income and geographic location (Peck, 2017). In the U.S., almost 1.4 million people suffer from burn-related injuries yearly and nearly 54,000 to 180,000 are hospitalized as a result of these injuries (Epidemiology, 2017). Approximately 20-25% of burns are work-related and 67% of serious burn injuries occur in males. The 20-29 year-old demographic has the highest prevalence of serious burn injuries, followed by children under 9 years of age. Individuals above the age of 50 have the least occurrences of serious burn injuries accounting for only 2.3% (Epidemiology, 2017).
Flame burns and liquid scalds are the main causes of severe burn injury (Epidemiology, 2017). Most children under the age of 2 sustain severe burn injuries due to liquid scalds and hot surface burns, while children above the age of 2 suffer from severe burn injuries due to flame burns.
In the past 20 years, deaths from burn-related injuries have declined (Epidemiology, 2017). This decrease is a result of improved firefighting techniques, emergency medical services and the use of smoke detectors which has been attributed to an 80% decrease in mortality and a 74% reduction in injuries from residential fires (Epidemiology, 2017). Worldwide, 90% of burn deaths occur in low and middle-income countries where prevention programs are not in place and the quality of acute care is not readily available (Peck, 2011)
Etiology
The majority of burns are caused by a variety of environmental factors (Thermal Burns, 2017).
Thermal Burns: Flame burns, the most common type of burn, are sustained when the flame makes direct contact with the skin and tissue resulting in injury (Thermal Burns, 2017). A contact burn is damage to the skin caused by a hot object and include burns from cigarettes, irons or cooking appliances. A scald is a wound to the skin caused by a hot liquid, where the scald becomes greater depending on the thickness of the liquid and its duration of contact with the skin (Thermal Burns, 2017).
Electrical Burns: Burns caused by exposure to low, intermediate and high voltage electric currents (Cutaneous burns, 2017). Generally these burns tend to be deep and cause serious impairment to the skin and tissue (Thermal Burns, 2017).
Chemical Burns: Contact or exposure to industrial or household chemical products including flammable gases or liquids cause chemical burns (Cutaneous burns, 2017). Breathing difficulties result from the inhalation of hot gases, as they could damage upper airways (Thermal Burns, 2017).
Sunburns: Damage to the skin caused by ultraviolet rays emitted from the sun, tanning beds or sunlamps (Thermal Burns, 2017).
Ice Burns: Ice burns result when skin makes contact with ice or cold for a long period of time (Ice Burn, 2017). Ice burns cause the water in the cells of your skin to freeze, resulting in the development of sharp ice crystals that impair the composition of your skin cells causing blood vessels to constrict. Extended contact with snow, cold weather, or high-velocity winds can cause ice burns as well as the use of ice or cold packs when pressed directly onto bare skin (Ice Burn, 2017).
Non-accidental Burns: Nearly 20% of burns in children are caused by abuse or neglect (Cutaneous burns, 2017).
Clinical Presentation
First Degree Burns
This is the lowest grade of burn. Patients with first degree burns will present with red, non-blistered skin. There may be minor inflammation or swelling, some pain, and the affected tissue will be dry. As the burn begins to heal, skin will often peel and flake off (Burns, n.d.).
Although these burns are not serious, if the affected tissue covers a large area of your skin (more than 3 inches), or it is located on a major joint or face, then it is still important to see a doctor.
Second Degree Burns
Second degree burns are slightly more worrisome, as the damage extends beyond the top layer of the epidermis. The injured tissue will appear blistered, with some thickening of the skin, and extreme redness and soreness. Some of the blisters may pop open, giving a wet or weeping appearance to the burn. Scab-like tissue called fibrinous exudate may develop over the wound as it begins to heal (Burns, n.d.).
Third Degree Burns
Third degree burns are very serious, extending through every layer of the skin and causing the most damage. These burns require immediate medical attention. Patients will present with widespread thickness of affected tissue with a white leathery appearance. Affected tissue may range in colour from waxy and white to charred brown (Herndon et al., 1986).
It is a general misconception that third degree burns are the most painful. In fact, many patients with this severity of burn do not experience any pain at all. When the tissue damage extends through all layers of the skin, it often causes extensive nerve damage which prevents the patient from experience pain at the site of injury (Herndon et al., 1986).
Without surgery to repair these burns, the wound may heal with severe scarring and contracture.
Fourth Degree Burns
These types of burns are very rare, and severe. In some cases, if medical intervention is not immediately available, injury can be fatal (Herndon et al., 1986).
