Table of Contents
Lupus
Introduction
What is lupus?
Lupus is the common name for the disease known as lupus erythematosus. The disease is characterized by the body’s immune system attacking healthy tissues within the patient. The disease is an autoimmune chronic disease and can be fatal. Often appears as a rash with similar characteristics to a skin disease, but can develop to other organ systems of the body as well. Essentially the immune system produces antibodies in abundance which attack the body’s tissues causing inflammations, possible organ failures, etc. (Askanase et al., 2012). It is interesting to note that the name lupus is believed to be derived from the rash people developed as a result of the disease and how it looks similar to a bite from a wolf. The first case was reported in 1874 and it is a fairly old disease (Adelman et al., 1986). Usually it is not life-threatening, but it is positively correlated with a shorter lifespan and in certain severe cases directly leads to death.
Types of lupus
There are many different types of lupus that occur in clinical cases. Each of these types has different treatment methods and pathophysiology for how they work. It depends on how the immune system attacks the tissues in the body and which tissues they attack. Three subtypes of lupus that are common in clinical settings include:
- Acute cutaneous lupus erythematosus (ACLE)
- Local rash
- Less severe
- Systemic cutaneous lupus erythematosus (SCLE)
- Affects multiple body systems simultaneously
- Often affected by sun exposure to head, shoulders, neck, etc.
- Chronic Cutaneous lupus erythematosus (CCLE)
- This covers other less common forms like lupus timidus, lupus profundus and chilblain lupus
- Depends on types of sensitivity to the sun
- How lesions are formed etc. (Walling, 2009)
Risk factors (hormones, genes, environment)
Female sex hormones are linked with a higher prevalence of the disease. In dizogyotic twins (separate zygotes) there is 1-5% chance of the disease being passed on. In monozygotic twins it was found that there was a 29-57% chance of the disease being present meaning there is a genetic component. There are no specific genes that code for this disease. However, there is a correlation in monozygotic twins having similar genetics which cause the disease to become prevalent. Therefore, there may be a genetic link for the disease, but having the gene does not necessarily mean that people will develop the disease. The environment is also believed to be important for the development of the disease where some monozygotic twins did not develop the disease (Askanase et al., 2012). There are epigenetic factors believed to be triggered based on the environment of the patient that may or may not lead to the disease.
Epidemiology
Women are more likely to be affected (9 times more likely than men). After puberty and before menopause women have the highest rate of getting the disease (15:1 compared to men) (Askanase et al., 2012). Non-Caucasians are more likely to have the disease than Caucasians (Lau et al., 2006). In a paper by Lau et al (2006), they looked at prevalence records of lupus around the world and compared them to different ethnic groups. They found that Indians, Afro-Americans, Chinese and Japanese had higher rates of prevalence than Caucasians from North America or England. There were also reported differences in the instances of the disease between the different ethnicities. They also noted that these groups may have less socio economic advantages for dealing with the disease making their rates inflated compared to Caucasians.
Pathogenesis
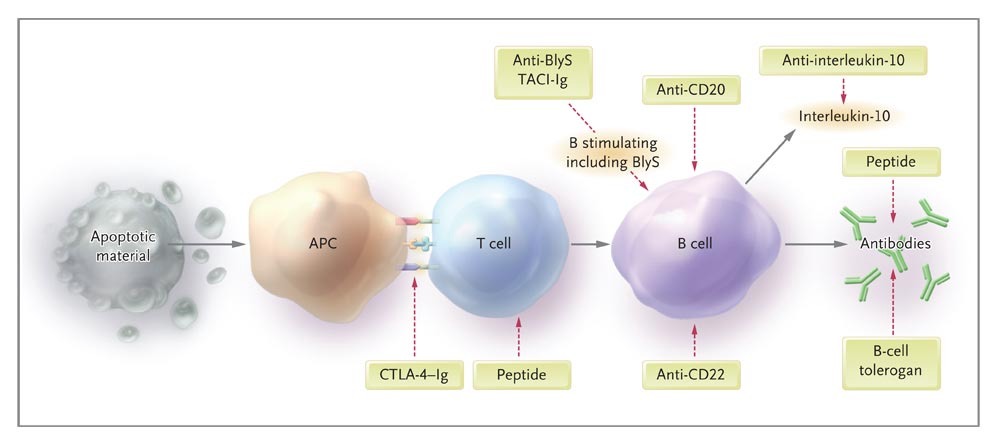
Lupus is an chronic autoimmune disease in which the body produces its own antibodies targeted at itself (Rahman & Isenberg, 2008; Elkon & Casali, 2008; Fortuna & Brennan, 2013). These antibodies are known as autoantibodies. Environmental factors like UV light and drug stimulation can cause abnormalities in apoptosis, a common manifestation of Lupus. Destruction of the cell leads to components of the nucleus being released which serve as the antigens stimulating the innate and adaptive immune response (Rahman & Isenberg, 2008; Elkon & Casali, 2008; Fortuna & Brennan, 2013).
