Table of Contents
Diabetes Mellitus
Introduction
Diabetes mellitus (commonly referred to as diabetes) is a group of metabolic disorders caused by defects of insulin secretion. The prevalence of this disease has skyrocketed since the beginning of the 21st century, becoming the seventh most common global cause of death in 2016 (World Health Organization, 2018). This increase is most likely due to the lifestyle shift in North American and European countries. The domination of fast food chains and increased automation in the workplace and streets has lead to a decrease in physical activity and healthy eating habits.
There are four major categories of this disease: Type 1 diabetes, Type 2 diabetes, gestational diabetes, and specialized types of diabetes (Egan and Dinneen, 2014). Type 1 diabetes is caused by the destruction of pancreatic β-cells. The most common method of destruction being facilitated by the body’s inflammatory response. Type 2 diabetes is caused by insulin resistance, which is mediated by dysfunctional pancreatic β-cells. Gestational diabetes occurs when the onset of diabetes is during pregnancy. The final major category of diabetes (specialized types) encompasses a large variety of diseases that can be categorized as diabetes but have different onsets and mechanisms from the first three categories. The most common example is maturity-onset diabetes of the young (MODY), which is an inherited form of diabetes and associated with mutations in hepatic genes (Egan and Dinneen, 2014).
The focus of this wiki page will be on Type 1 and Type 2 diabetes, where risk factors, symptoms, diagnosis, epidemiology, etiology, pathophysiology, and treatment methods will be discussed.
Epidemiology
The global prevalence of diabetes has been steadily increasing and on the rise. With increased availability of fast foods and unhealthy options, this causes an increase in poor health behaviours, raising a big concern. Based on previous data that captures future trends in diabetes frequency, the number of adults with diabetes globally has been projected to increase from 382 million to 592 million by 2035 (Forouhi & Wareham, 2014). The epidemiology of diabetes varies depending on different factors such as the type of diabetes, sex, age, geography, ethnicity and genetics.
Type 1 diabetes: It has been shown that in most populations, the highest incidence of type 1 diabetes is in between birth and 14 year old children (Forouhi & Wareham, 2014). More specifically, the geographical location has an impact on the incidence of type 1 diabetes in children, with Finland having the highest incidence and Venezuela having the lowest. In general, countries in Europe and North America had higher incidences of type 1 diabetes in children under the age of 14 compared to countries in south America and Asia (with Kuwait as an exception) (Forouhi & Wareham, 2014). It has also been shown that males are slightly more prevalent to type 1 diabetes than women (Forouhi & Wareham, 2014).
Type 2 diabetes:
Individuals with type 2 diabetes account for more than 85% of the total cases of diabetes (Forouhi & Wareham, 2014). Similar to type 1 diabetes, the prevalence of type 2 diabetes varies according to geographical locations. It has been shown that western countries and ethnic groups that have developed a western diet, have the highest prevalence of type 2 diabetes (Forouhi & Wareham, 2014). These countries include different regions in USA, China and India. In fact, the prevalence of type 2 diabetes in China is projected to increase from 98.4 million to 142.7 million by 2035 (Forouhi & Wareham, 2014). Developing countries on the other hand, have the lowest prevalence of type 2 diabetes, specifically in rural areas such as the Mapuche Indian region in Chile. The prevalence of type 2 diabetes increases quickly with age in both genders (Forouhi & Wareham, 2014).
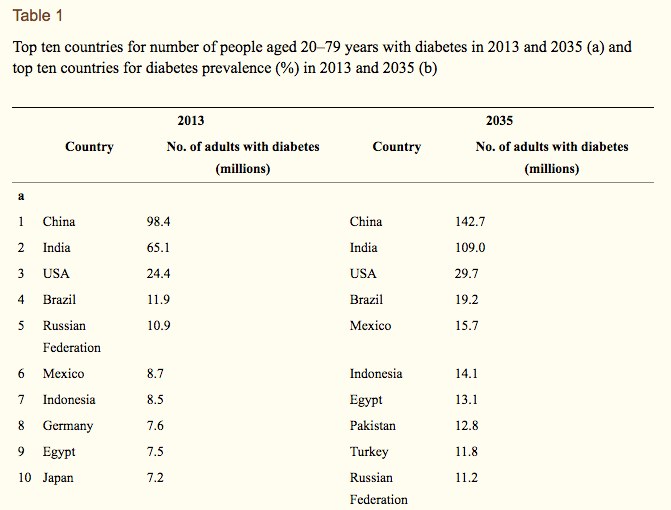
Figure 1: Top ten countries for number of people with diabetes aged between 20–79 years in 2013 and 2035. (Forouhi & Wareham, 2014)
Etiology
Causes of Type 1 Diabetes:
The pancreas contains beta cells capable of producing insulin, type 1 diabetes occurs when the body´s immune system attacks these cells (National Institute of Diabetes and Digestive and Kidney Diseases [NIDDK], 2016). This autoimmune destruction is initiated by an interaction between genetics and the environment.
