This is an old revision of the document!
Table of Contents
Migraines
<style justify> A migraine is a debilitating, recurring, primary headache disorder. Genetic mutations in the CACNA1A gene, coding for voltage-gated calcium channels, have been implicated in about half the cases of familial hemiplegic migraine (FHM). The onset of migraines can be due to the hyperexcitability of trigeminal neurons and the abnormal integration of sensory information. Consequently, the individual may experience symptoms such as nausea, change in appetite, decreased cognitive ability, visual disturbances and lightheadedness. These symptoms may last anywhere from 4-72 hours. While there is no cure for migraines, there are drug therapeutics targeted at pain relief and prevention. New therapies related to neurostimulation are emerging but more research needs to be done. Overall, migraine is underdiagnosed and undertreated and improvements from the clinical end are needed.
</style>
History
<style justify> Migraines are one of the oldest documented illness being described as early as 1200 BCE by the Egyptians. Arataeus of Cappadocia is however the one credited with the discovery of migraines after having extensively described unilateral headaches with aura. Migraines have plagued humans throughout our history with little progress made in the area of treatment and cures. Several treatments have been tried with no avail, including hot irons, bloodletting, inserting garlic into incisions made in the temple and applying opium and vinegar solutions directly to the skull. Some have even gone as far as to perform surgeries such as lobotomies on migraine sufferers. Trepanation involves making a hole in the skull to let out evil spirits that presumably were causing the migraine. It is possibly the oldest surgery in history and may date as far back as 6500 BCE. The first known use of medication that has shown some success is use of ergotamine in the 1930s. Ergotamine constricts blood vessels in the brain and has been shown to provide pain relief in some individuals. Many drugs have been researched and experimented with since with little success. The first and currently only class of drugs developed and used solely for the treatment of migraines are Triptans, which were developed in the early 1990s.
</style>
Epidemiology
<style justify> Migraines are more common in males before puberty and in females after puberty with 19% of adult women and 11% of adult males being affected (Vos, 2010). Migraines commonly begin between the ages of 15 and 24 and have an increased incidence in adults aged 35 to 45 (Bartleson, 2010). The incidence of migraines are slightly lower in Asian and African countries, but this may be partially due to lack of diagnostic resources in these areas (Wang, 2003). In the United States, 18% of men and 43% of women will experience migraines at some point in their lives with about 6% of men and 18% of women experiencing migraines in a given year. Europeans have a lifetime risk of migraine between 12 and 28%. Chronic migraines occur in about 1.4 to 2.2% of the population. Worldwide, migraines affect about 15% of the population (Vos, 2010).
</style>
Figure 1: Prevalence of migraines in Canada by age group and sex
Risk Factors
<style justify> There are several factors that make one more prone to getting migraines.
Family History: Upto 90% of people who suffer from migraines have family members who have had the same condition. If one or both of your parents have migraines, then there is a good chance that you would suffer from migraine attacks.
Age: One can develop migraines at any age, but most people who suffer from migraine attacks get their first attack during adolescence. By age 40, most people who suffer from migraines would got their first migraine attack.
Sex: Women are 3 times more likely to suffer from migraine attacks than men. Boys tend to get more headaches than girls during childhood, but during and after puberty, girls suffer from migraines overwhelmingly more than boys.
Hormonal changes: Women are more susceptible to migraines during the onset or immediately after menstruation.
Genetics: mutations in a number of difference genes have been implicated in migraines. These genetic changes tend to lead to channelopathies that make the neurovascular system hyperexcitable
</style>
Exacerbating Factors
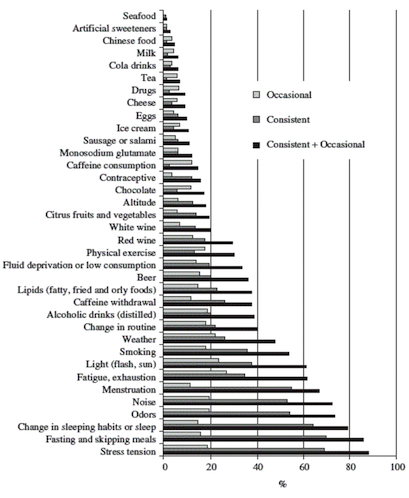
Figure 2: Exacerbating factors (Source: Camboim Rockett, F. et al., 2012)
</style>
<style justify>
- Certain foods or lack of: Salty foods, aged cheese, processed foods, sweeteners such as aspartame and preservative such as monosodium glutamate can result in migraines. Fasting for an extended period of time can also result in migraine attacks.
