This is an old revision of the document!
Table of Contents
Epilepsy: Childhood Absence Epilepsy
Introduction
Figure 1: Epileptic seizures involve disruption in brain cell activity.
Image from: http://www.webmd.com/epilepsy/types-of-seizures-their-symptoms </style>
<style justify> Epilepsy is the fourth most common neurological disorder in people of all ages, and affects the central nervous system. This disorder is chronic, and entails recurrent, unprovoked seizures lacking visible cause (Mayo Clinic, 2013). These seizures are the most characteristic symptom of this disorder, and are due mainly to the disruption of nerve cell activity, ranging from mild to severe (Mayo Clinic, 2013). Epilepsy may also constitute a range of other health problems, and can affect the safety, social relationships, and treatment of afflicted individuals (Epilepsy Foundation, 2014). Diagnoses of epilepsy are based on medical and family history, descriptions of episodic seizures, as well as various diagnostic tests, such as electorencephalograms (EEGs). Epileptic seizures are readily controllable with medications, or various other treatment options (Epilepsy Ontario, 2016).
Childhood Absence Epilepsy (CAE), or petit mal epilepsy, typically occurs in otherwise normal, school-aged children, with peak onset occurring at 6-7 years old. It is observed more frequently in young girls. This disorder is characterized by frequent, daily absence seizures (Loiseau et al., 2002). Absences differ from regular epileptic seizures in that they are non-convulsive and typically accompanied by a brief loss of consciousness. Absence seizures can occur in epileptic children up to 200 times a day (Crunelli and Leresche, 2002). They are unassociated with visual and sensory stimuli, and are generally deemed as unprovoked. CAE typically tends to recede in adolescence for most affected individuals (Crunelli and Leresche, 2002). </style>
<br>
Epidemiology
Approximately 1 in 100 Canadians currently live with epilepsy (Epilepsy Ontario, 2016). The yearly incidence of epilepsy is deemed to be approximately 50 cases per 100 000 individuals in developed and industrialized countries. In areas of socioeconomic deprivation, these risks tend to be higher. Generally, in these regions, the yearly incidence tends to hover around 150 cases per 100 000 individuals (Sander, 2003). Resource-poor countries are believed to demonstrate higher incidences of the disorder due, in part, to the lack of medical facilities and improper diagnoses. However, despite these factors, it is widely believed that rates in developing countries are genuinely higher (Sander, 2003).
Globally, 50 million people are currently afflicted by epilepsy. Active epilepsy — constituting recurrent seizures and use of medication — is estimated at 4-10 individuals per 1000 in higher income countries, while the rate proves higher in low income areas, at about 7-14 per 1000 (World Health Organization, 2012). Endemic conditions such as malaria, injury, and medical infrastructure are believed to contribute to these rates of disease (World Health Organization, 2012).
New diagnoses of epilepsy are approximated at 2.4 million annually (World Health Organization, 2012).
In the case of Childhood Absence Epilepsy, the annual incidence has been reported to fall within the range of 2-8% per 100,000 children under the age of 16 years old. Among children that are already afflicted with epilepsy, rates can go up 10% (Crunelli and Leresche, 2002). Furthermore, girls are deemed to be at twice the risk of boys in developing Childhood Absence Epilepsy, however, equal incidences have thus far been reported (Crunelli and Leresche, 2002).
<br>
Signs and Symptoms
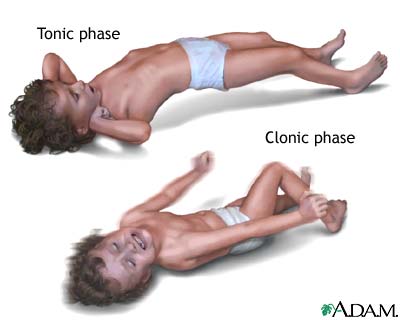
Figure 2: A depiction of tonic and clonic seizure types in children.