A patient with fourth degree burns will present with all symptoms of third degree burns, but the affected tissue will extend further beyond the layers of the skin and into the tendons, fascia and bone. These burns are almost never associated with pain, as most of the adjacent nerves in the area are significantly damaged (Herndon et al., 1986).
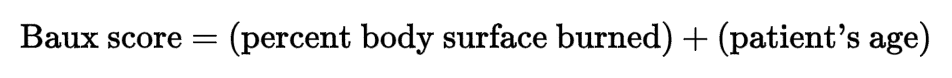
The Baux Scale
The Baux scale is a score system that is used to predict the chance of mortality due to severe burns. The score accounts for the correlative and causal relationship between mortality and other factors of injury including: age, burn size, and the presence of an inhalation injury (Krob et al., 1991). Studies have also shown that this scale correlates to a patient's length of stay in the hospital due to burns, as well as final health outcome as a result of the injury.
The original Baux score was the sum of the percent body surface burned plus the patient's age. If this score was over 140, then the burn was considered to be unsurvivable. This still had some variability depending on the immediate available treatment resources (Krob et al., 1991).
Figure 4 - This is the original Baux score equation, used to determine the risk of mortality for a burn patient. (Krob et al., 1991)
Later research modified the Baux scale to include inhalation injury. If a patient suffered from inhalation injury, they would have 17 added to their final score (Krob et al., 1991).
Physiology
Epidermis is the first layer and is a thin outer layer of the skin with many layers including stratum corneum, keratinocytes and basal layer (John Hopkins Medicine, 2017). The stratum corneum houses cells that contain keratin. This is a protective layer which keeps the body fluid in while keeping external substances out. The cells of this layer contentiously shed (John Hopkins Medicine, 2017). The next epidermal layer is a layer of keratinocytes or squamous cells. This layer is made up of living cells that are maturing and moving toward the surface to become the stratum corneum. The last epidermal layer is the basal layer where cells divide to replace the old cells that are shed at the surface (John Hopkins Medicine, 2017). The second major layer of the skin is the dermis. The dermis is held together by a protein called collagen, which is made by fibroblasts. The dermis contains blood vessels, lymph vessels, hair follicles, sweat glands, collagen bundles, fibroblasts and nerves. This layer also contains nerve endings that conduct pain and sensation signals. The second major layer of the skin is the subcutis (John Hopkins Medicine, 2017). The subcutis is the deepest layer of the skin. It contains a network of collagen and fact cells which help conserve the body’s heat and protect the body from injury by acting as a shock absorber (John Hopkins Medicine, 2017).
Pathophysiology
Local Response
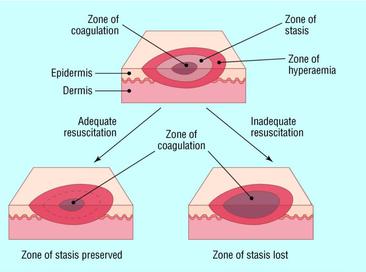 The local response varies by zones (Shehan Hettiaratchy, 2004). The zone of coagulation is the zone that occurs at the point of maximum damage (Shehan Hettiaratchy, 2004). There is irreversible tissue loss due to coagulation of the constituent proteins. The second zone is the zone of stasis. This zone is the surrounding zone of decreased tissue perfusion. This tissue could be potentially salvageable (Shehan Hettiaratchy, 2004). The aim of burn resuscitation is to increase tissue perfusion at this sight and prevent any damage becoming irreversible. The tissue in this area can be completely lost due to prolonged hypotension, infection or edema. The third zone of local response is the zone of hyperaemia (Shehan Hettiaratchy, 2004). This is the outermost zone in which tissue perfusion is increased. This tissue will recover unless undergoes severe sepsis or prolonged hypoperfusion (Shehan Hettiaratchy, 2004).
The local response varies by zones (Shehan Hettiaratchy, 2004). The zone of coagulation is the zone that occurs at the point of maximum damage (Shehan Hettiaratchy, 2004). There is irreversible tissue loss due to coagulation of the constituent proteins. The second zone is the zone of stasis. This zone is the surrounding zone of decreased tissue perfusion. This tissue could be potentially salvageable (Shehan Hettiaratchy, 2004). The aim of burn resuscitation is to increase tissue perfusion at this sight and prevent any damage becoming irreversible. The tissue in this area can be completely lost due to prolonged hypotension, infection or edema. The third zone of local response is the zone of hyperaemia (Shehan Hettiaratchy, 2004). This is the outermost zone in which tissue perfusion is increased. This tissue will recover unless undergoes severe sepsis or prolonged hypoperfusion (Shehan Hettiaratchy, 2004).