In patients with Lupus the main cells affected within the innate immunity are Dendritic Cells (DC) and Neutrophils (Rahman & Isenberg, 2008). DCs serve to process antigens (foreign particles) and present them to T-cells. In Lupus patients DCs have been linked to an increase in the humoral response and expansion of autoreactive T-cells and B-cells (Rahman & Isenberg, 2008; Fortuna & Brennan, 2013). Neutrophils are granulocytes which aid in killing microbes by NETs (Neutrophil Extracellular Trap). This is a process in which DNA is released into the extracellular fluid and forms web structures that attach to pathogens preventing their mobility and spread. In Lupus these NETs undergo NETosis (apoptosis of the NETs) which results in a large accumulation of DNA which serves as autoantigens for DCs (Fortuna & Brennan, 2013).
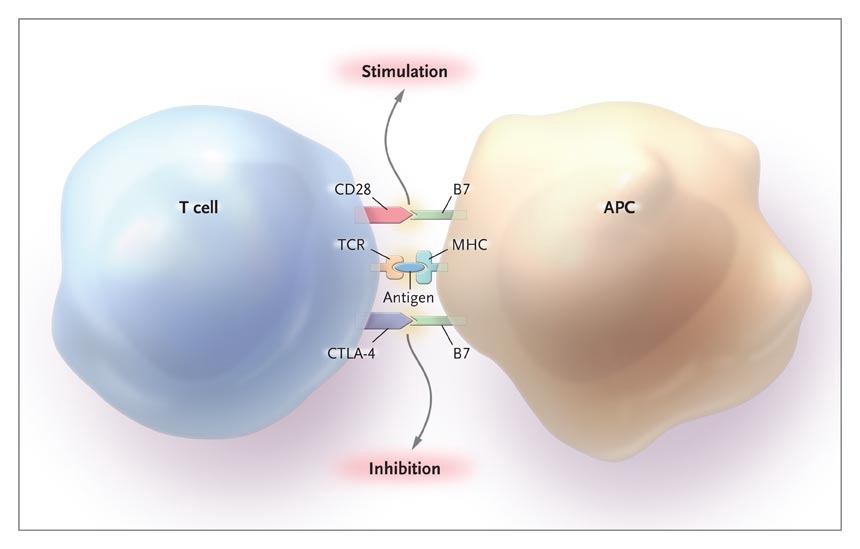
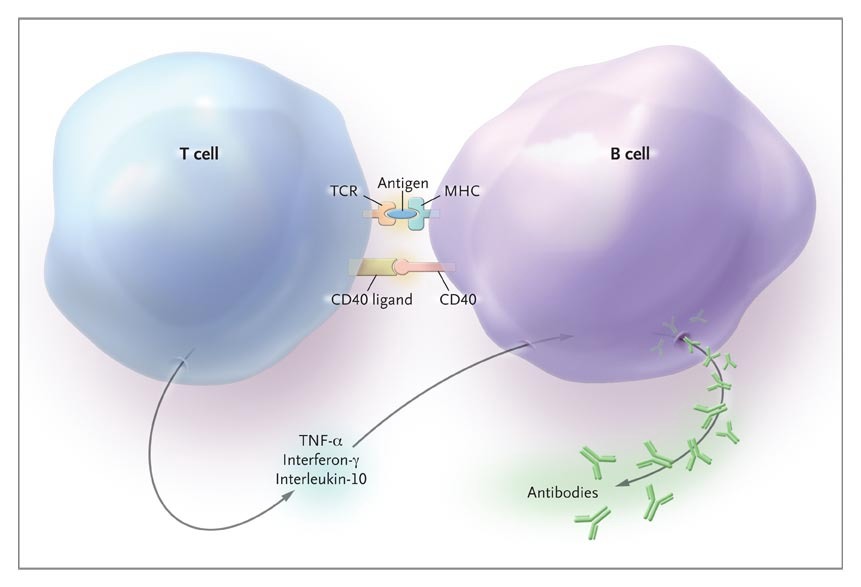 T-cell receptors (TCR) are located on the surface of T-cells. These receptors interact with the antigen that is presented by the APC (antigen presenting cell) or DC. The APC and T-cell form a complex with the TCR, and MHC and antigen (Rahman & Isenberg, 2008). However binding of the antigen-MHC complex does not result in a reaction. Instead binding of costimulatory ligands facilitate stimulation or inhibition. Stimulation results in recruitment of B-cells which form a new complex with the T-cell and antigen (Rahman & Isenberg, 2008). The cells stimulate the other in that binding of the B-cell CD40 to the CD40 ligand on the T-cell results in a release of cytokines from the T-cell. The cytokines stimulate B cell division, shift the antibody production from IgM to IgG, and allow for molecular changes in the antibody produced to increase affinity for the antigen (Rahman & Isenberg, 2008). The effect of the T-cell on the B-cell is based on its affinity to the antigen. Higher affinity of the T-cell to the antigen results in a greater response by the B cell.
T-cell receptors (TCR) are located on the surface of T-cells. These receptors interact with the antigen that is presented by the APC (antigen presenting cell) or DC. The APC and T-cell form a complex with the TCR, and MHC and antigen (Rahman & Isenberg, 2008). However binding of the antigen-MHC complex does not result in a reaction. Instead binding of costimulatory ligands facilitate stimulation or inhibition. Stimulation results in recruitment of B-cells which form a new complex with the T-cell and antigen (Rahman & Isenberg, 2008). The cells stimulate the other in that binding of the B-cell CD40 to the CD40 ligand on the T-cell results in a release of cytokines from the T-cell. The cytokines stimulate B cell division, shift the antibody production from IgM to IgG, and allow for molecular changes in the antibody produced to increase affinity for the antigen (Rahman & Isenberg, 2008). The effect of the T-cell on the B-cell is based on its affinity to the antigen. Higher affinity of the T-cell to the antigen results in a greater response by the B cell.