Epidemiological evidence supports the theory that an environmental influence, viruses, have a role in type 1 diabetes. This is demonstrated by the evidence indicating that regional differences in the prevalence of enterovirus infections have been correlated to type 1 diabetes (Yeung, Rawlinson, and Craig, 2011).
These infections are spread through infected feces and respiratory particles and have a higher chance of contributing to autoimmunity or type 1 diabetes in those with genetic risk factors (Yeung, Rawlinson, and Craig, 2011). Specifically, studies have shown children with autoimmunity affecting the pancreas had 3 times the probability to develop an enteric infection (Yeung, Rawlinson, and Craig, 2011).
Other environmental triggers include the presence of vitamin D deficiency, cow milk, and other dietary factors as well as chemical or cytotoxic factors in an individual´s early life (Teddy Study Group, 2008).
When investigating genetic factors, 18 regions of the genome are associated with type 1 diabetes including the IDDM1 region and the HLA region of genes. For instance, an autoimmune response destroying pancreatic beta cells is triggered by certain alleles of HLA genes encoding MHC proteins. These affect the coding of the proteins, making the proteins appear unrecognizable to the body´s immune system (Dean and McEntyre, 2004).
Causes of Type 2 Diabetes:
Genetic and environmental factors contribute to the causation of type 2 diabetes, the most common type of diabetes (NIDDK, 2016). Those who have obesity or are overweight, have a propensity for diabetes due to insulin resistance that can be caused by chronic inflammation (NIDDK, 2016). Insulin resistance begins with the body´s pancreas producing more insulin to help glucose enter cells when muscle, liver and fat cells are not able to use insulin well enough (NIDDK, 2016). However gradually, the body cannot produce enough insulin leading to an increase in blood glucose levels (NIDDK, 2016).
Apart from obesity, other environmental factors include the occurrence of metabolic syndrome, the impact of age and an inactive lifestyle (Eckel, 2008).
On the other hand, when examining genetic factors, research has shown certain gene variants can lead to the susceptibility of type 2 diabetes. However, the incidences are small, ranging from 5-10% (McCarthy, 2010).
Risk Factors
The risk factors for Type 1 diabetes are currently unknown. However, researchers have determined that the likelihood of developing Type 1 diabetes increases if one has a relative with the disease. Thus, implying a genetic connection. On the other hand, the risk factors Type 2 diabetes have been extensively researched. High blood pressure, high blood cholesterol levels, having a family member with diabetes, being overweight, taking glucocorticoid medications, being diagnosed with a psychiatric disorder (e.g. schizophrenia, depression), being a member of an at-risk ethnic group (e.g. African, Asian), and belonging to a lower socioeconomic group all contributes to the risk of developing Type 2 diabetes (Canadian Diabetes Association, 2018).
Symptoms
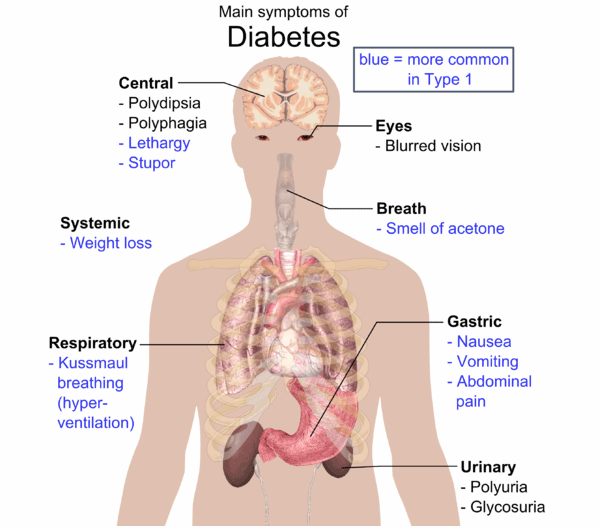
The most common symptoms of Diabetes Mellitus are increased hunger (polyphagia), increased urination (polyuria) and increased thirst (polydipsia), which result due to rapid development of hyperglycemia (high blood sugar). Other symptoms include lethargy, blurred vision, slow healing, sudden weight loss (mainly in Type 1) and numbness in the hands/feet (mainly in Type 2) (“American Diabetes Association”, 2017).