- Stress
- Drinks: Alcohol especially wine, and excessively caffeinated beverages
- Changes in sleep pattern: Jet lag, missing sleep or getting too much sleep can trigger migraines.
- Changes in temperature and/or air pressure: Changes in weather and air pressure
- Physical activity: Intense physical activity
- Medications: Oral contraceptives and vasodilators such as nitroglycerin
</style>
Prognosis
<style justify> Prognosis is extremely variable among migraine patients. They usually do not lead to further illness but can force sufferers out of work and lead to lost productivity, however migraines can either resolve completely or get progressively worse in select cases (Bigal, 2008) More recent research has found that migraines with aura may increase one’s risk for ischemic stroke and cervical artery dissection, though research is very premature and inconclusive (Schurks, 2009). Overall, migraines aren’t believed to increase risk of death due to heart disease or stroke (Weinberger, 2007). Migraine sufferers were found to have higher than average numbers of white matter brain lesions, though the significance of this finding is unknown (Hougaard, 2014).
</style>
Phases and Symptoms
<style justify> Signs and symptoms of migraines can vary from one individual to another. The symptoms are represented in four different phases:
The Prodrome Phase: This is the phase that occurs from a few days to a few hours before a headache. The prodromal phase occurs to about 60% of migraine patients. Its symptoms include a wide variety of phenomena including change in mood and behaviour, irritability, depression, change in appetite and craving for certain food, and changes in fluid balance in the body. (Blau, J. N., 1980)
The Aura: The phase that occurs right before a headache. The aura is a neurological phenomenon that usually lasts less between 30 to 60 minutes. 13-18% of migraine patients experience aura in every single migraine they have, and 13 -18% of migraine patients experience aura in some of the migraines they have. Symptoms can be visual or sensory. The visual symptoms occur in 99% of the aura cases and include vision disturbance with partial alteration in the field of vision. The sensory symptoms occur in 30-40% of aura cases, and include pain, numbness, and tingling feeling in the hand and arm of one side, and the nose and mouth on the same side. (Hansen, J. M. et al, 2012)
The Pain: Also known as the attack, and is the headache phase. During the pain phase most people experience unilateral headache, with some people experience bilateral headache. The headache comes with different intensities and usually get more intense during physical activity. The pain lasts between 4 and 72 hours for adults and can be less than 4 hours for children. The headache is also usually associated with neck pain. (Jes Olesen, 2006)
The Postdrome: The final phase, which occurs after the migraine attack. During the postdromal phase one experiences soreness in the same area of the migraine. Some patients also experience cognitive difficulties, mood changes, and weakness. (Kelman L., 2006)
</style>
Pathophysiology
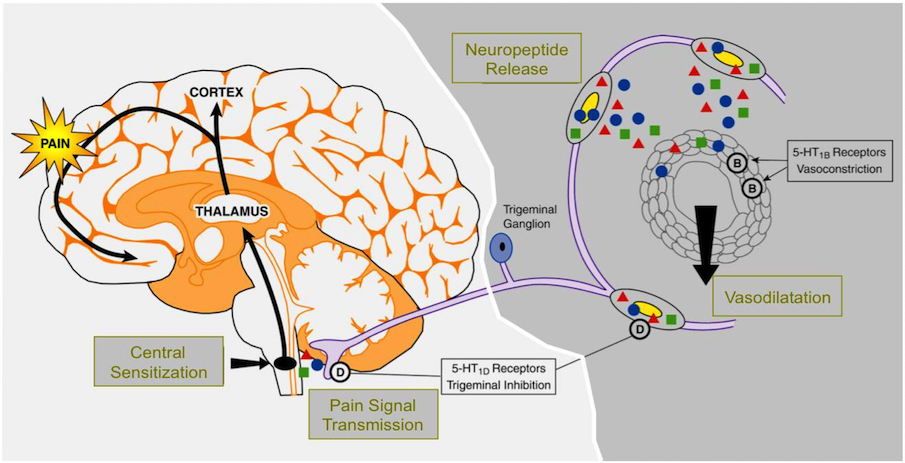
Figure 3: The Pathophysiology of Migraine
</style>
<style justify> The pathophysiology of migraine is fairly well understood, and evidence supports contributory roles of both neural and vascular mechanisms. It is a multifactorial disease whose progression is a result of the interaction of genes and environment. Researchers have identified a linkage to chromosome 19 and the biological basis for this is mutations involving the Cav2.1 (P/Q) type voltage-gated calcium channel CACNA1A gene. Now known as FHM-I, this mutation is responsible for about 50% of the identified families with familial hemiplegic migraine. One consequence of this mutation may be enhanced glutamate release. Researchers also indicate the possibility of a deficiency in serotonin levels however, the mechanism behind this is not well understood. Migraine genes give individuals a predisposition for developing migraine headaches but other factors like stress, food triggers, environmental triggers, hormonal changes or sleep disturbances are necessary triggers. The manifestation of headache in migraineurs is due to the activation of the trigeminovascular system, which is the major pain signaling system in the brain, followed by the release of vasodilatory neuropeptides. Changes in circulating levels of the neurotransmitter serotonin (5-HT) are characteristic of migraine and may contribute to the pathogenesis of the disorder. Recent progress in understanding the pathophysiology of migraine includes the identification of the physiologic roles of vasoactive neuropeptides associated with migraine and the characterization of 5-HT receptor subtypes.
