Table of Contents
Migraines
final_copy-migraine_headaches-_group_2_presentation_2_life_sci_4m03.pptx
<style justify> A migraine is a debilitating, recurring, primary headache disorder. Genetic mutations in the CACNA1A gene, coding for voltage-gated calcium channels, have been implicated in about half the cases of familial hemiplegic migraine (FHM). The onset of migraines can be due to the hyperexcitability of trigeminal neurons and the abnormal integration of sensory information. Consequently, the individual may experience symptoms such as nausea, change in appetite, decreased cognitive ability, visual disturbances and lightheadedness. These symptoms may last anywhere from 4-72 hours. While there is no cure for migraines, there are drug therapeutics targeted at pain relief and prevention. New therapies related to neurostimulation are emerging but more research needs to be done. Overall, migraine is underdiagnosed and undertreated and improvements from the clinical end are needed.
</style>
History
<style justify> Migraines are one of the oldest documented illness being described as early as 1200 BCE by the Egyptians. Arataeus of Cappadocia is however the one credited with the discovery of migraines after having extensively described unilateral headaches with aura. Migraines have plagued humans throughout our history with little progress made in the area of treatment and cures. Several treatments have been tried with no avail, including hot irons, bloodletting, inserting garlic into incisions made in the temple and applying opium and vinegar solutions directly to the skull. Some have even gone as far as to perform surgeries such as lobotomies on migraine sufferers. Trepanation involves making a hole in the skull to let out evil spirits that presumably were causing the migraine. It is possibly the oldest surgery in history and may date as far back as 6500 BCE. The first known use of medication that has shown some success is use of ergotamine in the 1930s. Ergotamine constricts blood vessels in the brain and has been shown to provide pain relief in some individuals. Many drugs have been researched and experimented with since with little success. The first and currently only class of drugs developed and used solely for the treatment of migraines are Triptans, which were developed in the early 1990s (American Migraine Foundation, 2016).
</style>
Epidemiology
<style justify> Migraines are more common in males before puberty and in females after puberty with 19% of adult women and 11% of adult males being affected (Vos, 2010). Migraines commonly begin between the ages of 15 and 24 and have an increased incidence in adults aged 35 to 45 (Bartleson, 2010). The incidence of migraines are slightly lower in Asian and African countries, but this may be partially due to lack of diagnostic resources in these areas (Wang, 2003). In the United States, 18% of men and 43% of women will experience migraines at some point in their lives with about 6% of men and 18% of women experiencing migraines in a given year. Europeans have a lifetime risk of migraine between 12 and 28%. Chronic migraines occur in about 1.4 to 2.2% of the population. Worldwide, migraines affect about 15% of the population (Vos, 2010).
</style>
Figure 1: Prevalence of migraines in Canada by age group and sex
Risk Factors
<style justify> There are several factors that make one more prone to getting migraines.
Family History: Upto 90% of people who suffer from migraines have family members who have had the same condition. If one or both of your parents have migraines, then there is a good chance that you would suffer from migraine attacks (Mayo Clinic, 2013).
Age: One can develop migraines at any age, but most people who suffer from migraine attacks get their first attack during adolescence. By age 40, most people who suffer from migraines would got their first migraine attack (Mayo Clinic, 2013).
Sex: Women are 3 times more likely to suffer from migraine attacks than men. Boys tend to get more headaches than girls during childhood, but during and after puberty, girls suffer from migraines overwhelmingly more than boys (Mayo Clinic, 2013).
Hormonal changes: Women are more susceptible to migraines during the onset or immediately after menstruation (Mayo Clinic, 2013).
Genetics: mutations in a number of difference genes have been implicated in migraines. These genetic changes tend to lead to channelopathies that make the neurovascular system hyperexcitable (Mayo Clinic, 2013).
</style>
Exacerbating Factors
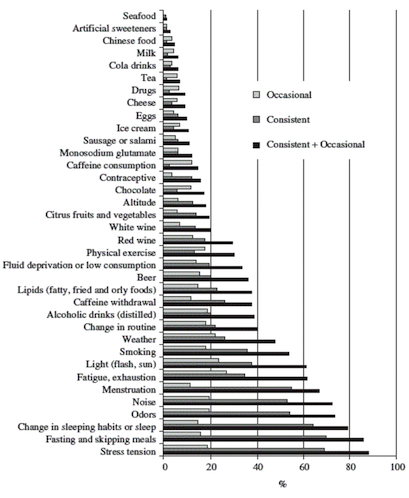
Figure 2: Exacerbating factors (Source: Camboim Rockett, F. et al., 2012)
</style>
<style justify>
- Certain foods or lack of: Salty foods, aged cheese, processed foods, sweeteners such as aspartame and preservative such as monosodium glutamate can result in migraines. Fasting for an extended period of time can also result in migraine attacks.