Image from: https://therefusers.com/cdc-says-seizures-can-occur-after-vaccination/ </style>
The symptoms of epilepsy are a result of experiencing seizures, which is the defining feature of this neurological disorder. A seizure occurs when there is an excessive synchrony of activity between neurons within the brain (McCormick & Contreras, 2001).
Seizures can be classified broadly as either partial or generalized (McCormick & Contreras, 2001). Partial seizures occur when the onset of abnormal activity is in one cortical region of the brain; typically within one cerebral hemisphere (McCormick & Contreras, 2001). Generalized seizures occur when the onset of abnormal activity is in both cerebral hemispheres (McCormick & Contreras, 2001). There are different subcategories of partial and generalized seizures and each with their own set of symptoms.
Partial seizures can either be simple or complex in which the later involves a loss in consciousness or cognitive abilities and the former does not (McCormick & Contreras, 2001). Simple partial seizures may also involve an “aura” which is a sensory experience prior to the onset of the seizure (McCandless, 2011). These sensory experiences could involve: perceived buzzing or whistling noises, a bad taste in the mouth, visions of flashing lights, hallucinations, sweating, or nausea, etc., depending on the brain region involved (McCandless, 2011). Clonic movements (constant contraction and relaxation of muscles) of the neck, face or whole extremities may also appear as a symptom in simple partial seizures (McCandless, 2011). Complex partial seizures may involve the experience of an aura prior to the onset of the seizure, motionless staring involving a loss of consciousness or repetitive movements of the extremities (McCandless, 2011).
Generalized seizures are further divided into 6 subcategories each with differing symptomatology. They are: Clonic seizures, tonic seizures, absence seizures, atonic seizures, myoclonic seizures and tonic-clonic seizures (Mayo Clinic, 2017).
Clonic seizures: involve repetitive jerking movements usually of the face, neck and extremities associated with alternating muscle contraction and relaxation.
Tonic seizures: involves the stiffening of the muscles usually in the back, legs or arms, lasting for less than 20 seconds.
Absence seizures: involve a brief loss of consciousness leading to motionless staring. Simple absence seizures last for less than 10 seconds while complex absence seizures last up to 20 seconds and are accompanied by unintentional bodily movements.
Atonic seizures: involve a loss of muscle control for less than 15 seconds, which could lead to the individual collapsing to the ground.
Myoclonic seizures: involves very brief twitching or jerking of the neck, shoulders, arms or legs. It will seem as though the individual is being electrically shocked. These seizures will last no longer than a couple seconds.
Tonic-clonic seizures: this type of generalized seizures has two phases associated with it. First is the tonic phase in which the individual’s muscles will tighten and then they will lose consciousness. Second is the clonic phase where the individual’s muscles will contract and relax in a rhythmic fashion. These seizures typically last for 1 to 3 minutes, however if prolonged to over 5 minutes this becomes a medical emergency. (Mayo Clinic, 2017; Devinsky & Sirvin, 2013)
The symptoms reported for childhood absence epilepsy in particular are a result of the absence seizures experienced. The seizures present as staring spells lasting approximately 10 to 20 seconds as a result of a brief lack of consciousness (Holmes and Fisher, 2013). The child will not know that they have experienced the seizure and will continue with the activity they were previously involved in or they may experience some brief confusion (Donner, 2010). These seizures could occur up to one hundred times daily and are typically spurred on by exercise (Holmes and Fisher, 2013). A child may also experience automatisms, which are actions performed by the body unintentionally (Donner, 2010). These actions may include, tongue movement, chewing, swallowing, raising eyelids and fiddling with hands (Donner, 2010).