The antibodies that are produced by the B cell are known as autoantibodies because they bind to molecules that the body has in abundance such as DNA. The main antigen in Lupus patients is double stranded DNA (Rahman & Isenberg, 2008; Elkon & Casali, 2008; Fortuna & Brennan, 2013). Once the anti-DNA antibody binds to the antigen they form a antigen-antibody complex inducing inflammation at the tissue (Elkon & Casali, 2008; Rahman & Isenberg, 2008; Fortuna & Brennan, 2013). It has been proposed that this complex migrates to the renal glomerular basement membrane and activates complement and promotes inflammation in kidneys which is characteristic of Lupus (Rahman & Isenberg, 2008; Fortuna & Brennan, 2013). Another theory suggests antibodies cross react with proteins in kidney thereby having an effect. Studies demonstrated that anti-DNA antibodies cross reacted with alpha actin which is a protein critical to maintaining function of renal podocytes (cells of the filtration barrier) (Rahman & Isenberg, 2008; Fortuna & Brennan, 2013).
Signs & Symptoms
Considering that lupus is a very complex disease that has thousands of faces, it is hard to list and describe all of its symptoms because almost all of the body’s systems can be affected. Ultimately, symptoms of lupus drastically vary from person to person making each person’s symptom profile to be unique. Some individuals experience mild symptoms, compared to others who may be affected more severely. The explained symptoms may appear in the early stages of the disease, or may occur as the disease progresses. Specifically, it is rare to see sudden and severe symptoms during the onset of the disease. Rather, with the progression of the disease, new symptoms begin to appear over the course of weeks, months, and sometimes years. Considering that the symptoms have the tendency to appear and disappear, it is difficult and may take an individual time to realize that their health may be at risk (Mielczarek, 2017). When discussing symptoms, it is important to consider that there are two types of them. The first type of symptoms are ones that can happen in other diseases, and are therefore referred to as non-specific symptoms. Whereas as the second type of symptoms are lupus specific.
