This is an old revision of the document!
Table of Contents
Introduction
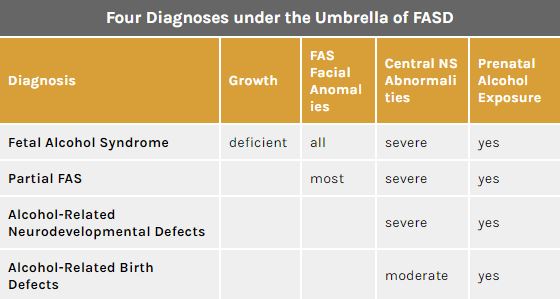
Figure 1: Diagnosis and characteristics under the FASD Umbrella </style>
<style justify> The detrimental effects of drinking during pregnancy have been commonly known for many centuries. However, It wasn’t officially documented until the late 1900s when medical practitioners decided it was necessary to establish formal term to describe these effects.[1] Researchers have since arrived at adopting an overarching term, called Fetal Alcohol Spectrum Disorder (FASD), thereby encompasses all the levels of prenatal alcohol exposure.
Fetal Alcohol Spectrum Disorder (FASD) is an umbrella term that describes the range of effects that can occur in an individual whose mother drank alcohol during pregnancy.[2] Such effects could be physical, mental, and/or behavioral. There are four main characteristics of those affected by FASD. They are: growth deficiencies, facial anomalies, central nervous system abnormalities and prenatal alcohol exposure. Notably, the disabilities caused with FASD are irreversible and have lifelong implications to individuals who are affected.[3]
Although FASD is not a diagnosis in itself, four diagnoses fall under its spectrum that increase in seriousness depending on the severity of FASD characteristics (Figure 1)[1]:
- Fetal Alcohol Syndrome (FAS)
- Partial FAS (pFAS)
- Alcohol Related Neurodevelopmental Disorder (ARND)
- Alcohol Related Birth Defects (ARBD)
</style>
Epidemiology
<style justify> Epidemiological studies are central to understanding how health-related conditions, such as fetal alcohol spectrum disorder (FASD), are distributed in human populations and to identifying factors that influence the occurrence of those distributions.
Meta-regressions have estimated that 2.3% of babies are born with FASD globally.[4] However, these rates vary considerably between countries and even within different regions of a nation. It is observed that populations situated within poorer and undeveloped areas experience higher prevalence of FASD. For example, several villages within South Africa can experience rates as high as 32% [5]. In contrast, more wealthy cities in a developed nation like Australia can have prevalence rates as low as 0.1%.[6] Reasons for the discrepancy in rates can lie in systemic problems involving alcohol abuse and poor education.
Canada specifically has over 3,000 babies being born with FASD every year. Furthermore, 300,000 individuals are currently living with a diagnosis under the FASD umbrella. Although the general prevalence rate lies between 1-2%, Aboriginal communities in Canada experience higher incidence of FASD. Studies done in Aboriginal communities in British Columbia found rates as high as 16%.[7]
</style>
Pathophysiology
<style justify> FASD is really hard to detect. The most optimal way is for self-disclosure, otherwise there are tests physicians may carry out in order to determine whether the woman is at risk of drinking.[8] </style>
Signs
<style justify> So the first sign you can see is how much is the intake of alcohol. The average consumption of alcohol for non-pregnant women is defined into three categories – light drinking (1.2 drinks per day), moderate drinking (2.2 drinks per day), and finally heavy drinking (3.5 drinks per day or more).[8] However, the amount of alcohol needed to be consumed to cause potential damage to the offspring is just one drink per day.[8][9] Recent studies have shown that even one drink per day is detrimental to the babies’ health and as such have concluded that establishing a threshold cannot be adequately identified.[8]
As mentioned above the signs for FASD are extremely hard to see. No biological marker is accurate enough to identify FASD. Studies have shown some signs of analysis of meconium and hair samples for fatty acid ethyl esters, but a larger sample size would be needed.[8] Another research that is being seen is γ-glutamyl transferase, hemoglobin-associated acetaldehyde, and carbohydrate-deficit transferrin.[8] Again, the issue lies that this research cannot be proven working to identify drinking in pregnant women.[9] </style>
<style center>
</style>
<style justify> The easiest sign is from the patient themselves. Self-reporting of maternal alcohol is essential to protect the lives of the baby and mother.[8] However, the stigmatization of drinking causes fewer people to discuss with this with their doctor. One thing doctors use as a consensus is the history of the patient. This leads to doctors assuming individuals who did not drink before pregnancy or a minimum amount would stop.[8] As studies showed, this was highly inaccurate as twice as many people admitted to alcohol consumption rather than when compared to medical records.
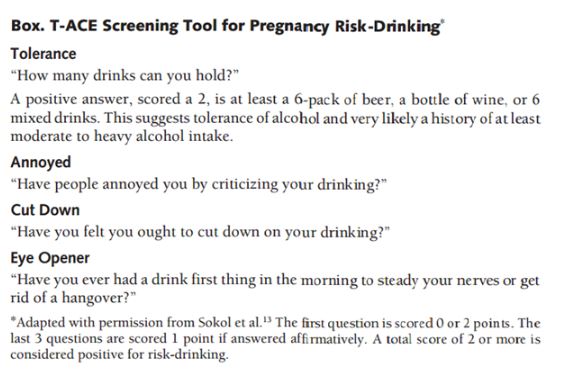
This is not to say that doctors do not have tools to figuring out women who intake alcohol during pregnancy. For example, one tool is called the T-ACE, and it is a traditional screening test by asking four questions.[8] The results from the analysis typically identify 90% of patients who can be potential risk-drinkers, but false-positives can also be ruled out by asking follow-up questions. Other tests are Tolerance, Worry, Eye-opener, Amnesia, Cut-down (TWEAK), Alcohol Use Disorders Identification Test (AUDIT), and Short Michigan Alcoholism Screen Test (SMAST) are a few tests used to identify potential risk-drinkers.[8] </style>
Symptoms
<style justify> The symptoms of individuals who have FAS have often had characteristics of facial dysmorphology, which is midfacial hypoplasia, long smooth philtrum, thin upper lip, small eyes that seem wider apart. Another symptom deals with growth restriction which affects the central nervous system and causes neurodevelopmental abnormalities, like ophthalmic involvement. Habituation to stimuli was most noticeable for neonatally, and much worse symptoms developed at eight months by using two indexes – Bayley Mental Developmental Index, and Psychomotor Developmental Index. Both of these indexes check to see how infant behavioral functioning based on a scale. Additionally, infants were reported to have much slower reaction time when the mother was drinking between low to moderate. Symptoms in Preschool children are much more noticeable, with reaction time towards a task taking much longer, struggling to maintain attention, and hyperactivity. Aside from these effects, learning disabilities, memory deficits, psychiatric problems like mood disorders have been seen in school-aged children who were exposed to moderate drinking levels.
Find the symptoms is not an easy thing to do. Many doctors have failed in identifying children with FAS, with one study going as far as out of 19 infants, only one was identified as a possible effect of FAS.[8] However there were seven who displayed it. About half of family physicians themselves have little confidence in diagnosing for FAS.[8] </style>