Systemic Response
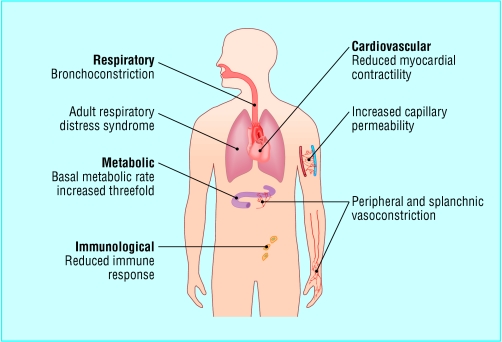 The systemic response is the effect of a burn on the whole body (Shehan Hettiaratchy, 2004). Once the burn reaches 30% of total body area, the release of cytokines and other inflammatory mediators at the site of injury results in a systemic response. Cardiovascular changes occur in severe cases as well (Shehan Hettiaratchy, 2004). The capillary permeability is increased which results in loss of intravascular proteins and fluids into the interstitial compartment. This leads to peripheral and splanchnic vasoconstriction. Contractility of the cardiac muscles increases, possibly due to release of tumour necrosis factor a. These changes along with the fluid loss lead to systemic hypotention and pypoperfusion. Respiratory changes also occur (Shehan Hettiaratchy, 2004). Inflammatory cells cause bronchoconstriction and in severe burns lead to adult respiratory distress syndrome. There are also metabolic changes that occur (Shehan Hettiaratchy, 2004). The basal metabolic rate increases up to three times its original rate. The increase in splanchnic metabolic rate and hypoperfusion requires the patient to undergo enteral feeding to prevent and decrease catabolism and gut integrity. Severe burns also result in immunological changes such as non-specific downregulation of immune response. This affects both the humoral and cell-mediated pathways (Shehan Hettiaratchy, 2004).
The systemic response is the effect of a burn on the whole body (Shehan Hettiaratchy, 2004). Once the burn reaches 30% of total body area, the release of cytokines and other inflammatory mediators at the site of injury results in a systemic response. Cardiovascular changes occur in severe cases as well (Shehan Hettiaratchy, 2004). The capillary permeability is increased which results in loss of intravascular proteins and fluids into the interstitial compartment. This leads to peripheral and splanchnic vasoconstriction. Contractility of the cardiac muscles increases, possibly due to release of tumour necrosis factor a. These changes along with the fluid loss lead to systemic hypotention and pypoperfusion. Respiratory changes also occur (Shehan Hettiaratchy, 2004). Inflammatory cells cause bronchoconstriction and in severe burns lead to adult respiratory distress syndrome. There are also metabolic changes that occur (Shehan Hettiaratchy, 2004). The basal metabolic rate increases up to three times its original rate. The increase in splanchnic metabolic rate and hypoperfusion requires the patient to undergo enteral feeding to prevent and decrease catabolism and gut integrity. Severe burns also result in immunological changes such as non-specific downregulation of immune response. This affects both the humoral and cell-mediated pathways (Shehan Hettiaratchy, 2004).
Pathophysiology of Burn Wound
The burn pathophysiology is characterized by an inflammatory reaction which leads to formation of oedema (Arturson, 1980). Oedema forms due to increased microvascular permeability, vasodilation and increased extravascular osmotic activity. These responses are caused by the chemical mediators of inflammation and the direct heat effect of a burn on the microvasculature. Vasodilation and increased vascular permeability is mostly initiated by histamine release (Arturson, 1980). Free radicals are released from polymorphonuclear leucocytes which cause damage to the cell membrane. This damage activates the enzymes that catalyze the hydrolysis of prostaglandin precursor causing rapid formation of prostaglandin. Prostaglandin inhibits the release of norepinephrine thus modulating the adrenergic nervous system which is activated in response to thermal injury (Arturson, 1980). The morphological changes of the blood lymph barrier are the increase in the number of vacuoles and many open endothelial intercellular junctions (Arturson, 1980). As well, the continuous loss of fluid from the blood circulation in the areas of damaged tissue results in an increase in haematocrit levels and a rapid fall in plasma volume as well as deceased cardiac output and hypoperfusion on cellular level. Burn shock will develop if the fluids are not restored. Also, burn wound provides a substantial area for entry of surface infection resulting in high risk of septic shock (Arturson, 1980).
