This is an old revision of the document!
Table of Contents
Amyotrophic lateral sclerosis (Lou Gehrig's Disease)
<style justify> Amyotrophic lateral sclerosis (ALS) is a fatal neurodegenerative disease that results in degeneration and death of motor neurons leading to muscle wasting and an inability to control voluntary movement (Leigh & Wijesekera, 2009). The ‘living wires’ which connect your brain to your muscles degenerate, leading to a loss of mobility, loss of speech and eventually impact the ability to breathe. A proposed explanation for the progression of this disease focuses on the effects of the hyperactivation of motor neurons, by the amino acid glutamate, on neuronal pathways. Treatment options include drug therapy, which interferes with the action of glutamate, and the potential to use stem cell therapy to replace malfunctioning astrocytes.
</style>
History
<style justify> Migraines are one of the oldest documented illness being described as early as 1200 BCE by the Egyptians. Arataeus of Cappadocia is however the one credited with the discovery of migraines after having extensively described unilateral headaches with aura. Migraines have plagued humans throughout our history with little progress made in the area of treatment and cures. Several treatments have been tried with no avail, including hot irons, bloodletting, inserting garlic into incisions made in the temple and applying opium and vinegar solutions directly to the skull. Some have even gone as far as to perform surgeries such as lobotomies on migraine sufferers. Trepanation involves making a hole in the skull to let out evil spirits that presumably were causing the migraine. It is possibly the oldest surgery in history and may date as far back as 6500 BCE. The first known use of medication that has shown some success is use of ergotamine in the 1930s. Ergotamine constricts blood vessels in the brain and has been shown to provide pain relief in some individuals. Many drugs have been researched and experimented with since with little success. The first and currently only class of drugs developed and used solely for the treatment of migraines are Triptans, which were developed in the early 1990s (American Migraine Foundation, 2016).
</style>
Epidemiology
<style justify> Migraines are more common in males before puberty and in females after puberty with 19% of adult women and 11% of adult males being affected (Vos, 2010). Migraines commonly begin between the ages of 15 and 24 and have an increased incidence in adults aged 35 to 45 (Bartleson, 2010). The incidence of migraines are slightly lower in Asian and African countries, but this may be partially due to lack of diagnostic resources in these areas (Wang, 2003). In the United States, 18% of men and 43% of women will experience migraines at some point in their lives with about 6% of men and 18% of women experiencing migraines in a given year. Europeans have a lifetime risk of migraine between 12 and 28%. Chronic migraines occur in about 1.4 to 2.2% of the population. Worldwide, migraines affect about 15% of the population (Vos, 2010).
</style>
Figure 1: Prevalence of migraines in Canada by age group and sex
Phases and Symptoms
<style justify>