It is thought that the migraine begins with this reversible, transient cortical event known as cortical spreading depression (CSD). It is a slow moving wave of depolarization that starts in the occipital lobe and moves forward and is followed by a prolonged inhibition of cortical activity. First identified by Leão in the rabbit, this distinctive electrophysiological phenomenon has been correlated with the visual aura that precedes the onset of headache in migraine. Although it is not clear how CSD begins in the human brain, genetic factors are likely to play a role in individual CSD susceptibility. The current understanding of the genetic factors underlying migraine and CSD comes from studies of rare monogenic mutations in patients diagnosed with the common form of familial hemiplegic migraine (FHM). In agreement with the human data, mice carrying FHM mutations have shown increased susceptibility to CSD and altered synaptic transmission. That cortical excitability is also evident in psychophysical and neurophysiological studies that demonstrate abnormal processing of sensory information even between attacks. Such altered excitability may also contribute to typical migraine with aura, as suggested by a genetic mutation in a two-pore domain potassium channels that regulate neuronal resting potential and excitability. Together, these findings support the notion that neuronal excitability plays a pivotal role in the predisposition to develop a migraine.
This cortical spreading depression is what initiates the activation of the trigeminovascular system. It begins through antidromic activation at distal trigeminal nerve terminals, which release neurotransmitters including substance P, neurokinin A and calcitonin gene related peptide (CGRP). Calcitonin gene-related peptide is the most potent vasodilator neurotransmitter of the trigeminal system. Substance P, a nondecapeptide involved in nociceptive transmission has vasodilatory effects on the cerebrum. Neurokinin A is a decapeptide with a profile of action and localization in the trigeminal system that is similar to that of substance P but with less potent vasodilatory effects and longer-lasting effects on blood vessel permeability. The critical neuropeptide in the generation of migraine seems to be CGRP rather than substance P or neurokinin A. These substances then bind to receptors on intracranial blood vessels and cause vasodilation, plasma protein extravasation and ultimately sterile inflammation. This results in the reactivation of the trigeminal nerve but now in an orthodromic fashion. The signal is relayed to the trigeminal nucleus caudalis which is a central structure in the brain stem that forwards pain impulses to the thalamus and ultimately the sensory cortex. This atypical, stimulus induced activation of the brain stem during and between migraine attacks, leads to the lack of normal habituation to repetitive stimuli and ultimately sensitization. Sensitization is the idea that repeated administration of a stimulus results in progressive amplification of a response. Once the first order trigeminal neurons become sensitized, normally innocuous, intracranial stimuli, such as a pulsating artery, become painful and result in a throbbing pain made worse with activity. If the pain is unsuccessfully treated, second order and third order neurons extending through the midbrain, thalamus and cortex are continuously activated. This can ultimately lead to central sensitization caused by pain from stimuli that are normally not painful.
</style>
Treatment
To date, there is no actual cure for migraine sufferers. Ideally, acute treatment of migraine should work rapidly, with few side effects, be cost effective and get the patient functional as soon as possible. Drug therapeutics that do exist are primarily targeted around symptom relief during and after the migraine attack. [12]
Ergotamines: It was first isolated by Arthur Stole in 1918 and first used as a treatment option for migraines in 1925. Its chemical structure is similar to that of amines, serotonin, norepinephrine and dopamine. The mode of action of ergotamine in migraine may be by means of selective arterial vasoconstriction on certain cranial vessel beds or, alternatively, by depression of central serotonergic neurons mediating pain transmission or circulatory regulation. They have a complex mode of action that involves interaction with a variety of receptors which include 5-HT, dopamine and noradrenaline.