Psychosocial Outcomes
Psychosocial Outcomes of Burns
Acute Phase
Patients with burns exhibit symptoms of anxiety and depression which begin to appear in the acute phase of recovery (Wiechman & Patterson, 2004). Acute stress disorder and post-traumatic stress disorder are more common after burns than other forms of injury. These symptoms are typically seen in patients that have larger burns and more severe pain and express more guilt about the precipitating event (Wiechman & Patterson, 2004). The severity of depression is correlated with a patient’s level of resting pain and level of social support. Sleep disturbance is central to both the anxiety and depression. Sleep can be affected by patient’s mood, agitation and nightmares (Wiechman & Patterson, 2004). Also, the patient is often awakened during the night for analgesia or for vital signs. At this stage, the patient may also begin the grieving process as they become more aware of the impact the burns might have on their life relating job, mobility, physical ability and appearance (Wiechman & Patterson, 2004).
Long Term Rehabilitation
High demands of long-term rehabilitation and social stressors such as family strains, return to work, sexual dysfunction, change in body image and disruption in daily may also cause negative psychosocial outcomes (Wiechman & Patterson, 2004). Patients could experience distress caused by vivid memories of the incident. However, adjustment to burn injuries improves over time and is believed to be independent of size of injury (Wiechman & Patterson, 2004). As well, burn scars are known to cause psychosocial outcomes (Lawrence et al, 2001). Multiple studies have reported that visibility, severity and location of scar have a strong relationship with the quality of life in the survivors of the major burns. Specifically, these burn characteristics are highly associated with psychosocial variables such as social comfort and perceived (Lawrence et al, 2001).
Treatment
Treatment Based on Burn Classification
The treatment protocols put in place are based on the degree of burn (Kagan et al, 2009). In a first degree burn, only the epidermis is involved. Blisters do not form, but the burn is red and quite painful (Kagan et al, 2009). Usually, in 2-3 days, erythema and pain dissipate. By day 4, the injured epithelium peels away from the newly healed epidermis, a process which is commonly seen after a sunburn (Kagan et al, 2009). The second degree burns fall under two categories: partial-thickness burns and superficial partial-thickness burns. Partial thickness burns involve the epidermis and portions of the dermis and can be clinically categorized as either superficial partial-thickness or deep partial-thickness (Kagan et al, 2009). Superficial partial-thickness burns characteristically form blisters between the epidermis and dermis. Since blistering may not occur for some hours after the burn injury, burns that initially appear to be only epidermal in depth may be determined to be partial-thickness burns after 2-4 hours later (Kagan et al, 2009). Most superficial partial thickness burns will heal spontaneously in less than 3 weeks and do so typically without functional impairment or hypertrophic scarring (Kagan et al, 2009).
Second degree burns accumulate a layer of fibrous exudate and necrotic debris of the injured surface, which may predispose the wound healing and additionally making it more difficult to determine the wound depth by visual inspection (Kagan et al, 2009). Most deep partial thickness burns extend into the lower layers of the dermis and possess characteristics that are distinctly different from superficial or mid-dermal partial-thickness burns. These burns take 3 to 9 weeks to heal (Kagan et al, 2009). These burns invariably cause considerable scar formation and joint function is usually impaired, therefore are best treated by excision and grafting. If a partial thickness burn fails to heal within 3 weeks, it is functionally and cosmetically equivalent to a full-thickness injury (Kagan et al, 2009).
Third degree burns are full thickness burns that involve 3 layers of the dermis and often injure underlying subcutaneous adipose tissue as well. These types of burns contain burn eschars that are firm and structurally intact covering the head and denatured dermis. In a few days, if left intact, the eschar will separate from the underlying viable tissue, leaving an open unhealed bed of granulated tissue (Kagan et al, 2009). Without surgery, they can heal only by wound contracture with epithelialization from the wound margins. Some full-thickness burns involve not only all layers of the skin, but also deeper structures such as muscle, tendon, ligament and bone and are classified as deep full-thickness or fourth degree (Kagan et al, 2009). In order to treat these burns, grafting may use autologous skin grafts or biological dressings and kin substitutes or both. Deep full-thickness burns may require amputation or closure with alternative techniques (Kagan et al, 2009).