Figure 2: Overview of common symptoms seen in both T1DM and T2DM
Polyphagia is often experienced by diabetic patients due to reduced absorption of glucose by the cells in their body. The reduced intake of glucose by the cells can either be as a result of insufficient amount of insulin or insulin resistance. Insulin insufficiency is seen in Type 1 diabetes whereas insulin resistance is seen in Type 2 diabetes. Either way, cell absorption of glucose will not take place and glucose will accumulate in the bloodstream. Ultimately, the glucose deprived cells signal the brain for more food intake even if food was recently ingested. Thus, resulting in excessive eating (Ramachandran, 2014).
Polyuria occurs when the concentration of the filtered load of glucose goes above 10 mmol/L, exceeding the capacity of the kidney tubules to reabsorb glucose due to the saturation of the transport proteins. This results in glucose being found in the urine. Furthermore, water is drawn to glucose through osmosis and thus produces excessive glucose-containing urine. This in turn results in polydipsia as the body becomes dehydrated. Weight loss is another classic symptom due to catabolism as the body seeks for energy through breakdown of muscles and fat (Ramachandran, 2014).
It is also important to notice that many of the symptoms for type 2 diabetes are so mild that it can go unnoticed. While symptoms for Type 1 can go unnoticed as well, it is less likely to do so. Therefore, it is imperative to consult a doctor immediately, if any of these symptoms are present. Although there are several similarities between Type 1 and Type 2 diabetes, the cause and treatment for them are different (“MNT”, 2016).
Diagnosis
There are several methods and tests available to screen for diabetes. The most common method is the use of blood tests. A blood test measures high blood glucose levels, which are known to be an indication of diabetes. A total of two abnormal blood tests are required for an official diagnosis for diabetes.
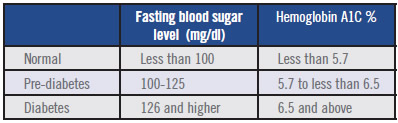 Figure 3: The ranges of blood glucose measures in an A1C test and a Fasting blood test used to diagnose diabetes.
Figure 3: The ranges of blood glucose measures in an A1C test and a Fasting blood test used to diagnose diabetes.
A1C Test: A common blood test that is usually used to screen for diabetes, is the glycated hemoglobin test (A1C). This blood test measures the blood glucose that is attached to hemoglobin. The more there is blood glucose attached to hemoglobin, the higher the level of plasma glucose. In general, an A1C range of 7.5-6.4% indicates prediabetes. And a measure of 6.5% or higher on two A1C tests is an indication of diabetes (2. Classification and Diagnosis of Diabetes, 2014).
Some patients are not able to get an A1C test done for various reasons , therefore a normal blood glucose test can be done for a diagnosis. A plasma glucose test can be done while fasting or non-fasting (random blood glucose count).
Fasting: This blood test measures the fasting blood glucose levels. A fasting blood glucose range of 100-125 mg/dL is considered as prediabetes. A result of 126 mg/dL or higher of fasting blood glucose levels is an indication of diabetes (Diagnosis and Classification of Diabetes Mellitus, 2009).
Non-Fasting: This blood test measures the blood glucose levels at any random time. A random blood glucose levels of 200 mg/dL or higher suggests diabetes (Diagnosis and Classification of Diabetes Mellitus, 2009).