Initial Phase: Symptoms of the initial phase include pain, feeling weak, fatigue, muscle twitching, and muscle atrophy. These symptoms lead to one tripping, dropping things, having slurred speech, having trouble swallowing or breathing, muscle cramping, and weight loss. 75% of people experience the initial symptoms one of their limbs first, which is known as “limb-onset”. 25% of the people experience trouble with speech, swallowing, and breathing first, which is known as “bulbar-onset”. (Mioshi, E. et al., 2014)
Progression: As the disease progresses, patients lose their ability to use their limbs, and therefore become unable to walk. Patients also lose their ability to speak or swallow food. Patients who experience the “limb-onset” have their symptoms progress from one limb to the other then to the rest of the body regions. Patients who experience the “bulbar-onset” have their symptoms progress to their arms then to their legs. (Hillel, A. D. et al., 1989)
Late Stages: Almost all patients with ALS end up with a respiratory failure that leads to their death within two to five years after diagnosis. However, there are some patients, around 4%, that lived with ALS for ten years or longer. (Turner, M. R. et al., 2003)
</style>
Pathophysiology
<style float-centre>
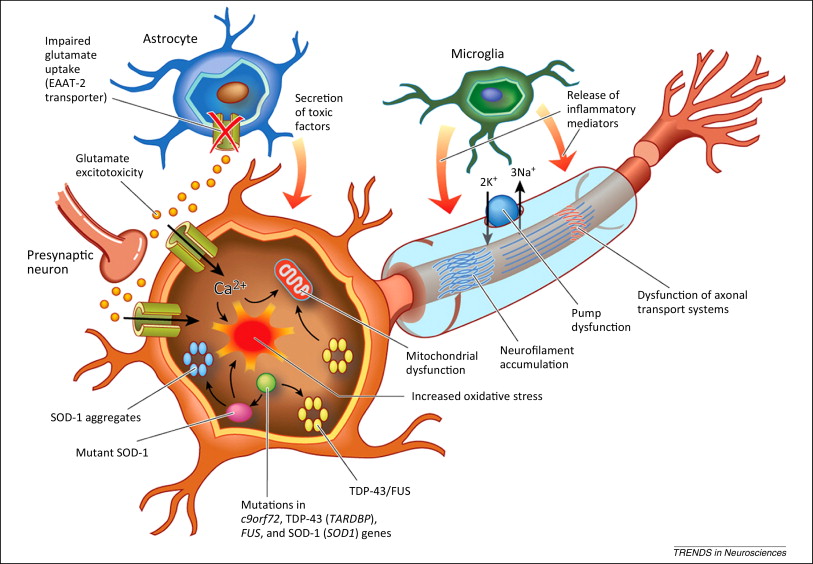
Figure 3: The Pathophysiology of ALS
</style>
<style justify>
Amyotrophic lateral sclerosis (ALS) is a progressive neurodegenerative disease that primarily involves the motor neuron system. It is characterized by the loss of motor neurons in both the brain and spinal cord (Majoor-krakauer et. al, 2011) There is no single cause of ALS, as the disease is currently characterized by its major symptom: the death of motor neurons. For this reason, it is classified as a Complex Genetic Disorder, with no single genetic or environmental factor causing onset, and a combination of factors uniquely contributing to each case (Gordon, 2011). Due to the variety of underlying causes and mechanisms that result in ALS, there are two accepted “forms” of the disease that result in similar pathophysiology. In approximately 10% of cases, ALS is a mostly genetic disease and is inherited, this is known as Familial ALS, or FALS. The other 90% is thought to be caused by a unknown mix of environmental factors as well as genetic predisposition, and is known as sporadic ALS or SALS (Kato, 2008). Both forms are poorly understood, and the major differentiator between the two is observable family history. </style>
Genetic abnormality
<style justify>
Although a consistent genetic marker has yet to be observed in FALS patients, approximately 20% of families with a history of ALS have a mutation on chromosome 21 for a gene known as SOD1, thought to code for the enzyme superoxide dismutase (Saccon et. al, 2013). The mutation on SOD1 is thought to be autosomal dominant, meaning it only has to inherited from one parent to trigger expression in the phenotype. Due, to this mutation is present in only 20% of FALS cases, it currently has no diagnostic use.
</style>
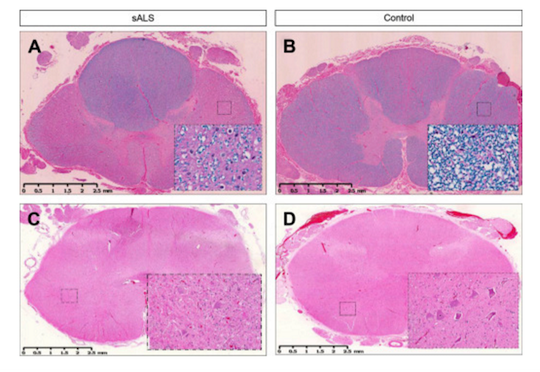
Figure 4: Lateral sclerosis is shown in the thoracic spinal cord in SALS (A) and compared with control (B). Inserts show loss of myelin in the white matter tracts under higher power (20X). Loss of motor neurons is shown in the lumbar spinal cord in SALS (C) and compared with control (D).