- Stress
- Drinks: Alcohol especially wine, and excessively caffeinated beverages
- Changes in sleep pattern: Jet lag, missing sleep or getting too much sleep can trigger migraines.
- Changes in temperature and/or air pressure: Changes in weather and air pressure
- Physical activity: Intense physical activity
- Medications: Oral contraceptives and vasodilators such as nitroglycerin
</style>
Prognosis
<style justify> Prognosis is extremely variable among migraine patients. They usually do not lead to further illness but can force sufferers out of work and lead to lost productivity, however migraines can either resolve completely or get progressively worse in select cases (Bigal, 2008) More recent research has found that migraines with aura may increase one’s risk for ischemic stroke and cervical artery dissection, though research is very premature and inconclusive (Schurks, 2009). Overall, migraines aren’t believed to increase risk of death due to heart disease or stroke (Weinberger, 2007). Migraine sufferers were found to have higher than average numbers of white matter brain lesions, though the significance of this finding is unknown (Hougaard, 2014).
</style>
Phases and Symptoms
<style justify> Signs and symptoms of migraines can vary from one individual to another. The symptoms are represented in four different phases:
The Prodrome Phase: This is the phase that occurs from a few days to a few hours before a headache. The prodromal phase occurs to about 60% of migraine patients. Its symptoms include a wide variety of phenomena including change in mood and behaviour, irritability, depression, change in appetite and craving for certain food, and changes in fluid balance in the body. (Blau, J. N., 1980)
The Aura: The phase that occurs right before a headache. The aura is a neurological phenomenon that usually lasts less between 30 to 60 minutes. 13-18% of migraine patients experience aura in every single migraine they have, and 13 -18% of migraine patients experience aura in some of the migraines they have. Symptoms can be visual or sensory. The visual symptoms occur in 99% of the aura cases and include vision disturbance with partial alteration in the field of vision. The sensory symptoms occur in 30-40% of aura cases, and include pain, numbness, and tingling feeling in the hand and arm of one side, and the nose and mouth on the same side. (Hansen, J. M. et al, 2012)
The Pain: Also known as the attack, and is the headache phase. During the pain phase most people experience unilateral headache, with some people experience bilateral headache. The headache comes with different intensities and usually get more intense during physical activity. The pain lasts between 4 and 72 hours for adults and can be less than 4 hours for children. The headache is also usually associated with neck pain. (Jes Olesen, 2006)
The Postdrome: The final phase, which occurs after the migraine attack. During the postdromal phase one experiences soreness in the same area of the migraine. Some patients also experience cognitive difficulties, mood changes, and weakness. (Kelman L., 2006)
</style>
Pathophysiology
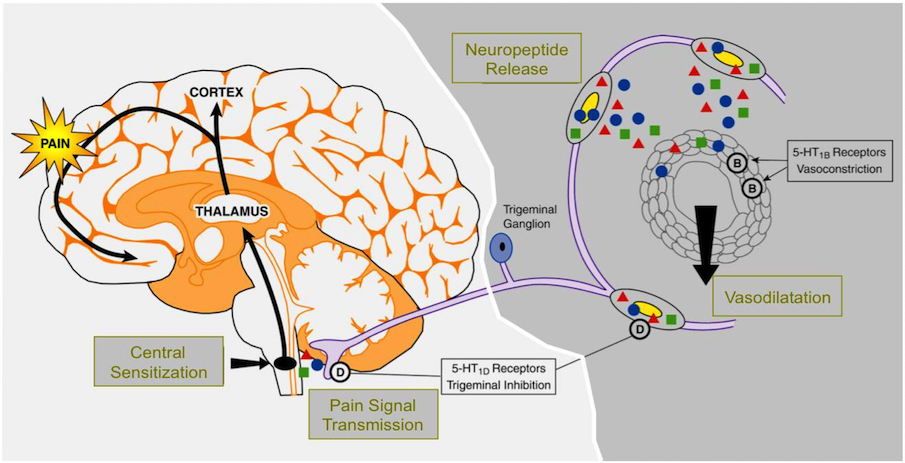
Figure 3: The Pathophysiology of Migraine
</style>
<style justify> The pathophysiology of migraine is fairly well understood, and evidence supports contributory roles of both neural and vascular mechanisms. It is a multifactorial disease whose progression is a result of the interaction of genes and environment. Researchers have identified a linkage to chromosome 19 and the biological basis for this is mutations involving the Cav2.1 (P/Q) type voltage-gated calcium channel CACNA1A gene (Noseda & Burstein, 2013). Now known as FHM-I, this mutation is responsible for about 50% of the identified families with familial hemiplegic migraine (Noseda & Burstein, 2013). One consequence of this mutation may be enhanced glutamate release. Researchers also indicate the possibility of a deficiency in serotonin levels however, the mechanism behind this is not well understood. Migraine genes give individuals a predisposition for developing migraine headaches but other factors like stress, food triggers, environmental triggers, hormonal changes or sleep disturbances are necessary triggers. The manifestation of headache in migraineurs is due to the activation of the trigeminovascular system, which is the major pain signaling system in the brain, followed by the release of vasodilatory neuropeptides (Noseda & Burstein, 2013). Changes in circulating levels of the neurotransmitter serotonin (5-HT) are characteristic of migraine and may contribute to the pathogenesis of the disorder. Recent progress in understanding the pathophysiology of migraine includes the identification of the physiologic roles of vasoactive neuropeptides associated with migraine and the characterization of 5-HT receptor subtypes.