Burn care assumes a series of ongoing but separate interventions until healing of all wounds whether operated or non-operated is achieved (Kagan et al, 2009). Multiple stages of staged and non-staged surgical procedures may be necessary followed by substantial procedural care that was not anticipated at the time of the previous surgical intervention (Kagan et al, 2009). Critical care services are a necessary component of daily care for patients with extensive or complicated burn injuries. The burn management requires significant attention to pathophysiological changes by the systemic response to the burn injury (Kagan et al, 2009). In that case, patients would need meticulous evaluation and correction of fluid and electrolyte, metabolic, cardiopulmonary, homeostatic and infectious derangements (Kagan et al, 2009). The labour-intensive daily critical care evaluation and management service is necessary to achieve satisfactory results (Kagan et al, 2009). Diabetes mellitus, obesity, hypertension and cardiovascular disease can become an enormous barrier to burn wound healing. The best outcome is achieved when the surgeon the burn surgeon also provides careful management of these conditions throughout the patient’s critical course (Kagan et al, 2009).
Surgical Treatment
 Escharotomy is a surgical incision through the burn eschar (Kagan et al, 2009). This procedure is usually performed within the first 24 hours of burn injury. Burn eschar has an unyielding, leathery consistency and is characterized by denatured proteins and coagulated vessels in the skin (Kagan et al, 2009). When the burn eschar circumferentially surrounds any body structure, the tissues within are subject to increasing interstitial pressures exacerbated by the tissue edema that develops during the acute phase of burn resuscitation in the first 48 hours after burn injury (Kagan et al, 2009). This procedure releases the constriction caused by the burn eschar but do not remove the eschar. After approximately a week, the burn eschar is excised to the level of viable underlying tissue (Kagan et al, 2009).
Escharotomy is a surgical incision through the burn eschar (Kagan et al, 2009). This procedure is usually performed within the first 24 hours of burn injury. Burn eschar has an unyielding, leathery consistency and is characterized by denatured proteins and coagulated vessels in the skin (Kagan et al, 2009). When the burn eschar circumferentially surrounds any body structure, the tissues within are subject to increasing interstitial pressures exacerbated by the tissue edema that develops during the acute phase of burn resuscitation in the first 48 hours after burn injury (Kagan et al, 2009). This procedure releases the constriction caused by the burn eschar but do not remove the eschar. After approximately a week, the burn eschar is excised to the level of viable underlying tissue (Kagan et al, 2009).
Debridement of burn wounds is another procedure which involves removal of loose, devitalized necrotic contaminated tissue, foreign bodies and other debris on the wound using mechanical and sharp techniques (Kagan et al, 2009). Wound healing is optimized when wound surfaces are clean with minimal microbial colonization and necrotic debris present (Kagan et al, 2009).
Excision of burn wounds is a surgical procedure which requires incision through the deep dermis of open wounds, burn eschar and burn scars (Kagan et al, 2009). This involves surgical removal of all necrotic tissue. Excision of burn scars could also be performed on deep burn that would not heal on their own (Kagan et al, 2009). The goal is to remove all necrotic and viable tissue and to prepare the wound for immediate or delayed would closure (Kagan et al, 2009). 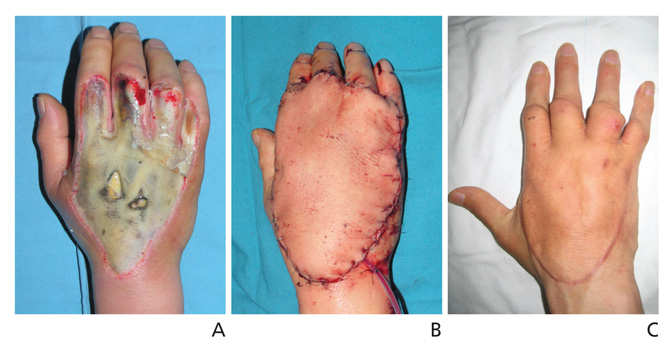
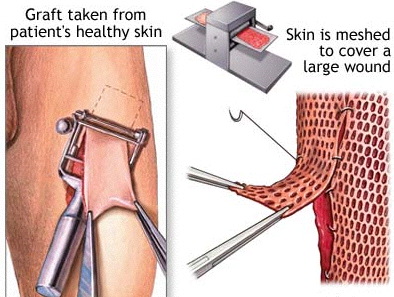
Grafting
Skin grafting is a type of surgery used to treat burn patients. It is performed under anesthesia where healthy skin is taken from a section on your body defined as the donor site (Skin graft, 2017). Two types of skin graft procedures are available (Plastic Surgery, 2017). Split-thickness grafts involve the transplant of only a few layers of the outer skin whereas full-thickness grafts encompass all of the dermis, resulting in permanent scarring. Most individuals have a split-thickness skin graft which involves taking the epidermis and dermis layers of the donor site (Skin graft, 2017). The donor site is taken from sections of the body that are usually covered, such as buttocks or inner thigh regions. The graft is spread on the bare region in need of covering and is held together by a dressing and a few stitches (Plastic Surgery, 2017). A sterile dressing covers the donor site for 3 to 5 days to prevent any infections from arising. Split-thickness skin grafts tend to have a quick recovery period compared to full-thickness skin grafts which tend to require longer hospital stays (Skin graft, 2017).