Bunina Bodies
<style justify>
One of the hallmarks of ALS diagnosis is the presence of Bunina Bodies, or round to oval eosinophilic intracellular inclusions in the motor neurons of the spinal cord and brain stem of both patients with sporadic ALS (SALS) and patients with familial ALS (FALS). Although Bunina bodies are present in 85-90% of ALS cases (Saberi et. al, 2015), their relationship to the underlying cause of ALS is unknown, as they test negative for a variety of biomarkers associated with neuro-degeneration. Interestingly, the only cases where Bunina bodies are absent are FALS cases that include the SOD1 mutation (Kato, 2008). Bunina bodies are shown below (denoted by black arrows) (Saberi et. al, 2015).
</style>
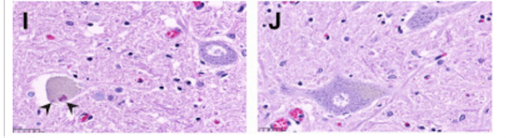
Figure 5: Black arrows indicate the presence of bunina bodies
Proteinopathy- TDP43
<style justify> A third observation of ALS proposes that the disease is a due to the presence of prions or misfolded proteins, as seen in many other neurological diseases, has been proposed. Large protein inclusions were commonly seen in the neurons of ALS patients, and in 2006, TDP-43 was identified as the major component of these inclusions. TDP-43 is a heterogeneous nuclear ribonucleoprotein and has many different cellular functions, including the stability, transport, and modification of mRNA. Mutations in the gene for TDP-43, TARDBP, have been implicated in facilitating the neurotoxic conditions of ALS, particularly in the glycine rich area of the gene (Guo et. al, 2011). This has led to the inference that variation in the mRNA metabolism is an area for further research. Similarly, to Bunina bodies, this pathology has been almost exclusively seen in ALS patients without the SOD1 mutation, suggesting that ALS can have multiple mechanisms that result in the same symptoms. </style>
Proposed Mechanism: <style justify> In healthy individuals, glutamate is released from the presynaptic neuron and activates receptors on the postsynaptic membrane (Foran & Trotti, 2009). This causes ion-gated calcium and sodium channels to open up and initiate an action potential. Glutamate transporters, located in adjacent astroglia cells, remove excess glutamate left in the synapse in order to prevent any further activation (Foran & Trotti, 2009). In patients with ALS, there is overactivation of these glutamate receptors, which can be caused by excessive glutamate release or a malfunctioning of the reuptake system on the presynaptic membrane (Foran & Trotti, 2009). This increased activation results in higher intracellular calcium concentrations that exceed the buffering capacity of the mitochondria and endoplasmic reticulum and ultimately lead to neuronal excitotoxicity and neuron death (Foran & Trotti, 2009). This abnormal increase in glutamate concentration can be linked to the presence of mutations in associated molecular factors.
Astrocytes, which absorb and recycle neurotransmitters, containing a superoxide dismutase 1 mutation (SOD1) are thought to be implicated in this hyperexcitability phenotype observed in individuals with ALS. To demonstrate the involvement of the SOD1 mutation, researchers cultured induced pluripotent stem cell-derived motor neurons with the SOD1 mutation and compared the spontaneous firing of these neurons to controls (Wainger et.al, 2014). They were able to show that SOD1 mutant neurons fired significantly more than neurons lacking this mutation supporting the idea that astrocytes are not executing their normal function (Wainger et al, 2014). When researchers corrected the mutant SOD1 gene to a wild-type, this overactivation was no longer observed (Wainger et al, 2014). Overall, the toxicity effects of this mutation are seen primarily in familial cases of ALS although astrocytes in general, play a role in both familial and sporadic forms (Wainger et al, 2014).
</style>
Treatment
To date, there is no actual cure for individuals diagnosed with ALS. Much of the treatment available is targeted around managing the symptoms and attempting to slow down the progression of the disease. There has only been one FDA approved drug therapy available with many clinical trials taking place to test more options. Overall, management of patients with ALS requires a multidisciplinary approach, with the expertise of many different health care professionals to provide the best care and least amount of suffering for these individuals.