It is thought that the migraine begins with this reversible, transient cortical event known as cortical spreading depression (CSD). It is a slow moving wave of depolarization that starts in the occipital lobe and moves forward and is followed by a prolonged inhibition of cortical activity (Noseda & Burstein, 2013). First identified by Leão in the rabbit, this distinctive electrophysiological phenomenon has been correlated with the visual aura that precedes the onset of headache in migraine (Noseda & Burstein, 2013). Although it is not clear how CSD begins in the human brain, genetic factors are likely to play a role in individual CSD susceptibility. The current understanding of the genetic factors underlying migraine and CSD comes from studies of rare monogenic mutations in patients diagnosed with the common form of familial hemiplegic migraine (FHM). In agreement with the human data, mice carrying FHM mutations have shown increased susceptibility to CSD and altered synaptic transmission (Noseda & Burstein, 2013). That cortical excitability is also evident in psychophysical and neurophysiological studies that demonstrate abnormal processing of sensory information even between attacks. Such altered excitability may also contribute to typical migraine with aura, as suggested by a genetic mutation in a two-pore domain potassium channels that regulate neuronal resting potential and excitability (Noseda & Burstein, 2013). Together, these findings support the notion that neuronal excitability plays a pivotal role in the predisposition to develop a migraine.
This cortical spreading depression is what initiates the activation of the trigeminovascular system. It begins through antidromic activation at distal trigeminal nerve terminals, which release neurotransmitters including substance P, neurokinin A and calcitonin gene related peptide (CGRP (Noseda & Burstein, 2013)). Calcitonin gene-related peptide is the most potent vasodilator neurotransmitter of the trigeminal system. Substance P, a nondecapeptide involved in nociceptive transmission has vasodilatory effects on the cerebrum (Noseda & Burstein, 2013). Neurokinin A is a decapeptide with a profile of action and localization in the trigeminal system that is similar to that of substance P but with less potent vasodilatory effects and longer lasting effects on blood vessel permeability (Noseda & Burstein, 2013). The critical neuropeptide in the generation of migraine seems to be CGRP rather than substance P or neurokinin A. These substances then bind to receptors on intracranial blood vessels and cause vasodilation, plasma protein extravasation and ultimately sterile inflammation (Noseda & Burstein, 2013). This results in the reactivation of the trigeminal nerve but now in an orthodromic fashion. The signal is relayed to the trigeminal nucleus caudalis which is a central structure in the brain stem that forwards pain impulses to the thalamus and ultimately the sensory cortex (Noseda & Burstein, 2013). This atypical, stimulus induced activation of the brain stem during and between migraine attacks, leads to the lack of normal habituation to repetitive stimuli and ultimately sensitization. Sensitization is the idea that repeated administration of a stimulus results in progressive amplification of a response (Noseda & Burstein, 2013). Once the first order trigeminal neurons become sensitized, normally innocuous, intracranial stimuli, such as a pulsating artery, become painful and result in a throbbing pain made worse with activity. If the pain is unsuccessfully treated, second order and third order neurons extending through the midbrain, thalamus and cortex are continuously activated (Noseda & Burstein, 2013). This can ultimately lead to central sensitization caused by pain from stimuli that are normally not painful.