Figure#: Skin graft procedure.
http://personalpages.manchester.ac.uk/staff/j.gough/lectures/te/13_skin/page7.html
Surgical closure of burn wounds achieves the following goals: to facilitate optimal and rapid healing of the wound and the second is to better the adverse influence of the burn wounds on the body’s systematic responses, especially the immune and metabolic systems (Kagan et al, 2009). Multi-stage excision and grafting involves a series of steps. In this process, part of the burn wound is excised initially and the remainder is removed in one or more subsequent operations. This is often done with cosmetically important areas such as the face as well as with more extensive burns in physiologically less stable patients (Kagan et al, 2009). There are some risks associated with skin graft surgery including bleeding, loss of grafted skin where the graft does not heal or heals at a slow pace, increased sensitivity, uneven skin surface, chronic pain (rare) and skin discoloration (Skin graft, 2017).
Burn Teams
The amount of burn victims and severity has caused the creation of burn centers. Within these burn centres is what is now known as burn teams. The teams consist of individuals from a variety of areas in the health field to have a multidisciplinary approach. One health professional on their own does not have the knowledge and experience to deal with the physical burn and the psychological affects that come with it. Without burn units and their teams, individuals that are inflicted with burns will go to a general hospital and receive care like any other patient where they are treated for the infliction and not on an individual level (Edwards, Heard, Latenser, Quinn, van Bruggen , & Jovic, 2011).
- Burn Surgeons: The leaders of the team. Organize and implement the care of the patient. Since the locations of burns varies, different types of surgeons are needed depending on where the burn is located. They need to be able to lead and communicate with the team as well as know when to seek the expertise of another team member (Al-Mousawi, Mecott-Rivera, Jeschke, & Herndon, 2009).
- Nurses: Are the largest portion of the members of the burn teams. Are involved with daily care for the patients. The nurses are constantly monitoring the patients to see if anything changes. Both practical and research nurses are a part of burn teams (Al-Mousawi et al., 2009).
- Anesthesiologists: When the severity of burns is high, the burn team will look towards an anesthesiologist to assist with treating the patient. Issues with airways, ventilation, heat-loss, fluid and electrolyte balance, and circulatory instability will be addressed to help improve the treatment and recovery (Al-Mousawi et al., 2009).
- Respiratory Therapists: Often when a severe burn injury inflicts the lungs, respiratory therapists get involved with the treatment. They help with the breathing injury, mechanics and sepsis, as well as the respiratory systems inflammatory response to the burn. While helping treat the patients they utilize a protocol-based approach (Al-Mousawi et al., 2009).
- Occupational/Physical Therapists: Once the treatment is complete, depending on the extent of the burn the individual may need some form of rehabilitation. Occupational and physical therapists will give the patient a personalized program to follow to help improve recovery. If the program is followed through over the correct period of time the patient may get back to functioning the way he or she used to (Al-Mousawi et al., 2009).
- Dietician: Major burns cause the body to use a lot of its energy stores in order to respond to the infliction. With this in mind, the patient may be lacking important nutrients. A dietician or nutritionist will be responsible for implementing and monitoring nutritional intake for the patients to get the nutrients they need as well as speed up recovery (Al-Mousawi et al., 2009).
- Psychosocial Experts: Not only do burns have an impact on the physical body but also psychologically due to the trauma associated with the burn injury. Psychological experts like psychologists, psychiatrists and social workers will be consulted to help the patient and their loved ones response to the injury and the transition period. Making sure the patient has an improved mental state is needed to help with pain tolerance, anxiety, motivation and care not just during treatment, but after as well (Al-Mousawi et al., 2009).