Ergotamines:
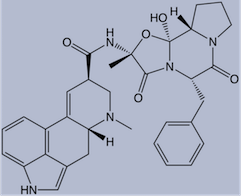
Figure 4: Chemical structure of ergotamine
</style>
<style justify> It was first isolated by Arthur Stole in 1918 and first used as a treatment option for migraines in 1925 (Kalra & Elliott, 2007). Its chemical structure is similar to that of amines, serotonin, norepinephrine and dopamine. The mode of action of ergotamine in migraine may be by means of selective arterial vasoconstriction on certain cranial vessel beds or, alternatively, by depression of central serotonergic neurons mediating pain transmission or circulatory regulation (Kalra & Elliott, 2007). They have a complex mode of action that involves interaction with a variety of receptors which include 5-HT, dopamine and noradrenaline.
2 modes of action related to migraine:
1.Activation of 5-HT1B receptors located on intracranial blood vessels, leads to vasoconstriction of blood vessels (Kalra & Elliott, 2007).
2.Activation of 5-HT1D receptors on sensory nerve endings of trigeminal system, inhibits pro-inflammatory neuropeptide release (Kalra & Elliott, 2007).
Oral absorption of ergotamine is about 60-70% and the concurrent administration of caffeine improves both the rate and extent of absorption (Tfelt-hansen et al, 2000). Due to high first-pass metabolism, ergotamine has a very low bioavailability from oral administration (Tfelt-hansen et al, 2000). Ergotamine and ergotamine-caffeine combination pills still play a role in the acute treatment of migraine in those patients who do not respond adequately to triptan therapy. Ergotamine has more side effects (nausea, vomiting, peripheral and coronary vasoconstriction) due to its relatively nonselective adherence to serotonin, dopamine and adrenergic receptors (Tfelt-hansen et al, 2000). </style>
Figure 5: Placebo controlled clinical trial with ergotamine
</style>
<style justify>
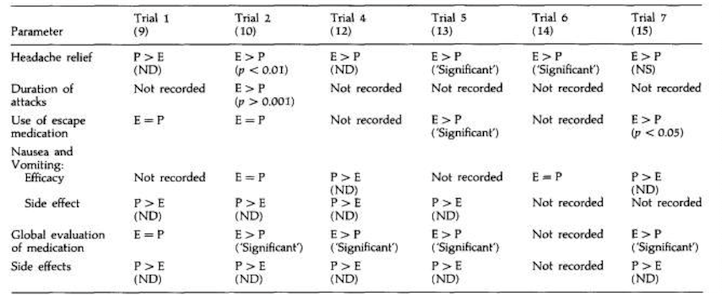
The study conducted by Dahlof, 1993 looked at the effect of ergotamines on headache relief in people presenting with symptoms of migraines. In comparison to the placebo treatment, ergotamines were found to be more effective in the relief of headache in 5 out of the 6 trials. In three of the trials, there was a statistically significant difference. The combination of ergotamine and caffeine was used in three of the studies (12,13,15). Caffeine was included to improve absorption and efficacy. In the other trial, ergotamine was given together with caffeine, belladonna alkaloids and a barbiturate (11).This combination of drugs is significantly more effective than ergotamine alone in relieving migraine headache and other symptoms (12).
Nausea and vomiting: All ergotamine trials evaluated had some analysis of nausea and/or vomiting. In the four trials where efficacy assessments were made, nausea and/or vomiting either increased in severity after treatment with ergotamine, and more patients were affected than was observed with placebo or there was little difference between the two treatments (10, 12, 14, 15). In all trials where the symptoms were assessed as side effects, more patients were affected following ergotamine than following placebo (9, 10, 12, 13) (Dahlof, 1993).
Global evaluation of medication: Five of the ergotamine trials evaluated presented results for patients’ preference for ergotamine or placebo. In four trials, significantly more patients preferred ergotamine to placebo (10, 12, 13, 15). In the fifth trial, similar numbers of patients clinically diagnosed as having migraine preferred placebo to ergotamine as preferred ergotamine to placebo (13) (Dahlof, 1993).