Non-specific symptoms include fatigue, weight changes, fever, and swollen glands. These symptoms are usually only associated to lupus after lupus-specific symptoms are observed. Firstly, fatigue is a common symptom among lupus patients. Specifically, the tiredness an individual experiences when suffering from lupus is much greater than the activities done (Mielczarek, 2017). Thus, it is important to differentiate normal tiredness from lupus tiredness. Next, lupus causes fluctuations in weight. There may be continuing weight loss that cannot be explained over either a small or large period of time. There can also be weight gain due to swelling of the body, especially in the feet and legs. Another non-specific symptom is the occurrence of a fever which happens with common conditions, like a cold or the flu. However, in lupus patients a fever is taken seriously because it may indicate the presence of an infection, or that lupus is becoming active in the body. This type of fever is noted to be either low-grade fevers that occur over a prolonged period of time, or very high fevers that happen suddenly. Lastly, the observation of many swollen glands may be an indicator of lupus especially if they are noticed along with lupus-specific symptoms (Mielczarek, 2017).
Symptoms specific to lupus occur due to the involvement of various organs of the body. The combinations of the organs being affected is immense, and explaining each possible combination and providing a complete list of lupus-specific symptoms is unfeasible. Thus, in order to help differentiate lupus from other conditions, the American Rheumatism Association has provided eleven abnormalities that lead to the suspicion of lupus. These abnormalities include: symptoms, signs, and tests, which will be discussed further in the diagnosis section (Mielczarek, 2017). Compared to symptoms, which are what an individual feels, signs are what can be observed by the physician. Important to note that only a couple of lupus patients actually develop all eleven abnormalities. Listed below are the 11 abnormalities:
- The butterfly rash: occurs over the cheeks and the bridge of the nose, may be faint or obvious.
- Photosensitivity: occurs in almost half the patients. Exposed skin experiences extreme sensitivity to sunlight causing rashes.
- Discoid lupus: scaly, raised on the arms, chest, scalp, ears, and even face.
- Mucosal ulcers: sores in the mouth and nose mucous linings.
- Arthritis: extremely common in lupus patients—unusual for patients to not have arthritis. Causes joint pain in the hands, wrists, knees, elbows, and other joints of the arm and legs. The pain does move from one joint to another, and is therefore referred to as migratory pain. When lupus is extremely active, there will be severe pain and swelling around said joints. Deformities from lupus arthritis may occur, but there will not be any major loss of function.
- Pleuritis and Pericarditis: Affects about half the lupus patient population. The inflammation of the lungs’ lining is referred to as pleuritis, whereas pericarditis is the inflammation of the heart’s lining. These two may occur either simultaneously or individually. Pleuritis, and sometimes pericarditis, results in an individual experiencing specific chest pains when air is breathed in. These signs can be observed by a physician through the use of a chest x-ray, heart ultrasound and electrocardiogram (ECG).
- Kidney involvement: can vary from moderate to extreme. Almost all patients with lupus are known to have some sort of kidney involvement. In about fifty percent of lupus patients, there is a concern of kidney failure resulting in the kidneys’ inability to provide clean blood for the body. Unfortunately, patient will not experience symptoms until the kidneys have already been damaged. The most common symptom of kidney damage is oedema, also known as fluid retention, which includes swelling and weight gain, specifically in the legs and feet. Detecting kidney involvement is crucial because most lupus-related deaths are because of severe kidney involvement.
- Seizures and Psychosis: occurs because of the central nervous system’s involvement with lupus. Occurs in about fifteen to twenty-five percent of patients. Seizures cause a person to lose control of voluntary movement and consciousness. An individual who experiences seizures as their first symptom is not suspected with lupus unless other lupus-related issues are observed.Psychosis is a mental disorder that involves the disruption of thoughts and behaviours, this results in hallucinations and delusions.