<br>
Diagnosis
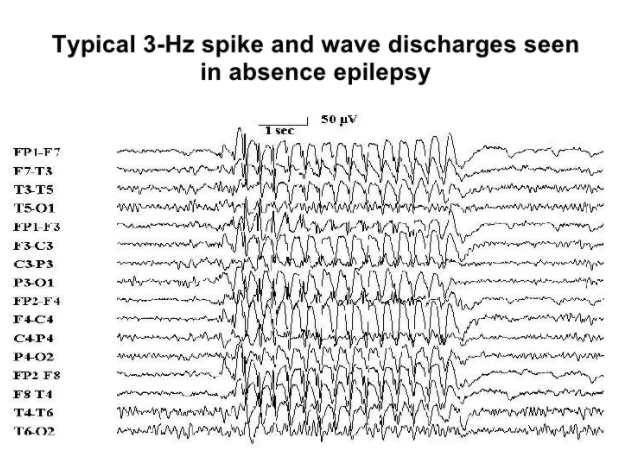
Figure 3: Typical EEG spikes in CAE.
Image from: http://www.slideshare.net/Kouya71/epilepsy-4502939 </style>
Doctors will take a number of steps to come to the proper diagnosis of epilepsy. Diagnostic procedures include:
Electroencephalogram (EEG): the EEG is the most common tool used in the diagnosis of epilepsy. The detection of an interictal spike by the EEG will assist in the confirmation of epilepsy as a diagnosis (Mayo Clinic, 2017). This interictal spike is caused by abnormal hypersynchrony among neurons in the brain (Pillai & Sperling, 2006). The EEG is also useful in determining whether the seizure is of partial or generalized origin (Pillai & Sperling, 2006).
Computerized Tomography (CT): the cross-sectional images of the brain taken by the CT scan can be used to investigate if there is any anatomical damage or abnormalities within the brain leading to the onset of the seizures (Mayo Clinic, 2017). Physicians will be able to detect if there are any tumors or cysts within the brain that may be associated with the seizures (Mayo Clinic, 2017).
Magnetic Resonance Imaging (MRI): MRI can provide more detailed images of the brain tissue with the use of strong magnets and radio waves (Mayo Clinic, 2017). Physicians can potentially detect lesions and abnormalities within the brain leading to the onset of the seizures (Mayo Clinic, 2017).
Positron Emission Tomography (PET): measures metabolic activity in the body with the use of a radioactive tracer that is injected into a vein (Mayo Clinic, 2017). PET can be used to detect the activity levels of brain regions that may be abnormal and leading to the seizures (Mayo Clinic, 2017).
Functional Magnetic Resonance Imaging (fMRI): technique that follows the path of oxygenated blood in the body to indicate where increased levels of activity reside (Mayo Clinic, 2017). Research is underway to combine fMRI with EEG in the diagnosis of epilepsy to get a more precise understanding of where abnormal activity is occurring in the brain during a seizure (Gotman, 2008).
History check: A physician will ask questions about the symptoms that have been occurring to raise the health concern. The physician will also ask about family history to identify whether there are any genetic underpinnings associated with the onset of the patient’s seizures (Mayo Clinic, 2017).
Examinations (Neurological & Neuropsychological): The physician can test motor, cognitive, memory, and speech functions to narrow down the type of seizures the patient may be experiencing (Mayo Clinic, 2017).
Laboratory tests: Physicians may request a blood sample from patients to look into whether they may have a genetic condition, toxin, or infection leading to the onset of the seizures (Mayo Clinic, 2017). The blood test can also help to determine if the seizures are merely a byproduct of another disease, such as diabetes.
To diagnose childhood absence epilepsy, physicians will start off with asking the caregiver about the history of the symptoms being presented and any other associated health problems (Holmes & Fisher, 2013). They will then proceed in a physical examination to see if there is any bodily damage that could be leading to the seizures (Holmes & Fisher, 2013). An electroencephalogram (EEG) on the child’s brain activity is essential in detecting the presence of seizures. The child will be diagnosed with childhood absence epilepsy if there is generalized neuronal activity at 3 Hz spike and wave discharges as indicated by the EEG (Holmes & Fisher, 2013). This 3 Hz spike is caused by a depolarization via excessive excitatory neuronal activity among pyramidal cells in cortical structures (McCormick & Contreras, 2001). In order to study the child’s seizure episodes with the EEG or to merely observe their symptoms, the child will be asked to intentionally hyperventilate (Holmes & Fisher, 2013). Hyperventilation has been shown to induce an absence seizure in most children diagnosed with CAE (Holmes & Fisher, 2013). CT and MRI scans appear to be normal in these patients, indicating that there doesn’t appear to be anatomical damage or abnormalities in the brains of these children (Holmes & Fisher, 2013).