Pathophysiology
Type 1 Diabetes
T1DM is characterized by autoimmune destruction of pancreatic β-cells by CD4+ and CD8+ T-cells and macrophages infiltrating the islets which leads to a deficiency of insulin secretion. Majority of the patients have detectable anti-insulin antibodies and approximately 85% of T1 diabetics have circulating islet cell antibodies. Most of which are directed against GAD (glutamic acid decarboxylase) within pancreatic β-cells (Baynest, 2015). Insulitis with gradual β-cell destruction leads to pre-diabetes and finally to overt DM. These patients are susceptible to other autoimmune diseases, such as Addison’s disease, celiac disease, myasthenia gravis and Hashimoto’s thyroiditis (Siddiqui et al., 2004). There is also excessive secretion of glucagon due to the abnormal function of pancreatic α-cells in T1DM patients. The improperly increased glucagon levels in turn worsens the metabolic defects due to insufficient insulin. Insulin deficiency leads to hyperglycemia and then increased levels of free fatty acids in the plasma due to irrepressible lipolysis, which then suppresses glucose breakdown in the skeletal muscle. This impairs glucose utilization and causes insulin insufficiency to reduce the expression of important genes for target tissue to respond normally to insulin such as GLUT 4 class of glucose transporters in adipose tissue and glucokinase in liver (Baynest, 2015).
Type 2 Diabetes
T2DM is characterized by two main pathological defects: impaired insulin action due to insulin resistance and impaired insulin secretion due to the dysfunction of the pancreatic β-cell (Baynest, 2015). Moreover, chronic food oversupply is the primary reason for pancreatic β-cell failure and onset of T2DM in susceptible individuals. Unsusceptible chronically over-nourished individuals remain resistant to T2DM by disposing excess calories to subcutaneous adipose tissue rather than to the skeletal muscle, liver or islet β cells. Whereas, susceptible over-nourished individuals develop T2DM as a result of failing to dispose excess calories safely to the subcutaneous adipose tissue and instead to the visceral adipose tissue such as the skeletal muscle, liver, and pancreas which cause severe tissue damage. As a result, there is increased glucagon secretion and reduced incretin response; impaired expansion of subcutaneous adipose tissue, inflammation of adipose tissue and development of peripheral insulin resistance. Deteriorating islet β-cell function can lead to the need for insulin therapy (Siddiqui et al., 2004).
Mechanisms
The primary regulator of blood glucose uptake is the hormone Insulin. Insulin most commonly acts upon the IGF-1 receptor located across the cell membrane (Siddiqui, 2013). A Deficiency of insulin or an issue with its receptors therefore plays a major role in the development of all types of diabetes.
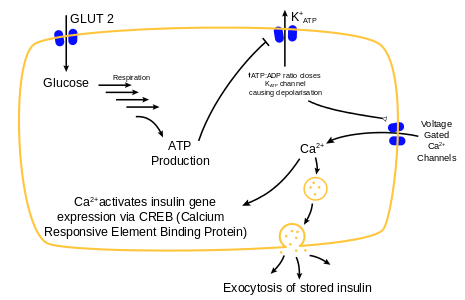
Insulin Signal Transduction Pathway
Insulin is released into the bloodstream from β-cells located in islets of Langerhans, a region of the pancreas. When a rise in blood glucose occurs, glucose enters the β-cell through the GLUT-2 inter-membrane receptor. It is then through a signal transduction cascade that voltage-gated calcium ion channels open, allowing extracellular calcium ions to enter the cell. Ca2+ can then activate insulin-gene expression via CREB (Calcium Responsive Element Binding Protein). At the same time, Ca2+ binds to insulin storing vesicles, which causes exocytosis of the insulin in the bloodstream (Siddiqui, 2013).
Figure 4 Insulin release pathway of pancreatic β-cells
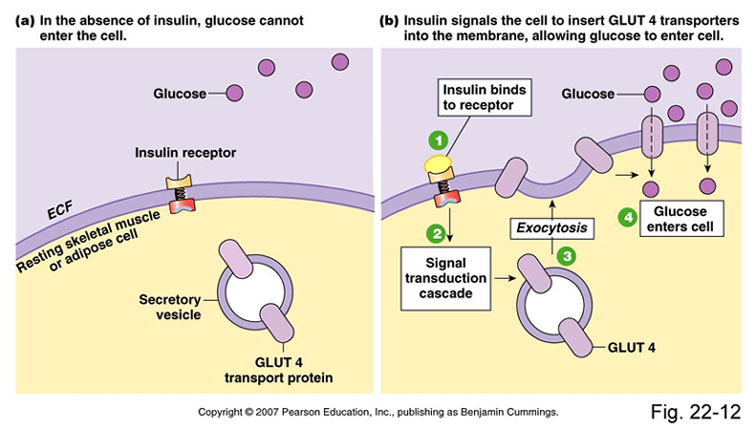
Upon reaching the target cell, Insulin can then bind to the extracellular portion of the IGF-1 tyrosine receptor kinase. Through a signal transduction cascade, vesicles containing GLUT-4 inter-membrane transport proteins are secreted to the cell membrane, where glucose enters through passive diffusion (Siddiqui, 2013).
