Table of Contents
Amyotrophic lateral sclerosis (Lou Gehrig's Disease)
<style justify> Amyotrophic lateral sclerosis (ALS) is a fatal neurodegenerative disease that results in degeneration and death of motor neurons leading to muscle wasting and an inability to control voluntary movement (Leigh & Wijesekera, 2009). The ‘living wires’ which connect your brain to your muscles degenerate, leading to a loss of mobility, loss of speech and eventually impact the ability to breathe. A proposed explanation for the progression of this disease focuses on the effects of the hyperactivation of motor neurons, by the amino acid glutamate, on neuronal pathways. Treatment options include drug therapy, which interferes with the action of glutamate, and the potential to use stem cell therapy to replace malfunctioning astrocytes.
</style>
History
<style justify> Jean- Marie Charcot (1825-1893) noted the first reports of the characteristics of ALS in 1874, and named the fatal syndrome based on what he found. He was a noted French neurologist who explained how the central nervous system works and who has been called “the Father of Neurology”. (Rowland, 2001) </style>
Figure 1: Famous physicist Stephen Hawking
</style> <style justify> Drs. Scarmeas, Shih, Stern, Ottoman, and Rowland recently published a scientific article, concluding that subjects with motor neuron diseases were more likely to be slim, or had once been serious athletes. Many famous people in US history have had ALS (Scarmeas, N. et al., 2002). For example:
- Lou Gehrig was a very famous Yankee baseball player
- Ezzard Charles was a heavyweight-boxing champion
- Catfish Hunter- baseball player
- Senator Jacob Javits was an avid tennis player
- David Niven was a competitive sailor.
- Stephen Hawking, the famous physicist
- Even some in the musical field were subjected to ALS; Dimitri Shostakovitch and Charles Mingus both vigorously practiced musical instruments
</style>
Epidemiology
<style justify> ALS strikes about six to eight people per 100,000 (ALS Society of Canada, 2012).In any given year, about two new cases of ALS per 100,000 people will be diagnosed (ALS Society of Canada, 2012). In the US, approximately 5,000 people are diagnosed yearly with ALS (Kiernan, MC. et al., 2011).. With an estimated Canadian population of 34 million, approximately 2,000 - 3,000 people in Canada currently have ALS (ALS Society of Canada, 2012). The incidence (new cases) of ALS increases with age. Most are between the ages of 40-70, but it can also occur in older and younger adults, and rarely in teenagers. Presently in the United States, about 30,000 people are victims of ALS; most will die within 3-5 years of contracting the fatal syndrome. Ten percent of all known cases are hereditary. Although males are more prone to ALS, the condition has no racial, ethnic or socioeconomic boundaries (Kiernan, MC. et al., 2011).
</style>
Figure 2: The figure shows prevalence rates per 100,000 population for cases of amyotrophic lateral sclerosis in the United States, by age group, on the basis of data from the National ALS Registry for October 19, 2010-December 31, 2011. Prevalence rates were highest for persons aged 70-79 years and lowest for those aged 18-39 years. Available at: http://www.cdc.gov/als.
Phases and Symptoms
<style justify>
Initial Phase: Symptoms of the initial phase include pain, feeling weak, fatigue, muscle twitching, and muscle atrophy. These symptoms lead to one tripping, dropping things, having slurred speech, having trouble swallowing or breathing, muscle cramping, and weight loss. 75% of people experience the initial symptoms one of their limbs first, which is known as “limb-onset”. 25% of the people experience trouble with speech, swallowing, and breathing first, which is known as “bulbar-onset”. (Mioshi, E. et al., 2014)
Progression: As the disease progresses, patients lose their ability to use their limbs, and therefore become unable to walk. Patients also lose their ability to speak or swallow food. Patients who experience the “limb-onset” have their symptoms progress from one limb to the other then to the rest of the body regions. Patients who experience the “bulbar-onset” have their symptoms progress to their arms then to their legs. (Hillel, A. D. et al., 1989)
Late Stages: Almost all patients with ALS end up with a respiratory failure that leads to their death within two to five years after diagnosis. However, there are some patients, around 4%, that lived with ALS for ten years or longer. (Turner, M. R. et al., 2003)
ALS does not affect the five senses of sight, hearing, taste, smell and touch, nor does it normally affect the eye muscles, heart, bladder, bowel, or sexual muscles.