Prevention
Providing adequate burn care in the Western world costs around $1000 US dollar per patient per day (Atiyeh et al.,2009).. This is not an ideal situation for those in developing countries and emphasizes the fact that prevention is a primary means to reduce burn-related death and disabilities. Barriers to prevention in developing countries also include having limited resources, limited knowledge in regards to first-aid treatment and inaccessibility to modern medicine (Atiyeh et al.,2009).. The primary target group of prevention efforts should be children from a lower socioeconomic status. This group is the largest and most vulnerable group for burn injuries. It is important to recognize that many of the risk factors associated with burn injuries cannot be modified easily or quickly and thus a multifaceted solution is needed for burns prevention. A multifaced solution requires the help of health workers to promote burn prevention along with programs implemented to help fight issues such as educational deficits, poverty, overcrowding, and poor housing (Atiyeh et al.,2009).
Atiyeh et al. (2009) highlight three main strategies that aim to reduce harm from injuries which include education, product design and environmental change, and legislation and regulation. In the strategies figure, strategies to reduce harm from injuries emphasize an active and passive approach. The educational strategy is an active approach focused on the individual (host) to help them avoid injury by modifying their environment to reduce the likelihood of injury. By knowing the environmental risks, it is more likely that preventative behavior will happen in an individual. Passive injury prevention involves product and environment modification. Product modification can be influenced by education the public to ask for safer products, and they can create pressure on authorities to produce prevention legislations (Atiyeh et al.,2009).
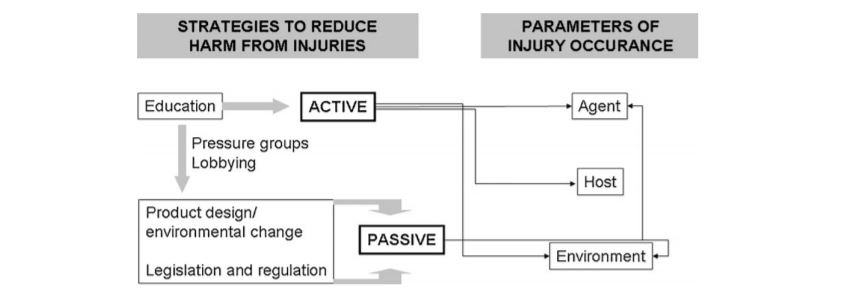 Figure. 8 – Strategies to reduce harm from injury (Atiyeh et al., 2009)
Figure. 8 – Strategies to reduce harm from injury (Atiyeh et al., 2009)
Home Prevention Strategies
There are many tips that can be applied to help prevent home burns. For example, in the kitchen, one should never leave the stove turned on unattended (“Burns Prevention”, 2017). It is important to pay attention when the stove is on and not be distracted to do other chores. Also, it is a good habit to turn the handles of pots and pans inward when cooking so that it can't be knocked over. When using the microwave, you should open the lid of a container slowly after it has been heated up in the microwave so that the stream can’t burn you (“Burn Prevention and Fire Safety Tips”, 2017). In the bedroom and living rooms, keep outlets and extension cord away from flammable areas. If there are any unused outlets, you should take extreme precaution and use safety caps. Lastly, if there are any electronic appliances such as an iron or curling iron that you aren't using, then it should be unplugged (“Burns Prevention”, 2017).
Workplace Prevention Strategies
When discussing workplace prevention strategies, it is heavily dependent on the workplace and work environment. People will have different workplace prevention strategies for burns that cater to their specific work environment. For example, someone working in construction will have to be caution of flammable solutions and dress appropriately according to the weather. Compared to a restaurant personnel, who would have to pay extra attention when serving hot beverages to customers. A general tips for everyone in the workplace including being aware of hazards that can cause burns, do not attempt any tasks that you are uncomfortable with or feel that can harm you and ask for assistance/further instruction when required.
Children Prevention Strategies
It is important to take extra caution if you have children in your house. According to the American Burn Association in 2015, 95% of burns to young children our at home (“Prevention Poster Contest Winners”, 2015). Therefore, some basic steps to help prevent burns include have a no kids zone where kids have to stay at least 3 feet away so that you can use hot item etc. Also, check the temperature of the water before placing children into bath. Keep lighters and matches in an area that children cannot reach (ex. Top shelves). Do not let children carry hot liquid such as a full cup of hot chocolate without a lid because they may split it on themselves (“Stanford Children's Health”, 2017).
Additional General Prevention Strategies Tips for Everyone
- Use sun protection when going outdoors for a prolong period of time
- If you get a severe burn, seek medical attention as soon as possible
Presentation
References
Al-Mousawi, A. M., Mecott-Rivera, G. A., Jeschke, M. G., & Herndon, D. N. (2009). Burn teams and burn centers: the importance of a comprehensive team approach to burn care . Clinic Past Surgery , 36 (4), 547-554.