</style>
Treatment
To date, there is no actual cure for migraine sufferers. Ideally, acute treatment of migraine should work rapidly, with few side effects, be cost effective and get the patient functional as soon as possible. Drug therapeutics that do exist are primarily targeted around symptom relief during and after the migraine attack. Acute treatment can be divided into migraine specific and nonspecific therapy.
Ergotamines:
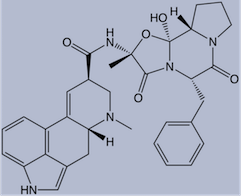
Figure 4: Chemical structure of ergotamine
</style>
<style justify> It was first isolated by Arthur Stole in 1918 and first used as a treatment option for migraines in 1925 (Kalra & Elliott, 2007). Its chemical structure is similar to that of amines, serotonin, norepinephrine and dopamine. The mode of action of ergotamine in migraine may be by means of selective arterial vasoconstriction on certain cranial vessel beds or, alternatively, by depression of central serotonergic neurons mediating pain transmission or circulatory regulation (Kalra & Elliott, 2007). They have a complex mode of action that involves interaction with a variety of receptors which include 5-HT, dopamine and noradrenaline.
2 modes of action related to migraine:
1.Activation of 5-HT1B receptors located on intracranial blood vessels, leads to vasoconstriction of blood vessels (Kalra & Elliott, 2007).
2.Activation of 5-HT1D receptors on sensory nerve endings of trigeminal system, inhibits pro-inflammatory neuropeptide release (Kalra & Elliott, 2007).
Oral absorption of ergotamine is about 60-70% and the concurrent administration of caffeine improves both the rate and extent of absorption (Tfelt-hansen et al, 2000). Due to high first-pass metabolism, ergotamine has a very low bioavailability from oral administration (Tfelt-hansen et al, 2000). Ergotamine and ergotamine-caffeine combination pills still play a role in the acute treatment of migraine in those patients who do not respond adequately to triptan therapy. Ergotamine has more side effects (nausea, vomiting, peripheral and coronary vasoconstriction) due to its relatively nonselective adherence to serotonin, dopamine and adrenergic receptors (Tfelt-hansen et al, 2000). </style>
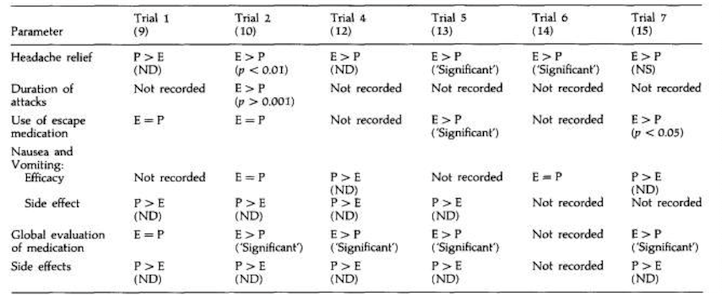
Figure 5: Placebo controlled clinical trial with ergotamine
</style>
<style justify>
The study conducted by Dahlof, 1993 looked at the effect of ergotamines on headache relief in people presenting with symptoms of migraines. In comparison to the placebo treatment, ergotamines were found to be more effective in the relief of headache in 5 out of the 6 trials. In three of the trials, there was a statistically significant difference. The combination of ergotamine and caffeine was used in three of the studies (12,13,15). Caffeine was included to improve absorption and efficacy. In the other trial, ergotamine was given together with caffeine, belladonna alkaloids and a barbiturate (11).This combination of drugs is significantly more effective than ergotamine alone in relieving migraine headache and other symptoms (12).