<br>
Etiology
ENTER HERE YUMNA
<br>
Pathophysiology
ENTER HERE YUMNA
<br>
Prognosis and Prevention
ENTER HERE KRITIKA
<br>
Treatment
Antiepileptic Drug (AED) monotherapy is the mainstay treatment measure for patients diagnosed with recurrent, unprovoked seizures or epilepsy. With the various types of seizures and epilepsy syndromes, a broad-spectrum of AEDs are available that are selective in targeting certain types of seizures/epilepsy syndromes then others (Ha & Bellanger, 2013). While AEDs do not cure epilepsy, instead are taken to prevent the onset of a seizure by altering and reducing the excessive electrical activity (or excitability) of the neurons that normally cause a seizure (Goldenberg, 2010). Different AEDs work in different ways and have different effects on the brain. AEDs are taken prophylactically either once or twice a day (Ha & Bellanger, 2013).
Childhood Absence Epilepsy and AEDs:
The three medications of choice commonly used as initial monotherapy to treat childhood absence epilepsy are Ethosuximide (Zarontin), Valporic acid (Epilim), and Lamotrigine (Lamictal).
Ethosuximide selectively blocks a type of calcium channel called the T-type calcium currents in the thalamic neurons, which inhibits the thalamocortical circuits responsible for generating the EEG spike-wave complex underlying and directly reducing absence seizures (Peterson & Albertson, 1998). Ethosuximide is given orally to patients as an initial dose of 250 mg capsule per day for 3-6 year olds and two 500mg capsules per day for children above 6 years of age (Goldenberg, 2010). Common side effects include anorexia and drowsiness and in extreme and less common cases liver toxicity and drug rash (Goldenberg, 2010).
Valproic acid decreases the breakdown of GABA, resulting in an increased inhibitory effect. Valproic acid is available in liquid or capsule form with a starting dose of 15 mg/kg/day or maintenance dose of 60mg/kg/day. Common side effects include abdominal discomfort, nausea, and weight gain (Goldenberg, 2010).
Lamotrigine works by blocking the sodium channels and is available in chewable and pill form. It is usually started at 0.5mg/kg/day and can be increased to a maximum of 5 to 10 mg/kg/d (Goldenberg, 2010).
The most efficacious and tolerable treatment has not been defined with very little guidelines for physicians to utilize when prescribing one AED over the other as each of these medications have different side effects and drug interaction profiles (Buchhalter, 2011).
However, as of a double blind, randomized control trial conducted in 2013, Ethosuximide is now the recommended first-line therapy in children with childhood absence epilepsy (Glauser et al., 2013). The study looked at the efficacy, tolerability and neuropsychological effects of ethosuximide, valproic acid, and lamotrigine in children diagnosed with CAE. 435 children were eligible and randomly assigned to one of three groups; drug doses were titrated for clinical response (until the child was free of seizures). The primary outcome was freedom from treatment failure (a defined criterion) after 16 weeks of therapy; the secondary outcome was attentional dysfunction.
The researchers found that Ethosuximide and Valproic acid are more effective than Lamotrigine in the treatment of childhood absence epilepsy. Ethosuximide was also associated with fewer adverse attentional effects (in 33%) where as attentional dysfunction was more common with valproic acid (in 49% children). This study address the ambiguity clinicians experienced when treating patients and is the first of its kind providing an evidence-based standpoint to initiate Ethosuximide as a first line drug choice. Valproic acid and lamotrigine are options when seizures are refractory to Ethosuximide (Glauser et al., 2013).