2 modes of action related to migraine: 1.Activation of 5-HT1B receptors located on intracranial blood vessels, leads to vasoconstriction of blood vessels 2.Activation of 5-HT1D receptors on sensory nerve endings of trigeminal system, inhibits pro-inflammatory neuropeptide release
Oral absorption of ergotamine is about 60-70% and the concurrent administration of caffeine improves both the rate and extent of absorption. Due to high first-pass metabolism, ergotamine has a very low bioavailability from oral administration. Ergotamine and ergotamine-caffeine combination pills still play a role in the acute treatment of migraine in those patients who do not respond adequately to triptan therapy. Ergotamine has more side effects (nausea, vomiting, peripheral and coronary vasoconstriction) due to its relatively nonselective adherence to serotonin, dopamine and adrenergic receptors.
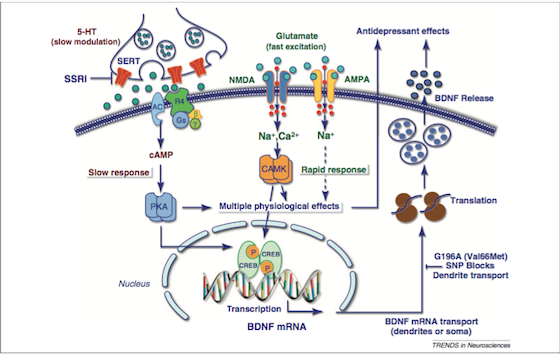
SSRIs: As the name suggests, these drugs prevent the reuptake of serotonin. They do this by inhibiting a monoamine transporter protein, SERT [Figure 3], that transports serotonin from the synaptic cleft to the presynaptic neuron. The SSRIs block the reuptake of serotonin, leading to increased concentrations of the neurotransmitter in the synaptic cleft [Figure 3] and, ultimately, to greater postsynaptic neuronal activity. SSRIs are actually a “successor” to SNRIs, as they are “selective” to serotonin, and usually do not affect other hormones in the nervous system. They are by far the most common drugs prescribed. Some examples of SSRIs include: Fluoxetine (Prozac), sertraline (Zoloft), and citalopram (Celexa). Side effects include: Sexual Dysfunction, Sleep Disorders, and headaches if treatment is suddenly stopped [13].
<html>
Figure 3: Signalling pathways and the treatment of depression (Source: Duman & Voleti, 2012)
</style>
<style justify> SNRIs: Like SSRIs, SNRIs prevent the reuptake of serotonin by inhibiting the activity of neurotransmitters. Unlike SSRIs, SNRIs also prevent the reuptake of the neurotransmitter Norepinephrine. These can be thought of as the less refined predecessor to SSRIs. Another class of antidepressants, known as tricyclic antidepressant (TCAs), also act in the same way as SNRIs. [13]
Psychotherapy: In the clinic, psychotherapy is often used as an alternative or in conjunction to pharmacological treatment. The main forms of psychotherapy used are cognitive behavioural therapy (CBT) and Interpersonal psychotherapy (IPT).
Cognitive Behavioural Therapy (CBT): CBT is founded on the principle that initial thoughts and perspectives are the root of associated behaviour. In CBT, the psychotherapist and patient work together to determine the patterns and markers of detrimental thought patterns. The focus on thought patterns allow it to be used to deal with the feelings of worthlessness in depression.[9]
Interpersonal psychotherapy (IPT): IPT is based on the principle that depressive symptoms are influenced by the relationships the patient holds with other people. The therapy acts to identify and analyze how disruptions in a patient’s relationship with another party plays a role in their behaviour. For example, the challenges of pregnancy often put a strain on the relationship between the new mother and the relationship with her spouse. The economic and personal challenges of having a child may affect the relationship between the new parents, and lead to depressive symptoms in the mother (or even father). Interpersonal therapy analyses relationships from the perspectives of
attachment, communication, and social importance. [9]
</style>
Conclusion
Overall, depression is a heterogenous, burdensome disorder that exhibits a highly variable course, an inconsistent response to treatment and an incomplete understanding of the underlying neurobiology. Its onset is gradual and it can manifest itself not only in psychological symptoms but physical symptoms as well. Future initiatives are focusing on novel treatments that can start to take effect quicker than the 4-5 weeks required for antidepressants. Research is beginning to look at the use of theta-burst stimulation which involves delivering magnetic pulses to the brain. It is a fast acting, simple, non invasive form of treatment. These magnetic pulses stimulate electric current in the brain and the hope is that repeated treatment can capitalize on the brain's neuroplasticity by changing the way in which the brain's neurons fire. However, this is a very new field and much more research needs to be done surrounding the efficacy and safety of this treatment.