This is an old revision of the document!
Table of Contents
Osteoporosis
History
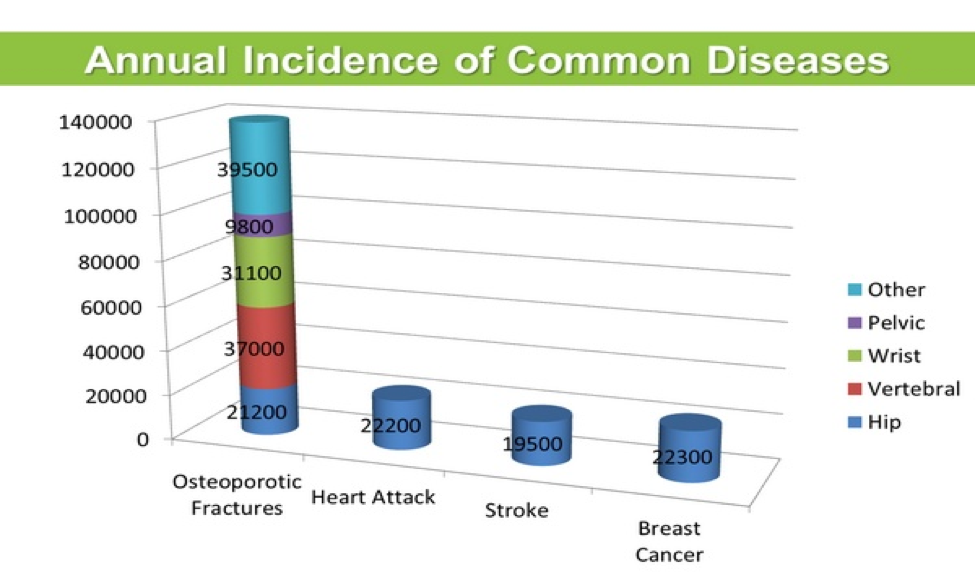
Osteoporosis is a medical condition characterized by low bone density and deterioration of bone matrix in connective tissues (Melton, 2001). Osteoporosis usually occurs after 50 years of age and impacts millions of Canadians and people around the globe. Osteoporosis induced injuries can result in prolonged hospitalization, decreased independence, higher incidence of depression, and a reduced quality of life (Iqbal, 2000). Osteoporosis results in significant personal and economic damage, with estimated costs of a yearly $13.8 billion for direct medical treatment in the United States (Iqbal, 2000). Research shows that approximately 20% of men over 50 years old are diagnosed with osteoporosis of the hip, spine or wrist. Furthermore, about 50% of women will suffer an osteoporotic fracture at some point in their life. The World Health Organization defines osteoporosis on the basis that an individual has a bone mineral density (BMD) of more than 2.5 standard deviations below the normal mean. Particularly, postmenopausal women have higher risks of developing osteoporosis due to declines in estrogen levels. A survey by the National Health and Nutrition institute in the United States, revealed that 20% of white postmenopausal women had osteoporosis of the femoral neck compared to 10% of Hispanic women and 5% of African-American women. In this same study, the prevalence of osteoporosis among white, Hispanic, and African-American men was 4%, 2%, and 3%, respectively (Melton, 2001). The following figure shows the annual incidence of common diseases in Canada and it is clearly evident that osteoporotic fractures are more common than heart attacks, stroke and breast cancer (Grant, 2015).
Risk Factors
Osteoporosis can happen due to insufficient adolescent bone density, fluctuation in hormone levels leads to imbalances and an overall nutrient-poor diet. During adolescence or puberty, bone density continuously increases and peak levels are reached when an individual is in their early 20’s. Following this age, osteoclast activity tends to surpass the osteoblast activity and rate of bone formation declines. Studies have revealed that a low peak bone density during puberty may induce a greater risk of developing osteoporosis when one is an adult (Schettler & Gustafson, 2004). Hormonal imbalances can occur because of an overactive or underactive thyroid and this phenomenon can in turn increase susceptibility to osteoporosis. Moreover, males who have low testosterone levels and females who have low estrogen levels, have a significantly greater risk of developing osteoporosis. A diet that is poor in Vitamin D or calcium can significantly decrease bone density (Larsen, Mosekilde & Foldspang, 2003). Calcium is deposited into trabecular bone during osteogenesis and without this essential element, bone growth occurs significantly slower and the overall structure may turn unstable. Vitamin D is essential for the small intestines as they use this vitamin to absorb calcium which is in turn supplied to the bones via the blood stream. Therefore, Vitamin D is vital to bone growth and insufficient amounts are indeed risk factors for osteoporosis.
Signs and Symptoms
For individuals that have osteoporosis, treating this disease early on is the best way to prevent more serious risks, but being able to detect bone loss signs early on is really unusual (Minnis, 2016). A couple signs that have been visible for individuals with osteoporosis in the early age include having a weaker grip strength, weaker fingernails, and receding gums (Minnis, 2016). As the individual enters a later stage of osteoporosis, an increase in bone loss is observed (Minnis, 2016). At this stage, the individual begins to observe more obvious signs (Minnis, 2016). These signs include neck and back pain, fractures that occur from a fall, getting a hunched back, and a loss of height (Minnis, 2016). For individuals with osteoporosis, areas of fracture include hip, wrist, and spine (Minnis, 2016).