</style>
Pathophysiology
<style float-centre>
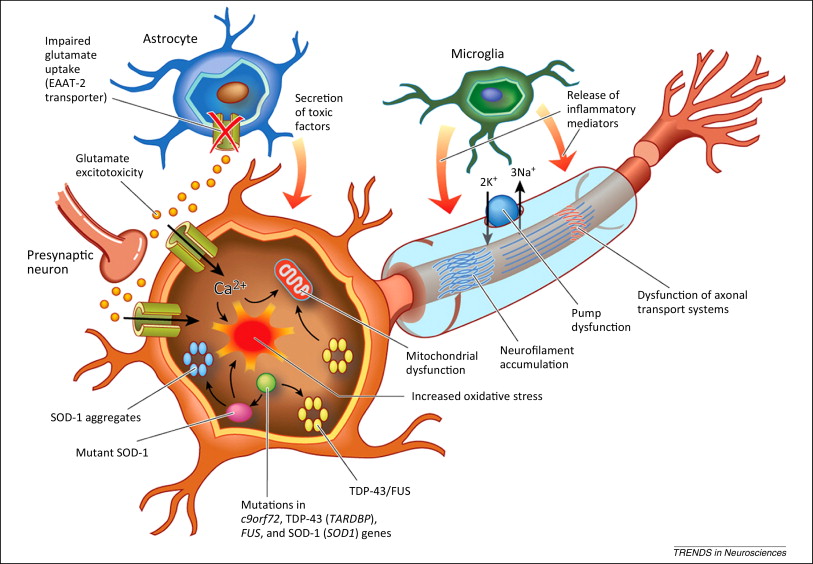
Figure 3: The Pathophysiology of ALS (Vucic et al, 2014)
</style>
<style justify>
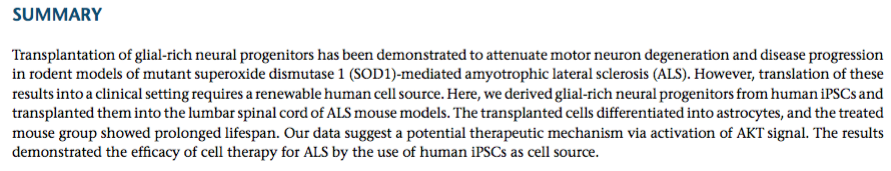
Amyotrophic lateral sclerosis (ALS) is a progressive neurodegenerative disease that primarily involves the motor neuron system. It is characterized by the loss of motor neurons in both the brain and spinal cord (Majoor-krakauer et. al, 2011) There is no single cause of ALS, as the disease is currently characterized by its major symptom: the death of both upper and lower motor neurons. For this reason, it is classified as a Complex Genetic Disorder, with no single genetic or environmental factor causing onset, and a combination of factors uniquely contributing to each case (Gordon, 2011). Due to the variety of underlying causes and mechanisms that result in ALS, there are two accepted “forms” of the disease that result in similar pathophysiology. In approximately 10% of cases, ALS is a mostly genetic disease and is inherited, this is known as Familial ALS, or FALS. The other 90% is thought to be caused by a unknown mix of environmental factors as well as genetic predisposition, and is known as sporadic ALS or SALS (Kato, 2008). Both forms are poorly understood, and the major differentiator between the two is observable family history. </style>
Genetic abnormality
<style justify>
Although a consistent genetic marker has yet to be observed in FALS patients, approximately 20% of families with a history of ALS have a mutation on chromosome 21 for a gene known as SOD1, thought to code for the enzyme superoxide dismutase (Saccon et. al, 2013). The mutation on SOD1 is thought to be autosomal dominant, meaning it only has to inherited from one parent to trigger expression in the phenotype. Due, to this mutation is present in only 20% of FALS cases, it currently has no diagnostic use.