- Blood cell disorders: the red or white cells or platelets are attacked by autoantibodies.
- Immunologic disorders: with the presence of other symptoms, when four autoantibodies are found in the blood, it leads to the suspicion of lupus. Details and the detection of the four autoantibodies is discussed in the diagnosis section.
- Antinuclear antibodies: Almost all lupus patients are observed to have these in their blood. More on this is discussed in the diagnosis section.
Diagnosis requires the presence of four of the eleven criteria points mentioned above, the tests used for diagnosis will be discussed further in the diagnosis section (Mielczarek, 2017).
Some other common symptoms among lupus patients include: Continuous increase in hair loss
- Subacute cutaneous lupus erythematosus involves rashes occurring on the arms and upper body
- Raynaud’s phenomenon is when fingers and toes turn white as a result of of being exposed to cold temperatures. This happens because of blood flow reduction because of the blood vessels spazzing. Digits may then turn bluish or reddish.
- Vasculitis is a term that can be translated to the inflammation of blood vessels. This results in raised, itchy hives that pop up on any part of the body. These hives tend to appear and disappear within twenty four hours.
- Headaches are very common in lupus.
- Consistently high blood pressure occurs alongside severe kidney involvement. Having persistently high blood pressure can lead to blood vessel damage, which can result in strokes and heart failure (Mielczarek, 2017).
Diagnosis
It is hard to diagnose lupus due to its complex underlying mechanisms. Its signs and symptoms are wide-ranging and vary from person to person. The symptoms of lupus often resemble or overlap symptoms of other diseases. Currently, it is not possible to accurately diagnose lupus using just one test. The combination of blood tests, urine tests, tissue biopsies and/or imaging tests aid with the diagnosis of lupus.
Blood tests for lupus
The normal immune system makes antibodies to help fight off foreign invaders (John Hopkins Lupus Center, 2018). In contrast, some immune systems produce antibodies that attack the body’s own cells mistaking them as invaders, causing inflammation and damage various body parts (John Hopkins Lupus Center, 2018). This type of antibodies is known as auto-antibodies, and is present in autoimmune diseases such as lupus (John Hopkins Lupus Center, 2018). Currently, many blood tests can be performed to identify specific auto-antibodies to assist the diagnosis of lupus (John Hopkins Lupus Center, 2018). A blood test confirming the presence of an auto-antibody cannot be conclusive, but combining many tests along with certain physical findings verifies the diagnosis (John Hopkins Lupus Center, 2018). Anti-nuclear antibody (ANA) tests are usually the first test conducted to test for the possible diagnosis of lupus, and in people with a positive result, more tests are performed to check for other antibodies that can help confirm the diagnosis (John Hopkins Lupus Center, 2018). These tests include anti-phospholipid antibody (APL), anti-double-stranded DNA antibody (anti-dsDNA), anti-Smith (anti-Sm), anti-U1RNP, anti-Ro/SSA, and anti-La/SSB.
- Anti-nuclear antibodies (ANAs) test detects ANA in blood (Brazier, 2018). ANAs are a type of special antibodies that that attacks nuclei inside cells (Lupus Foundation of America, 2013). A positive test indicates the presence of anti-nuclear antibody (John Hopkins Lupus Center, 2018). However, it does not mean the presence of an autoimmune disease such as lupus (John Hopkins Lupus Center, 2018). Around 98 percent of people with lupus will have a positive result in the ANA test (John Hopkins Lupus Center, 2018). However, a positive test for ANA is also seen in people with other diseases and even in people without any autoimmune disorders (Brazier, 2018). Therefore, other tests must be performed to confirm the diagnosis.
- Anti-phospholipid antibodies (APLs) are a type of antibody that targets phospholipids (Brazier, 2018). Only about 50 percent of people with lupus test positive for APLs (Brazier, 2018). Just like ANA test, individuals without lupus can also be tested positive with APLs (Brazier, 2018). Moreover, a positive test indicates a higher risk of blood clots, stroke, and pulmonary hypertension. The presence of APLs indicates a higher risk of pregnancy complications, such as miscarriage or premature birth (Suryanarayan & Garcia, 2014).