Figure 5 Target cell response to insulin signalling
Relevance to Diabetes Type I and II
It is at two places in the insulin signaling mechanisms that issues can occur. Within the islets of Langerhans, insulin can either being produced in minimal quantities or none at all. This could be caused by numerous issues, such as lack of insulin-gene expression, improper transcription, translation, or folding of the protein, and non-functioning β-cells to name only a few.
At the target cells. Insulin may be non-functioning when binding to IGF-1 receptors. Like all proteins, there are numerous places in the protein biosynthesis pathway that can cause a malfunction in the proteins or an absence of protein production.
Treatment
Management
Diabetes is a chronic disease, meaning that there is no known cure. However, there are ways to actively manage and control the disease through factors such as lifestyle choices and medication. The most frequent method of management is controlling blood sugar levels. The goal of management is to keep blood sugar within a range close to what would be considered normal, without causing low blood sugar (National Institute for Health and Clinical Excellence, 2008). Once diagnosed, the patient must go through significant lifestyle changes, such as losing weight, increasing activity, switching diets, insulin injections as well as oral medications in the case of type II diabetes (Haw, 2017).
A major part of the disease treatment is through education. Since the progress of the disease depends a lot on personal lifestyle choices, it is important that patients continue learning and actively taking part in their treatment program.
Medication
Medications used to treat diabetes act on lowering blood sugar levels. There are different types of anti-diabetic medications. Oral medication, such as metformin, is commonly prescribed while others are administered by injections. Type 1 diabetes can only be treated with insulin, either through insulin injections or insulin analogs (National Institute for Health and Clinical Excellence, 2008).
Surgery
Weight loss surgery is usually recommended for obese patients to promote long term blood glucose control. Operations such as gastric bypass may be conducted in order for patients to gain more control over their weight (Mottalib, 2017). Post-operation, many patients are able to control their blood glucose without the use of any medication. Long term mortality and complications from both diabetes and obesity are also decreased. However, around 1% of patients have increased short term risks of mortality post surgery (Mottalib, 2017). Usually, this surgery is considered for patients that are unable to get both blood sugar and weight under control.
Under certain circumstances, a pancreas transplant may be considered for patients suffering from type I diabetes. However, transplants are usually reserved for cases where a person may be suffering from severe complications, such as organ failure.
Prevention
Type I diabetes has no known means of prevention, however Type II diabetes can either be prevented or delayed through healthy lifestyle choices such as exercise, healthy diets, and maintaining a healthy body weight. Decreasing sugar intake and increasing foods rich in fiber have been known to decrease risk factors. Consuming less saturated fats along with quitting smoking have also shown to decrease type II diabetes risk factors as well (Haw, 2017).
Future Treatment
Diabetes has mainly been controlled by the administration of the insulin drug, however, this presents implications due to the constant need for injection and the possibility of developing insulin resistance. This is how researchers have come to develop ideas for future treatments such as utilizing vanadium salts (Shechter and Shisheva,1993).
It is evident that vanadium salts seem like a viable option as they are able to replicate the effects of insulin on important target tissues in vitro (Brichard and Henquin, 1995). Additionally, they are able to successfully decrease blood glucose levels within insulin-deficient diabetic rats and help glucose homeostasis in diabetic rodents that have insulin-resistance and obesity (Brichard and Henquin, 1995).
Final Remarks
Type 1 and Type 2 diabetes are both prevalent global diseases with long term consequences. Although there is still much that is not understood, researchers have come a long way and are advancing at a remarkable rate. The rate that the disease has been diagnosed should alarm all health organizations and encourage everyone to implement more preventative programs encouraging active, healthy lifestyles. This is especially true for North America, with the current culture of fast food and sedentary lifestyle. However, current research will continue to find ways to make the disease more manageable for day-to-day living.