</style>
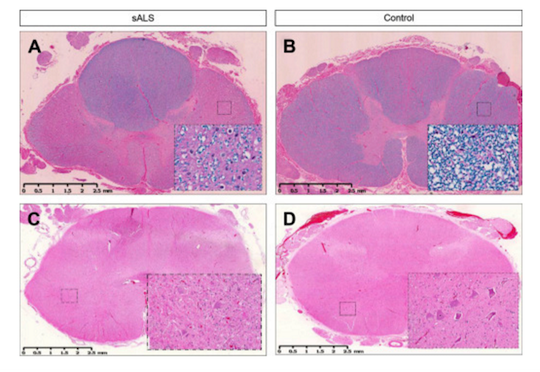
Figure 4: Lateral sclerosis is shown in the thoracic spinal cord in SALS (A) and compared with control (B). Inserts show loss of myelin in the white matter tracts under higher power (20X). Loss of motor neurons is shown in the lumbar spinal cord in SALS (C) and compared with control (D).
Bunina Bodies
<style justify>
One of the hallmarks of ALS diagnosis is the presence of Bunina Bodies, or round to oval eosinophilic intracellular inclusions in the motor neurons of the spinal cord and brain stem of both patients with sporadic ALS (SALS) and patients with familial ALS (FALS). Although Bunina bodies are present in 85-90% of ALS cases (Saberi et. al, 2015), their relationship to the underlying cause of ALS is unknown, as they test negative for a variety of biomarkers associated with neuro-degeneration. Interestingly, the only cases where Bunina bodies are absent are FALS cases that include the SOD1 mutation (Kato, 2008). Bunina bodies are shown below (denoted by black arrows) (Saberi et. al, 2015).
</style>
Figure 5: Black arrows indicate the presence of bunina bodies
Proteinopathy- TDP43
<style justify> A third observation of ALS proposes that the disease is a due to the presence of prions or misfolded proteins, as seen in many other neurological diseases, has been proposed. Large protein inclusions were commonly seen in the neurons of ALS patients, and in 2006, TDP-43 was identified as the major component of these inclusions. TDP-43 is a heterogeneous nuclear ribonucleoprotein and has many different cellular functions, including the stability, transport, and modification of mRNA. Mutations in the gene for TDP-43, TARDBP, have been implicated in facilitating the neurotoxic conditions of ALS, particularly in the glycine rich area of the gene (Guo et. al, 2011). This has led to the inference that variation in the mRNA metabolism is an area for further research. Similarly, to Bunina bodies, this pathology has been almost exclusively seen in ALS patients without the SOD1 mutation, suggesting that ALS can have multiple mechanisms that result in the same symptoms. </style>
Proposed Mechanism: <style justify> In healthy individuals, glutamate is released from the presynaptic neuron and activates receptors on the postsynaptic membrane (Foran & Trotti, 2009). This causes ion-gated calcium and sodium channels to open up and initiate an action potential. Glutamate transporters, located in adjacent astroglia cells, remove excess glutamate left in the synapse in order to prevent any further activation (Foran & Trotti, 2009). In patients with ALS, there is overactivation of these glutamate receptors, which can be caused by excessive glutamate release or a malfunctioning of the reuptake system on the presynaptic membrane (Figure 3) (Foran & Trotti, 2009). This increased activation results in higher intracellular calcium concentrations that exceed the buffering capacity of the mitochondria and endoplasmic reticulum and ultimately lead to neuronal excitotoxicity and neuron death (Figure 3) (Foran & Trotti, 2009). This abnormal increase in glutamate concentration can be linked to the presence of mutations in associated molecular factors.