Diagnosis
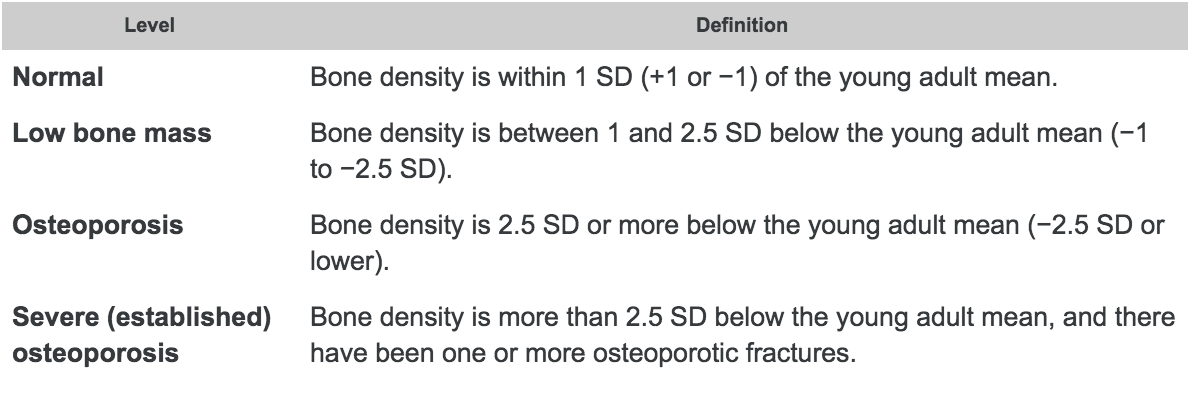
The bone mass density, also known as BMD, is the primary test that can be used to determine the bone strength using a dual X-ray absorptiometry. The scanned bone from either the hip or spine from an individual can determine the bone density to determine the diagnosis as well as any future fracture risks (Sozen, Ozisik, and Calik 2017). The World Health Organization (WHO) presents that osteoporosis is determined when an individual has 2.5 standard deviation below the average using a T-score. This can be performed from knowing the difference between the patient’s BMD and the average to compare with the severity of the diagnosis (Sozen, Ozisik,and Calik 2017). The results are usually compared to a healthy 30-year old adult’s bone mineral density. Therefore, a lower BMD number will indicate a higher risk of a fracture (National Resource Center, 2015).
Figure 5: A table demonstrating the comparison of standard deviations created by the World Health Organization (WHO).
Screening & Measuring Tools
Dual-energy x-ray absorptiometry (DEXA) is a method that can be performed on different areas to determine osteoporosis with a low radiation dose. This method consists of two energies where the x-ray goes across the desired area. Areas often included are the lumbar spine and proximal femur. However, if these areas are unavailable, the forearm can also be used to scan for BMD measurement (Ramos et al., 2011).
Another method used to determine osteoporosis is determined using blood tests or bone biopsies. Blood tests are able to indicate certain proteins such as alkaline phosphatase. An individual with a higher amount of alkaline phosphatase has a higher indication with certain bone diseases. Calcium levels in the blood can also indicate if an individual has enough calcium intake (Institute for Quality and Efficiency in Health Care, 2017).
Pathophysiology
Osteoporosis is a systemic disease of the bones characterized by a low skeletal bone density and mass, as well as deterioration of bone tissues. Together, these cause an individual with osteoporosis to have an increased risk of bone fracture (Garnero, 2008).
That being said, there are two classifications of osteoporosis identified; primary and secondary. Most commonly seen is primary osteoporosis which includes type 1 and type 2 which are postmenopausal osteoporosis and senile osteoporosis, respectively. On the other hand, secondary osteoporosis is characterized by bone mass loss from certain diseases. In addition, secondary osteoporosis is also caused from poor health choices like smoking and consumption of alcoholic beverages. Within primary osteoporosis, type 1 is associated with a loss of the hormones, estrogen and androgen, leading to increased bone turnover, bone resorption exceeds bone formation and dominant loss of trabecular bone rather than cortical bone. Type 2 osteoporosis is defined by predominant loss of cortical bone, and results from age related bone loss caused by systemic senescence and is induced by loss of stem-cell precursors (Dobbs, Buckwalter, & Saltzman, 1999).
Around the ages between 40 and 50, bone mass starts to decrease in both men and women at a yearly rate of 0.3 to 0.5 percent. In fact, postmenopausal women experience an increase in the loss of bone mass by as much as 10 times. Similarly, this increased rate also occurs in men after castration, when there is loss of function of the testicles (Dobbs, Buckwalter, & Saltzman, 1999).
Treatments - Prevention & Management
Unfortunately, there is no cure for osteoporosis as it is a symptom from ageing, however there are many prevention and management methods to reduce its severity. Thus, the current treatment methods are targeted at preventing the progression of osteoporosis, which include changes to one's lifestyle and drugs that reduce bone loss, increase bone strength and bone formation (Kling, Clarke, & Sandhu, 2014).