Artuson, G. (1980). Pathophysiology of the burn wound. Ann. Chir. Gynaecol. 69(5): 178-90. Burn | First Degree Burn | Second Degree Burn | MedlinePlus. (n.d.). Retrieved November 15, 2017, from https://medlineplus.gov/burns.html
Burn Prevention and Fire Safety Tips. (2017). Barnabas Health. Retrieved 15 November 2017, from http://www.barnabashealth.org/Saint-Barnabas-Medical-Center/Our-Services/The-Burn-Center/Community-Outreach/Burn-Prevention-and-Fire-Safety-Tips.aspx
Burns - Causes, Symptoms, Treatment, Diagnosis - MedBroadcast.com. (2017). Medbroadcast.com. Retrieved 22 November 2017, from http://www.medbroadcast.com/condition/getcondition/burns
Burns Prevention. (2017). Mayo Clinic. Retrieved 15 November 2017, from https://www.mayoclinic.org/diseases-conditions/burns/basics/prevention/con-20035028
Cutaneous burns Etiology - Epocrates Online. (2017). Online.epocrates.com. Retrieved 22 November 2017, from https://online.epocrates.com/diseases/41224/Cutaneous-burns/Etiology
Edwards, D., Heard, J., Latenser, B. A., Quinn, K. Y., van Bruggen , J., & Jovic, G. (2011). Burn injuries in Eastern Zambia: Impact of Multidisciplinary Teaching Teams . Burn Care & Research , 32 (1), 31-38.
Epidemiology of burn injuries globally. (2017). Uptodate.com. Retrieved 22 November 2017, from http://www.uptodate.com/contents/epidemiology-of-burn-injuries-globally
Everything You Need to Know About Ice Burn. (2017). Healthline. Retrieved 22 November 2017, from https://www.healthline.com/health/ice-burn#overview1
Herndon, D. N., Lemaster, J., Beard, S., Bernstein, N., Lewis, S. R., Rutan, T. C., . Osten, T. V. (1986). The Quality of Life after Major Thermal Injury in Children. The Journal of Trauma: Injury, Infection, and Critical Care, 26(7), 609-619. doi:10.1097/00005373-198607000-00004
Johns Hopkins Medicine. (2017). Burns. Hopkinsmedicine.org. Retrieved 19 November 2017, retrieved from https://www.hopkinsmedicine.org/healthlibrary/conditions/dermatology/burns_85,P01146
Kagan, R.J., Peck, M.P., Ahrenholz, D.H., Hickerson, W.L., Holmes, J.H., Homles, J.H., Korentager, R.A., Kraatz, J.J., Kotoski, G.M. (2009) Surgical Management of the Burn Wound and Use of Skin Substitutes. American Burn Association.
Khan, A., & Solan, M. (2016, April 26). Burns: Types, Treatments, and More. Retrieved November 15, 2017, from https://www.healthline.com/health/burns
Krob, MJ; d'Amico, FJ; Ross, DL (1991). “Do trauma scores accurately predict outcomes for patients with burns?”. The Journal of burn care & rehabilitation. 12 (6): 560–3. PMID 1779010. doi:10.1097/00004630-199111000-00011.
Lawrence JW, Mason ST, Schomer K, Klein MB. (2011). Epidemiology and impact of scarring following burn injury: A systematic review of the literature. J. of Burn Care & Research, 33(1), 136-46.
Peck, M. D. (2011). Epidemiology of burns throughout the world. Part I: Distribution and risk factors. Burns, 37(7), 1087-1100.
Plastic Surgery for Burns and Other Wounds. (2017). WebMD. Retrieved 22 November 2017, from https://www.webmd.com/skin-problems-and-treatments/plastic-surgery-burns#1
Prevention Poster Contest Winners. (2015). Ameriburn.org. Retrieved 15 November 2017, from http://ameriburn.org/prevention/prevention-resources/2015-poster-contest/
Skin graft Information | Mount Sinai - New York. (2017). Mount Sinai Health System. Retrieved 22 November 2017, from http://www.mountsinai.org/health-library/surgery/skin-graft
Stanford Children's Health. (2017). Stanfordchildrens.org. Retrieved 15 November 2017, from http://www.stanfordchildrens.org/en/topic/default?id=preventing-burn-injuries-90-P01750
Thermal Burns: Overview, Pathophysiology, Quantifying Burn Severity. (2017). Emedicine.medscape.com. Retrieved 22 November 2017, from https://emedicine.medscape.com/article/1278244-overview
World Health Organization. (2017). Burns. Retrieved November 10, 2017 from World Health Organization : http://www.who.int