Astrocytes, which absorb and recycle neurotransmitters, containing a superoxide dismutase 1 mutation (SOD1) are thought to be implicated in this hyperexcitability phenotype observed in individuals with ALS. To demonstrate the involvement of the SOD1 mutation, researchers cultured induced pluripotent stem cell-derived motor neurons with the SOD1 mutation and compared the spontaneous firing of these neurons to controls (Wainger et.al, 2014). They were able to show that SOD1 mutant neurons fired significantly more than neurons lacking this mutation supporting the idea that astrocytes are not executing their normal function (Wainger et al, 2014). When researchers corrected the mutant SOD1 gene to a wild-type, this overactivation was no longer observed (Wainger et al, 2014). Overall, the toxicity effects of this mutation are seen primarily in familial cases of ALS although astrocytes in general, play a role in both familial and sporadic forms (Wainger et al, 2014).
</style>
Treatment
<style justify> To date, there is no actual cure for individuals diagnosed with ALS. Much of the treatment available is targeted around managing the symptoms and attempting to slow down the progression of the disease. There has only been one FDA approved drug therapy available with many clinical trials taking place to test more options. Overall, management of patients with ALS requires a multidisciplinary approach, with the expertise of many different health care professionals to provide the best care and least amount of suffering for these individuals. </style>
Pharmacologic treatment: Riluzole
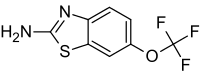
Figure 6: Chemical structure of the drug Riluzole
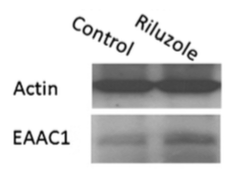
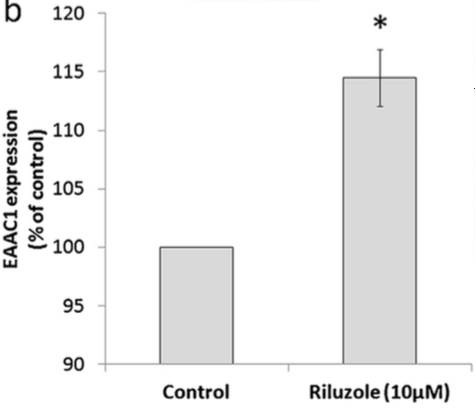
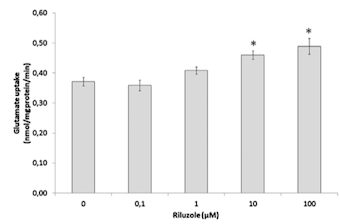
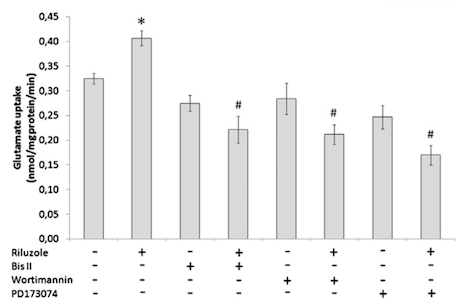
</style> <style justify> The only FDA approved treatment available to date is the drug Riluzole, which is thought to extend life expectancy by 2-3 months (Dall'Igna et. al, 2013). It belongs to the class of drugs known as antiglutamates and whose chemical formula is C8H5F3N2OS (Figure 6). It functions to prevent the overactivation of neurons by regulating neurotransmitter activity and inhibiting neuronal firing (Dall’Igna et al, 2013). Dall’Igna et. al (2013) studied the influence of riluzole on glutamate uptake at doses that did not induce damage on the studied cells within a 1 h time frame (0.1–100 M). One hour pre-incubation of riluzole significantly enhanced glutamate uptake in C6 astroglial cell cultures (Figure 8a). In further studies, the researchers chose the lowest effective dose of riluzole to alter glutamate uptake (10 M). Because EAAC1 is the main glutamate transporter in C6 astroglial cells, they analyzed the effect of riluzole on EAAC1 expression (Figure 7). Treatment with 10 M riluzole for 1 h induced an 18% increase in the expression of EAAC1 transporter as detected by Western blotting, indicating a possible mechanism for the increase in glutamate uptake (Figure 7). The increase in glutamate uptake was demonstrated to be dependent on PKC, PI3K and ERK intracellular pathways; riluzole had the opposite effect on glutamate uptake when it was added simultaneously with inhibitors of these enzymes (Figure 8b). Co-incubation of riluzole with the inhibitors of PKC (bisindolylmaleimide II), PI3K (wortmannin) or FGFR (PD173074) not only blocked the stimulatory effect of riluzole on glutamate uptake, but the riluzole plus inhibitor combination also decreased glutamate uptake levels to below the basal controls (Figure 8b). Such effects occurred in doses of bisindolylmaleimide II, wortmannin and PD173074 that alone had no significant effect on basal glutamate uptake (Dall'Igna, 2013). </style>
Figure 7: EAAC1 expression, measured by Western blotting with specific antibody, in C6 astroglial cells in the presence or absence of riluzole. Cells were pretreated with riluzole for 1 h in DMEM without serum.