- Anti-double-stranded DNA antibody (anti-dsDNA) is a specific type of ANA antibody that occurs in approximately 30 percent of people with lupus (John Hopkins Lupus Center, 2018). This test is useful in confirming a diagnosis of lupus since less than 1 percent of people without lupus have this antibody (John Hopkins Lupus Center, 2018). However, the absence of this antibody does not eliminate the possibility of lupus (John Hopkins Lupus Center, 2018). If the test is positive, it often indicates a more serious form of lupus, such as lupus nephritis (John Hopkins Lupus Center, 2018).
- Anti-Smith antibody is found almost exclusively in individuals affected with lupus (John Hopkins Lupus Center, 2018). Approximately 20 percent of people with lupus have an antibody to Smith, a ribonucleoprotein that is present in the nucleus of a cell. It is present in fewer than 1 percent of healthy people, and it is rare in people that have other disorders (John Hopkins Lupus Center, 2018). Thus, the presence of anti-sm antibodies along with a positive ANA test is likely to confirm the diagnosis of lupus (John Hopkins Lupus Center, 2018).
- Anti-U1RNP antibodies are frequently present with anti-Sm antibodies in people affected with Lupus (John Hopkins Lupus Center, 2018). A positive test for anti-U1RNP antibodies in people with lupus is about 25 percent, while fewer than 1 percent of healthy individuals have this antibody (John Hopkins Lupus Center, 2018). However, this anti-body is not as specific to lupus as anti-dsDNA and anti-sm antibody, it is often present in other diseases (John Hopkins Lupus Center, 2018).
- Anti-Ro/SSA and anti-La/SSB antibodies are primarily found in individuals with lupus as well as primary Sjögren's syndrome (John Hopkins Lupus Center, 2018). The advantage of this test is that it shows people with lupus who have tested negative for ANA (John Hopkins Lupus Center, 2018). However, they are present in about 15 percent of people without lupus, and in people with other disorders as well (John Hopkins Lupus Center, 2018). Moreover, a pregnant mother diagnosed with lupus that has anti-Ro and anti-La antibodies, increases the chance the baby will have neonatal lupus, a condition that can cause congenital heart block (John Hopkins Lupus Center, 2018).
- Anti-histone antibodies, histones are proteins that secure the structure of DNA (John Hopkins Lupus Center, 2018). Anti-histone antibodies are usually present in people with drug-induced lupus (DIL) (John Hopkins Lupus Center, 2018). However, they are not specific to systemic lupus, and need further tests to confirm (John Hopkins Lupus Center, 2018).
Other clinical tests for lupus
Serum (blood) complement test A serum complement test measures the levels of proteins that the body consumes when inflammation occurs (Brazier, 2018). Complement proteins are used up by the inflammation caused by lupus, which is why people with inflammation due to active lupus often have low complement levels (Brazier, 2018).
Urine tests Urine tests can help to diagnose and/or monitor the effects of lupus on the kidneys by examining the presence of protein, red blood cells and white blood cells (Brazier, 2018).
Erythrocyte sedimentation rate (ESR) This test measures the amount of inflammation in the body by measuring the rate at which red blood cells settle to the bottom of a test tube in one hour (John Hopkins Lupus Center, 2018). Erythrocyte sedimentation rate increases with more inflammation (John Hopkins Lupus Center, 2018). However, this test is not specific to lupus as elevated levels may also indicate other inflammatory condition (John Hopkins Lupus Center, 2018). This tool is often used by a doctor to monitor the progress of lupus (John Hopkins Lupus Center, 2018).
Treatments
Lupus is an autoimmune chronic disease that unfortunately does not carry with it a cure as of now. Even though there is not a straight out cure, there are treatments and medications that can greatly improve the quality of life of many lupus patients. Treatment for lupus really depends on the severity of your symptoms as medication can easy symptoms, reduce inflammation and prevent organ damage.
The first category of drugs involves the anti-inflammatory drug category. If you have lupus, there may be swelling the joints of the knees or wrists. Sometimes, patients have reported having a fever as well. Drugs in this category include NSAIDs such as ibuprofen and naproxen, which are over the counter medications that can combat these types of symptoms. However, overdosing on NSAIDs will increase your risk for stroke or heart attacks.