Lifestyle
There are many lifestyle modifications that individuals can engage in to reduce the detriments of osteoporosis and prevent its progression. Since one component of bones is calcium, one recommendation is to include more foods rich in calcium in one’s diet. Some examples of calcium rich foods are dairy products like milk or yogurt, leafy dark green vegetables, nuts and calcium-fortified foods. Additionally, there are calcium supplements available like calcium citrate and calcium carbonate that an individual can take. Together, these foods and supplements will aid in building bone strength and reducing the progression of osteoporosis (NYU Langone Health, n.d.).
Another vitamin that will help in preventing osteoporosis from progressing is vitamin D. Similar to calcium, there are foods and supplements available that an individual with osteoporosis can take. Examples include fatty fish like tuna or salmon, beef liver, cheese and egg yolks, as well as vitamin D supplements one can obtain over the counter. That being said, vitamin D works by promoting calcium absorption in the intestines and aids in the maintenance of balanced calcium levels. Moreover, vitamin D supplements can be taken in combination with calcium rich foods or supplements to increase the efficiency of calcium absorption (NYU Langone Health, n.d.).
Lastly, a healthy and physically active lifestyle is highly recommended for someone with osteoporosis, especially exercises involving the use of small weight. Some examples of exercises individuals can partake in are dancing, walking, jump rope, hiking, and stair climbing. These exercises can aid in increasing bone strength and stimulating bone growth. In addition, health practitioners recommend that individuals suffering from osteoporosis should avoid smoking and consume no more than two alcoholic drinks per day as both decrease bone density and increase fracture risk (NYU Langone Health, n.d.).
Drugs and Medication
As of now, the most effective drugs for osteoporosis are antiresorptive agents, meaning they decrease the amount of calcium removed from bones. Since bones are dynamic and constantly being remodelled, and osteoporosis results when bone resorption is higher than bone rebuilding, these medications inhibit the removal of bone so bone rebuilding is favoured. Many antiresorptive agents are available including alendronate, risedronate, raloxifene and others (Lewiecki, 2004).
Bisphosphonates are a class of antiresorptive drugs that are used to decreases risks of fractures of hip, wrist, and spine. These class of drugs are all administered orally to reduce adverse side effects, and to enhance the absorption of the medicine. They are taken in the morning and are taken with water to increase absorption. They can also be administered intravenous to avoid possible stomach problems (Lewiecki, 2004).
Alendronate (Fosamax) is an example of a bisphosphonate drug. It is effective treatment for postmenopausal osteoporosis as well as with glucocorticoid induced osteoporosis. This drug, similar to other bisphosphonates increases bone density and reduces various possible fractures. It is taken orally once a week for postmenopausal osteoporosis and is also the first drug used for increasing bone density in males with osteoporosis. This drug as all others does have a few side effects. This includes irritation of the esophagus or even inflammation of the esophagus. Differences in the chemical makeups of the other bisphosphonate drugs is what allows for certain side effects to be avoided (Gronholz, 2008).
Zoledronate (Reclast) is an intravenous administered bisphosphonate that is given once a year. It is able to effectively strengthen bones along with preventing both spinal and non-spinal fractures. As with all medications, side effects of this drug may result in muscle and joint aches, and so mild pain killers are given following treatment. This drug is used mainly to prevent postmenopausal osteoporosis and to increase bone mass in males suffering the disease (Gronholz, 2008).
Conclusion
Osteoporosis is set to become a major health concern with an ageing population. Scientists have identified human stem cells that develop into the bone, cartilage, and other tissues that make up the body’s skeleton (Price et al., 2018). This will one day help doctors repair or replace joint cartilage, heal broken bones more quickly, and build up bone in osteoporosis patients. Additionally, a new genetic screen may predict a person’s future risk of osteoporosis and bone fracture and may allow for more preventative measures (University of Stanford, 2018).
References
Grant, S. (2015). November is Osteoporosis Month. Retrieved March 5, 2019, from http://www.proofofcare.com/2015/11/november-is-osteoporosis-month/
Iqbal, M. M. (2000). Osteoporosis: epidemiology, diagnosis, and treatment. Southern Medical Journal, 93(1), 2–18. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10653058
Larsen, E. R., Mosekilde, L., & Foldspang, A. (2003). Vitamin D and Calcium Supplementation Prevents Osteoporotic Fractures in Elderly Community Dwelling Residents: A Pragmatic Population-Based 3-Year Intervention Study. Journal of Bone and Mineral Research, 19(3), 370–378. https://doi.org/10.1359/JBMR.0301240
Melton, L. J. (2001). The Prevalence of Osteoporosis: Gender and Racial Comparison. https://doi.org/10.1007/s00223-001-1043-9 Schettler, A. E., & Gustafson, E. M. (2004). Osteoporosis Prevention Starts in Adolescence. Journal of the American Academy of Nurse Practitioners, 16(7), 274–282. https://doi.org/10.1111/j.1745-7599.2004.tb00450.x