For patients who refuse pharmacological treatment, a Ketogenic diet, special high fat, low-carbohydrate diet, is available as an alternative regimen to control and manage seizures. (KRITIKA ADD STUFF HERE)
<br>
References
Buchhalter, J. (2011). Treatment of Childhood Absence Epilepsy—An Evidence-Based Answer at Last!. Epilepsy Currents, 11(1), 12-15.
Crunelli, V., & Leresche, N. (2002). Childhood absence epilepsy: genes, channels, neurons andnetworks. Nature Reviews Neuroscience, 3(5), 371-382.
Devinsky, O., & Sirven, J. I. (2013). Myoclonic Seizures and Tonic-Clonic Seizures. Epilepsy Foundation. Retrieved January 24, 2017, from http://www.epilepsy.com/learn/types-seizures/myoclonic-seizures
Donner, E. J. (2010). Absence Seizures. about kid’s health. Retrieved January 24, 2017 from, http://www.aboutkidshealth.ca/En/ResourceCentres/Epilepsy/UnderstandingEpilepsyDia gnosis/TypesofSeizures/Pages/Absence-Seizures.aspx
Epilepsy. (2013, May 31). Mayo Clinic. Retrieved January 21, 2017, from http://www.mayoclinic.org/diseases-conditions/epilepsy/basics/definition/CON-20033721?p=1
“Epilepsy”. Fact Sheets. World Health Organization. October 2012. Retrieved January 21, 2017.
Glauser, T. A., Cnaan, A., Shinnar, S., Hirtz, D. G., Dlugos, D., Masur, D., … & Adamson, P. C. (2013). Ethosuximide, valproic acid, and lamotrigine in childhood absence epilepsy: initial monotherapy outcomes at 12 months. Epilepsia, 54(1), 141-155.
Goldenberg, M. M. (2010). Overview of drugs used for epilepsy and seizures: etiology, diagnosis, and treatment. Pharmacy and Therapeutics, 35(7), 392.
Gotman, J. (2008). Epileptic Networks studied with EEG-fMRI. Epilepsia. 49 (s3), 42-51.
Ha, H., & Bellanger, R. (2013). Epilepsy: treatment and management. US Pharm, 38(1), 35-39.
Holmes, G. L. & Fisher, R. S. (2013). Childhood Absence Epilepsy. Epilepsy Foundation. Retrieved January 24, 2017, from http://www.epilepsy.com/learn/types-epilepsy-syndromes/childhood-absence-epilepsy
Loiseau, P., Panayiotopoulos, C. P., & Hirsch, E. (2002). Childhood absence epilepsy and related syndromes. Epileptic syndromes in infancy, childhood and adolescence, 3, 285-304.
McCandless, D. W. (2011). Epilepsy. Simple Partial Seizures (143-152) Chicago. IL: Springer Science+Business Media.
McCormick, D. A., & Contreras D. (2001). On the Cellular and Network Bases of Epileptic Seizures. Annul. Rev. Physiol, 63: 815-846.
Peterson, S. L., & Albertson, T. E. (Eds.). (1998). Neuropharmacology methods in epilepsy research. CRC Press.
Pillai, J. & Sperling, M. R. (2006). Interictal EEG and the Diagnosis of Epilepsy. Epilepsia. 47 (s1), 14-22.
Sander, J. W. (2003). The epidemiology of epilepsy revisited. Current opinion in neurology, 16(2), 165-170.
What Is Epilepsy? (2014, January). Epilepsy Foundation. Retrieved January 21, 2017, http://www.epilepsy.com/learn/epilepsy-101/what-epilepsy
What is Epilepsy? (2016). Epilepsy Ontario. Retrieved January 21, 2017, from http://epilepsyontario.org/about-epilepsy/what-is-epilepsy/
<br>