References
American Diabetes Association. (2017). Diabetes Symptoms. Retrieved from: http://www.diabetes.org/diabetes-basics/symptoms/
Are You at Risk?. (2018). Canadian Diabetes Association. Retrieved from: www.diabetes.ca/about-diabetes/risk-factors/are-you-at-risk.
Baynest W. (2015). Classification, Pathophysiology, Diagnosis and Management of Diabetes Mellitus. Journal of Diabetes & Metabolism, 06(05). doi:10.4172/2155-6156.1000541
Centers for Disease Control and Prevention. (2017). National diabetes statistics report. Atlanta, GA: Centers for Disease Control and Prevention.
Classification and Diagnosis of Diabetes. (2014). Diabetes Care, 38(Supplement_1), S8-S16. doi: 10.2337/dc15-s005
Dean L., McEntyre J. (2004). The Genetic Landscape of Diabetes. Retrieved April 5, 2011 from NCBI.
Diagnosis and Classification of Diabetes Mellitus. (2009). Diabetes Care, 33(Supplement_1), S62-S69. doi: 10.2337/dc10-s062
Eckel RH. Metabolic syndrome. In: Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL, Loscalzo J, eds. Harrisons Principles of Internal Medicine. 17th ed. New York, New York. McGraw-Hill;2008:1509-1514.
Ega, M., & Dinneen F. (2014). What is diabetes?. Medicine, 42(12), 679-681.
Forouhi N., & Wareham N. (2014). Epidemiology of diabetes. Medicine, 42(12), 698-702. doi: 10.1016/j.mpmed.2014.09.007
Haw S., Galaviz I., Straus N., Kowalski J., Magee J., Weber B., Wei J., Narayan M., Ali K. (2017). Long-term Sustainability of Diabetes Prevention Approaches: A Systematic Review and Meta-analysis of Randomized Clinical Trials. JAMA Internal Medicine. 177 (12): 1808–1817
McCarthy MI. (2010). Genomics, type 2 diabetes, and obesity. New England Journal of Medicine, 363(24), 2339-2350.
MNT Editorial, T. (2016, January 05). Diabetes Symptoms: Common Symptoms of Diabetes. Retrieved September 25, 2018, from https://www.medicalnewstoday.com/info/diabetes/diabetessymptoms.php
Mottalib A., Kasetty M., Mar Y., Elseaidy T., Ashrafzadeh S., Hamdy O. (2017). Weight Management in Patients with Type 1 Diabetes and Obesity. Current Diabetes Reports. 17 (10): 92. doi:10.1007/s11892-017-0918-8
National Institute for Health and Clinical Excellence. (2008). Clinical guideline 66: Type 2 diabetes. London.
Pathophysiology Research. (2017). Retrieved September 25, 2018, from https://www.diabetes.ca/research/research-funding/pathophysiology-research
Ramachandran, A. (2014). Know the signs and symptoms of diabetes. The Indian Journal of Medical Research, 140(5), 579–581.
Shechter, Y., & Shisheva, A. (1993). Vanadium salts and the future treatment of diabetes. Endeavour, 17(1), 27-31.
Siddiqui A., Siddiqui S., Ahmad S., Siddiqui S., Ahsan I., Sahu K. (2004). Diabetes: Mechanism, Pathophysiology and Management. International Journal of Drug Development and Research, 21-43. doi:10.1016/b978-012732350-3/50003-x
Siddiqui A., Siddiqui S., Ahmad S., Siddiqui S., Ahsan I., Sahu k. (2013). Diabetes: Mechanism, Pathophysiology and Management-A Review. Int. J. Drug Dev. & Res., 5(2): 1-23.
Symptoms & Causes of Diabetes. (2016). Retrieved from: https://www.niddk.nih.gov/healthinformation/diabetes/overview/symptoms-causes
TEDDY Study Group. (2008). The environmental determinants of diabetes in the young (TEDDY) study. Annals of the New York Academy of Science, 1150, 1-13.
The top 10 causes of death Fact sheet N°310. World Health Organization. May 24, 2018.
World Health Organization. Global report on diabetes. World Health Organization, 2016.
Yeung C., Rawlinson D., Craid E. (2011). Enterovirus infection and type 1 diabetes mellitus: systematic review and meta-analysis of observational studies. BMJ, 3, 342, d35.