Side effects : The side effect profile of ergotamine and placebo was reported in five of the six trials evaluated (9, 10, 12, 13, 15). In all these trials more patients reported side effects with ergotamine than with placebo. Side effects associated with ergotamine included nausea/ vomiting, dizziness/vertigo, drowsiness/tiredness, numbness, nervousness, trembling, dyspnoea and dry mouth (Dahlof, 1993). </style>
Triptans
<style justify> Triptans like Sumatriptan were developed to treat migraines in the early 1990s. They effectively relieve pain and nausea in approximately 75% of people. Triptans are often reserved for use in those with moderate to severe pain and for those who do not respond to analgesics (Johnston, 2010). They are administered as oral tablets, injections, nasal sprays and pills. Side effects include tingling, pain and tightness in the chest or throat, vomiting, dry mouth, flushing, dizziness and fatigue. In rare cases they can lead to cardiac ischemia (Gilmore, 2011). Triptans act in a similar manner as the ergotamines but are more selective and therefore have less side effects. Triptans are selective 5-hydroxytryptamine (5-HT) receptor agonists with high affinity for 5-HT1B and 5-HT1D receptors. These receptors when activated, constrict blood vessels in the brain to provide relief (Bartleson, 2010). Triptans are often avoided in patients who have cardiovascular disease, a history of stroke or have migraines accompanied by neurological problems. Patients should be evaluated for their risk of developing vascular disease before prescription for triptans is given. Triptans are not addictive but when used frequently, such as 10 or more days per month, medication overuse headaches can result. </style>
Cardiovascular medications in the treatment of migraine
Researchers do not yet understand how exactly beta blockers prevent migraines. They are traditionally used for cardiology patients to prevent the stimulation of adrenergic receptors responsible for increased cardiac action. For treating migraines it is thought that they act through beta1 adrenoreceptor inhibition of the activation of third order trigeminovascular nociceptive neurons. The beta blockers propranolol (Inderal La, Innopran XL, others), metoprolol tartrate (Lopressor) and timolol (Betimol) have proved effective for preventing migraines. You may not notice improvement in symptoms for several weeks after taking these medications. However, the usage of beta blockers are not advised if you are over 60, have heart or blood vessel conditions or use tobacco.
Another class of cardiovascular medications (calcium channel blockers) used to treat high blood pressure and keep blood vessels from becoming narrow or wide, also may be helpful in preventing migraines and relieving symptoms of an attack. The use of calcium channel blockers comes from the idea that migraine may be due to a mutation in calcium channels that make them hyperexcitable and as such this medication can help to counteract this effect. Verapamil (Calan, Verelan, others) is a calcium channel blocker that may help you.
Analgesics
<style justify> Most first line treatments for migraines are analgesics. Generally, these treatments are used as a primary option in severe cases, and are used when the symptoms of a migraine have just manifested themselves, as to prevent further progression. Analgesics are classified as a non-specific treatment when used in the treatment of migraines, as they are used in the treatment of other conditions as well (Pfaffenrath, 1995). As such, they are often used in combination with migraine specific therapies. Common analgesics for migraines are usually a class of drug known as Non-steroidal Anti-inflammatory Drugs (NSAIDS) such as Aspirin and Aleve. NSAIDS are generally used for moderate to severe migraines and are the final non specific treatment for migraines, as they treat the symptoms of migraines, rather than the underlying cause (Pfaffenrath, 1995). </style>
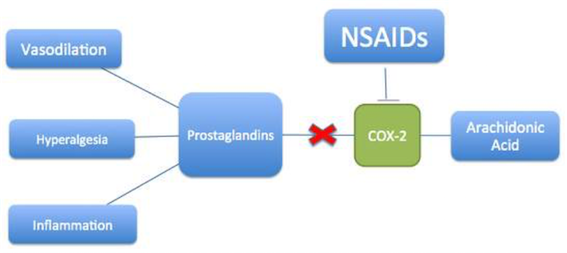
Figure 6: Mechanism of action of NSAIDs
</style>
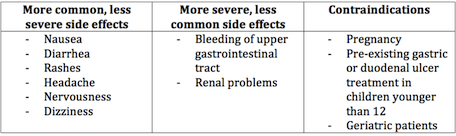