The second category for drugs involves the anti-malarial drug category. Since lupus has known symptoms such as rashes and mouth sores similar to Malaria, similar medications can be used to combat them. Furthermore, antimalarial drugs protect the skin from UV rays in the sunlight. However, these medications do increase the risk of clots. The third category for drugs involves the use use of corticosteroid, which are drugs that weaken parts of the immune system. These drugs would be prescribed if the doctor notices that lupus causes symptoms in your heart, lungs, kidneys or blood vessels. They can be taken as a pill or injected via an IV and are extremely quick at reducing swelling and joint inflammation. Corticosteroids, however, have some serious sides effects such as muscle weakness, diabetes and cataracts.
The fourth category for drugs involves Immunosuppressive Drugs which are similar to corticosteroids. These drugs also reduce the response your immune system sends out and controls symptoms/prevents organ damage in the long term. These drugs have known to reduce your body's innate ability to fight disease and might increase chances for cancer in the long run. Using them alongside corticosteroids is sometimes beneficial as lower doses of both of them can be used and as a result, the chances for higher side effects are reduced.
The fifth category for drugs involves Anticoagulants and Monoclonal Antibodies. Anticoagulants are a type of drug that assist in blood-thinning, which inherently reduces blood clots. Monoclonal antibodies are a new genre of drugs that are given via IV and target immune cells. They help reduce the need for steroid treatment, but these drugs have not been thoroughly tested in huge clinical populations.
For individuals that wish to stay away from pharmaceutical approaches, a few lifestyle changes can increase the quality of life for patients with lupus. By eating a balanced diet, getting plenty of sleep and exercise, you can seriously offset some of the chronic symptoms lupus causes.
Conclusion
In conclusion, Lupus is a chronic autoimmune disorder that causes diverse abnormalities in various areas and systems of the body. Considering that the signs and symptoms of this disorder vary from person to person, and are on and off, it is difficult to determine a diagnosis. Thus, there needs to be advancements in research for discovering methods for early Lupus diagnosis to meet its unique mechanism characteristics. Additionally, another area for future Lupus-related research is advancements in finding a cure for Lupus considering that there are only treatments for management currently available.
References
Askanase, A., Shum, K., & Mitnick, H. (2012). Systemic lupus erythematosus: an overview. Social work in health care, 51(7), 576-586.
Adelman, D. C., Saltiel, E., & Klinenberg, J. R. (1986, February). The neuropsychiatric manifestations of systemic lupus erythematosus: an overview. In Seminars in arthritis and rheumatism (Vol. 15, No. 3, pp. 185-199). WB Saunders.
Brazier, Y. (2018, November 12). What is lupus? Medical News Today. Retrieved from https://www.medicalnewstoday.com/articles/323653.php
Elkon, K., & Casali, P. (2008). Nature and functions of autoantibodies. Nature clinical practice. Rheumatology, 4(9), 491-8.
Fortuna, G., & Brennan, M. (2013). Systemic lupus erythematosus. Dental Clinics of North America, 57(4), 631-655. http://dx.doi.org/10.1016/j.cden.2013.06.003
John Hopkins Lupus Center. (2018). Lupus tests. Retrieved from https://www.hopkinslupus.org/lupus-tests/ Lau, C. S., Yin, G., & Mok, M. Y. (2006). Ethnic and geographical differences in systemic lupus erythematosus: an overview. Lupus, 15(11), 715-719.
Lupus Foundation of America. (2013). How lupus is diagnosed: an overview. Retrieved from https://www.lupus.org/resources/how-lupus-is-diagnosed-an-overview
Mielczarek, L. (2017). Living-Symptoms of SLE. Retrieved from https://www.lupuscanada.org/living-symptoms-of-sle
Rahman, A., & Isenberg, D. A. (2008). Systemic Lupus Erythematosus. New England Journal of Medicine, 358(9), 929–939. https://doi.org/10.1056/NEJMra071297
Suryanarayan, D. & Garcia, D. (2014). Anti-phospholipid antibodies and pregnancy. The Hematologist, 11(4). Walling, H. W., & Sontheimer, R. D. (2009). Cutaneous lupus erythematosus. American journal of clinical dermatology, 10(6), 365-381.