Figure 8: (a) Glutamate uptake in C6 astroglial cells in the presence or absence of riluzole. (b)Glutamate uptake in C6 astroglial cells in the presence or absence of riluzole and/or of the inhibitor of protein kinase C (PKC) bisindolylmaleimide II (Bis II), the inhibitor of phosphatidylinositol 3-kinase (PI3K) wortimannin or the inhibitor of extracellular-signal regulated kinase (ERK) PD173074.
Management strategies
Managing ALS is a continually changing challenge. Although ALS is a degenerative disease, the rate at which neurons and muscles degenerate is unpredictable and varies greatly from one individual to another. In some cases the disease seems to have reached a plateau, while in others it reaches a standstill for varying lengths of time. Also, ALS can progress steadily at a rapid or slow rate. Whatever the rate of muscle degeneration, individuals should remain as active as possible, without causing fatigue in affected muscles. Many health care professionals are involved including: the family doctor, neurologist, palliative care doctor, nurse clinicians, occupational therapist, physiotherapist, psychiatrist, dietician, respiratory therapist, speech-language pathologist and social worker (ALS Society of Canada, 2012). This speaks to the diverse nature of the symptoms and the multitude and magnitude of expertise required.
Management options focus on aiding the individual with:
- changes in mobility
- swallowing problems and maintaining good nutrition (i.e. tube feeding)
- changes in speech and maintaining communication
- changes in breathing and maintaining lung function
Future directives: stem cell therapy
Another potential, but preclinical therapeutic option is the use of human induced pluripotent stem cells (hIPSCs) that can differentiate to become healthy astrocytes (Kondo et al, 2014). Researchers transplanted hIPSCs into the spine of mSOD1 mice subjects after disease onset and observed differentiation of these cells into astrocytes and an overall prolonged lifespan (Kondo et al, 2014). The ability to generate functional astrocytes, to compensate for mutated ones, can be advantageous in rescuing motor neurons as it will allow for glutamate to be properly removed from the synapse, which will prevent hyperexcitability of the postsynaptic membrane.
Conclusion
Overall, ALS is a rapidly, progressing disease that greatly impacts the everyday functioning of the individual who has it. ALS destroys motor neurons which are an important link in the nervous system. It is through motor neurons that the brain sends messages to the voluntary muscles throughout the body which leads to the individual losing the ability to walk, talk and breath. ALS is now recognized to have multiple interacting causes, all sharing a common pathway leading to the destruction of the motor neurons. Glutamate excitotoxicity in ALS patients can be linked to mutant astrocytes that malfunction and this can be the target of potential therapies. Drug therapy has shown promising temporary effects and although more research needs to be done, there is the potential to use innovative stem cell therapeutics to introduce healthy astrocytes into neuronal regions for longer-term effects.
References
Als society of canada. (2012). A Manual for People Living with ALS. (7th ed.). Retrieved 27 March, 2016, from https://www.als.ca/sites/default/files/files/ALS%20Manual/2012%20Manual%20People%20Living%20With%20ALS%20-%20ENGLISH%20Final.pdf
Cifra, A., Nani, F., & Nistri, A. (2011). Riluzole is a potent drug to protect neonatal rat hypoglossal motoneurons in vitro from excitotoxicity due to glutamate uptake block. European Journal of Neuroscience, 33, 899-913.