<style justify> NSAIDs work by inhibiting the production of prostaglandins, which are the chemical messengers that initiate the pain and inflammation response (Whalen, K., 2012). Tissue in the human body produces prostaglandins in response to damage, and prostaglandins increase sensitivity in the nerves that send the pain response to the brain, thus establishing the pain threshold (Whalen, K., 2012). The mechanism by which NSAIDs prevent prostaglandin synthesis is by the inhibition of the cyclooxygenase (COX) enzymes that are found in their metabolic pathway [Figure 6] (European Neurological Review, 2011). There are two classes of COX enzymes, and most traditional NSAIDs that are used to treat migraines inhibit both COX-1 and COX-2. COX-1 is constitutive, while COX-2 is induced by injury (European Neurological Review, 2011). The reduction of prostaglandins inhibits pain signaling to the brain, ergo aiding in migraine management. </style>
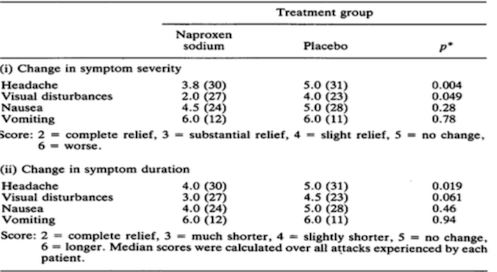
Figure 7: Effectiveness of NSAIDs in treatment of symptoms (Johnson et. al, 1985)
</style>
<style justify> Effectiveness of NSAIDs in the treatment of symptoms: Seventy patients with classical or common migraine were treated during their attacks with either naproxen sodium or placebo in a randomised, double-blind parallel group study (Johnson et. al, 1985). The initial dose of naproxen sodium was 825 mg followed one hour later by a further 550 mg, if symptoms were the same or had improved (Johnson et. al, 1985). Patients were seen at admission and then at monthly intervals until a total of ten attacks had been studied. During each attack the patient graded the severity of headache, visual disturbance, nausea and other important symptoms (specific to the patient) as none, mild, moderate or severe. In Figure 7, Naproxen sodium produced statistically significantly superior relief of headache in comparison with placebo (p= 0.004) and the duration of headache was significantly shorter in this group than in the placebo group (p= 0.019) (Johnson et. al, 1985). Patients in the naproxen sodium group also had a significant reduction in the severity of visual disturbances when compared with those in the placebo group (= 0.049). The differences detected between the groups with respect to the severity of nausea and vomiting and the duration of the visual disturbances, nausea and vomiting were not significant, but the score for the naproxen sodium group was numerically lower for the severity of nausea and for the duration of both visual disturbances and nausea (Johnson et. al, 1985). Scores for the severity and duration of vomiting were the same for both groups. In summary, naproxen sodium has proved to be a drug effective in relieving symptoms associated with common migraine when taken at the onset of an attack. </style>
Calcitonin gene related peptide antagonists
Currently CGRP1 antagonists hold promise as new anti-migraine drugs. Two recently introduced are: BIBN4096BS and Compound 1 (Kalra & Elliott, 2007). BIBN4096BS was tested in the trigeminal ganglion and found to inhibit vasodilatation (Kalra & Elliott, 2007). Other experiments support its possible role as an anti-nociceptor mediator in migraine. Compound 1 has similar properties but is less potent than BIBN4096BS in human tissues (Kalra & Elliott, 2007). A third smaller CGRP antagonistic molecule is SB-273779. It has similar properties as the other two but may have greater value for the study of migraine and CGRP activity in animal models (Kalra & Elliott, 2007). The efficacy of BIBN4096BS has been tested in humans in two studies published in 2004. In the first, the safety, tolerability and pharmacokinetics of BIBN4096BS were tested in healthy volunteers. After a single IV administration of gradually increasing dose, most of the adverse events occurred at the highest administered dose (10 mg) and were relatively mild and transient (Iovino et al 2004). In another controlled study, moderate or severe headache was treated with 2.5 mg of BIBN4096BS IV vs. placebo. The end-point of pain reduction within 2 hours to mild or no pain was achieved in 66% of BIBN4096BS treated patients vs. 27% of the placebo group (Doggrell 2004). In clinical practice, its potential use will be limited to settings appropriate for IV administration.
Surgery and Devices
Surgery
<style justify> Recently Plastic surgeons have advertised nerve decompression surgery as an innovative new treatment of migraine headaches. In the 1990s, the use of the muscle relaxant Botulinum toxin became popular in the treatment of chronic migraine. Its effect was thought to occur through paralysis of muscles surrounding nerves in areas of pain. This operation involves the removal of a muscle in an area of the forehead where patients experience migraine pain. The idea for surgery began with patients reporting that their headaches were disappearing after forehead rejuvenation plastic surgery (Migraine surgery Centre London, 2016). Combined, these observations led to a theory that migraine headache pain can be triggered by compression of superficial nerves by surrounding tissues, such as muscle, fascia, and bone. During nerve-decompression migraine surgery, nerves at one or multiple common migraine headache trigger sites are released from surrounding structures such as bone, muscle, fascia, and vessels (Migraine surgery Centre London, 2016). The Surgical Migraine Procedure is the removal of the corrugator muscles (small muscles associated with the eyebrows) (Migraine surgery Centre London, 2016). However, the efficacy of this method beyond placebo has been debated in the medical community. </style>
Devices
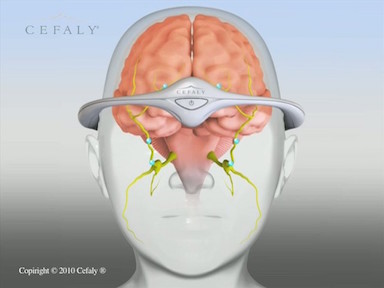
<style justify> Neurostimulation is the practice of applying gentle stimulation to nerves that have been identified as sending strong, frequent pain signals.
The Cefaly is a headband designed to deliver electrical impulses to nerves that transmit migraine pain and thereby theoretically suppress this trigger mechanism. To reduce the frequency of headaches, it is to be worn for 20 minutes every day (Didier et. al, 2015). The device consists of a battery-operated electrical pulse generator and a self-adhesive electrode (Didier et. al, 2015). The patient applies the electrode to the middle of the forehead and lowers a headband containing the electrical pulse generator over the forehead to engage a pin located on the electrode. Pressing a button on the band generates a pulsed electric current that stimulates the upper branches of the trigeminal nerve, producing a tingling or massaging sensation (Didier et. al, 2015). During the treatment, which has a fixed duration of 20 minutes, the intensity of the electric current gradually increases. </style>
http://www.cefaly.ca/#howitworks
https://www.youtube.com/watch?v=S_p0WlJd_dw
Conclusion
Overall, migraines are a heterogenous, burdensome disorder that are debilitating for the individuals experiencing them. There appears to be a strong link between genetics and environment in making individuals susceptible to migraine attacks. Symptoms can vary from one individual to the next and exacerbating factors can have different effects on different individuals. Our proposed course of treatment is to use non-steroidal anti-inflammatory drugs with caffeine administration to alleviate pain in migraine sufferers. Studies have shown that NSAIDs are significantly more effective at relieving symptoms of headache compared to other proposed therapeutics. NSAIDs, like Naproxen, are much more cost-effective, have a longer lasting effect, have a reduced likelihood of producing rebound headaches, show low reports of adverse affects and are non-addictive. It has been shown that co-administration with caffeine promote more effective intestinal absorption and a higher likelihood of a positive treatment response. Great progress has been made in understand migraine pathophysiology as well as defining new specific therapies. In recognition of the large market of migraine sufferers, the pharmaceutical and bioengineering industries are working towards newer and better approaches for affective interventions.