Dall'Igna, O., Bobermin, L., Souza, D., & Santos, A. (2013). Riluzole increases glutamate uptake by cultured C6 astroglial cells. International Journal of Developmental Neuroscience, 31, 482-486.
Gijn, J. (2011). Charles Bell (1774–1842). Journal of Neurology J Neurol 258, 1189–1190.
Gordon PH. Amyotrophic lateral sclerosis: pathophysiology, diagnosis and management. CNS Drugs. 2011;25(1):1-15.
Guo W, Chen Y, Zhou X, et al. An ALS-associated mutation affecting TDP-43 enhances protein aggregation, fibril formation and neurotoxicity. Nat Struct Mol Biol. 2011;18(7):822-30.
Foran, E., & Trotti, D. (2009). Glutamate transporters and the excitotoxic path to motor neuron degeneration in amyotrophic lateral sclerosis. Antioxidants & Redox Signaling, 11(7)
Hillel, A. D., Miller, R. M., Yorkston, K., McDonald, E., Norris, F. H., & Konikow, N. (1989). Amyotrophic lateral sclerosis severity scale. Neuroepidemiology, 8(3), 142-150.
Kato S. Amyotrophic lateral sclerosis models and human neuropathology: similarities and differences. Acta Neuropathol. 2008;115(1):97-114.
Kiernan, MC; Vucic, S; Cheah, BC; Turner, MR; Eisen, A; Hardiman, O; Burrell, JR; Zoing, MC (12 March 2011). “Amyotrophic lateral sclerosis.”. Lancet 377 (9769): 942–55. doi:10.1016/s0140- 6736(10)61156-7. PMID 21296405.
Kondo, T. et al. (2014). Focal transplantation of human iPSC-derived glial-rich neural progenitors improves lifespan of ALS mice. Stem Cell Reports, 3(2), 242-249.
Mackenzie IR, Rademakers R, Neumann M. TDP-43 and FUS in amyotrophic lateral sclerosis and frontotemporal dementia. Lancet Neurol. 2010;9(10):995-1007.
Majoor-krakauer D, Willems PJ, Hofman A. Genetic epidemiology of amyotrophic lateral sclerosis. Clin Genet. 2003;63(2):83-101.
Mioshi, E., Hsieh, S., Caga, J., Ramsey, E., Chen, K., Lillo, P., … & Kiernan, M. C. (2014). A novel tool to detect behavioural symptoms in ALS. Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration, 15(3-4), 298-304.
Rowland LP (March 2001). “How amyotrophic lateral sclerosis got its name: the clinical-pathologic genius of Jean-Martin Charcot”. Arch. Neurol. 58 (3): 512–5. doi:10.1001/archneur.58.3.512. PMID 11255459
Saberi S, Stauffer JE, Schulte DJ, Ravits J. Neuropathology of Amyotrophic Lateral Sclerosis and Its Variants. Neurol Clin. 2015;33(4):855-76.
Saccon RA, Bunton-stasyshyn RK, Fisher EM, Fratta P. Is SOD1 loss of function involved in amyotrophic lateral sclerosis?. Brain. 2013;136(Pt 8):2342-58.
Scarmeas, N., Shih, T., Stern, Y., Ottman, R., & Rowland, L. P. (2002). Premorbid weight, body mass, and varsity athletics in ALS. Neurology, 59(5), 773-775.
Turner, M. R., Parton, M. J., Shaw, C. E., Leigh, P. N., & Al-Chalabi, A. (2003). Prolonged survival in motor neuron disease: a descriptive study of the King’s database 1990–2002. Journal of Neurology, Neurosurgery & Psychiatry, 74(7), 995-997
Wijesekera, L., & Leigh, P. (2009). Amyotrophic lateral sclerosis. Orphanet Journal of Rare Diseases, 4(3)