Nausea and vomiting: All ergotamine trials evaluated had some analysis of nausea and/or vomiting. In the four trials where efficacy assessments were made, nausea and/or vomiting either increased in severity after treatment with ergotamine, and more patients were affected than was observed with placebo or there was little difference between the two treatments (10, 12, 14, 15). In all trials where the symptoms were assessed as side effects, more patients were affected following ergotamine than following placebo (9, 10, 12, 13) (Dahlof, 1993).
Global evaluation of medication: Five of the ergotamine trials evaluated presented results for patients’ preference for ergotamine or placebo. In four trials, significantly more patients preferred ergotamine to placebo (10, 12, 13, 15). In the fifth trial, similar numbers of patients clinically diagnosed as having migraine preferred placebo to ergotamine as preferred ergotamine to placebo (13) (Dahlof, 1993).
Side effects : The side effect profile of ergotamine and placebo was reported in five of the six trials evaluated (9, 10, 12, 13, 15). In all these trials more patients reported side effects with ergotamine than with placebo. Side effects associated with ergotamine included nausea/ vomiting, dizziness/vertigo, drowsiness/tiredness, numbness, nervousness, trembling, dyspnoea and dry mouth (Dahlof, 1993). </style>
Triptans
<style justify> Triptans like Sumatriptan were developed to treat migraines in the early 1990s. They effectively relieve pain and nausea in approximately 75% of people. Triptans are often reserved for use in those with moderate to severe pain and for those who do not respond to analgesics (Johnston, 2010). They are administered as oral tablets, injections, nasal sprays and pills. Side effects include tingling, pain and tightness in the chest or throat, vomiting, dry mouth, flushing, dizziness and fatigue. In rare cases they can lead to cardiac ischemia (Gilmore, 2011). Triptans act in a similar manner as the ergotamines but are more selective and therefore have less side effects. Triptans are selective 5-hydroxytryptamine (5-HT) receptor agonists with high affinity for 5-HT1B and 5-HT1D receptors. These receptors when activated, constrict blood vessels in the brain to provide relief (Bartleson, 2010). Triptans are often avoided in patients who have cardiovascular disease, a history of stroke or have migraines accompanied by neurological problems. Patients should be evaluated for their risk of developing vascular disease before prescription for triptans is given. Triptans are not addictive but when used frequently, such as 10 or more days per month, medication overuse headaches can result. </style>
Cardiovascular medications in the treatment of migraine
Researchers do not yet understand how exactly beta blockers prevent migraines. They are traditionally used for cardiology patients to prevent the stimulation of adrenergic receptors responsible for increased cardiac action. For treating migraines it is thought that they act through beta1 adrenoreceptor inhibition of the activation of third order trigeminovascular nociceptive neurons. The beta blockers propranolol (Inderal La, Innopran XL, others), metoprolol tartrate (Lopressor) and timolol (Betimol) have proved effective for preventing migraines. You may not notice improvement in symptoms for several weeks after taking these medications. However, the usage of beta blockers are not advised if you are over 60, have heart or blood vessel conditions or use tobacco.
Another class of cardiovascular medications (calcium channel blockers) used to treat high blood pressure and keep blood vessels from becoming narrow or wide, also may be helpful in preventing migraines and relieving symptoms of an attack. The use of calcium channel blockers comes from the idea that migraine may be due to a mutation in calcium channels that make them hyperexcitable and as such this medication can help to counteract this effect. Verapamil (Calan, Verelan, others) is a calcium channel blocker that may help you.
Analgesics
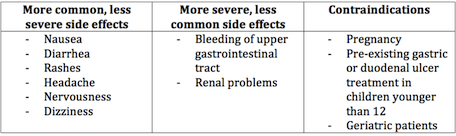
<style justify> Most first line treatments for migraines are analgesics. Generally, these treatments are used as a primary option in severe cases, and are used when the symptoms of a migraine have just manifested themselves, as to prevent further progression. Analgesics are classified as a non-specific treatment when used in the treatment of migraines, as they are used in the treatment of other conditions as well (Pfaffenrath, 1995). As such, they are often used in combination with migraine specific therapies. Common analgesics for migraines are usually a class of drug known as Non-steroidal Anti-inflammatory Drugs (NSAIDS) such as Aspirin and Aleve. NSAIDS are generally used for moderate to severe migraines and are the final non specific treatment for migraines, as they treat the symptoms of migraines, rather than the underlying cause (Pfaffenrath, 1995). </style>
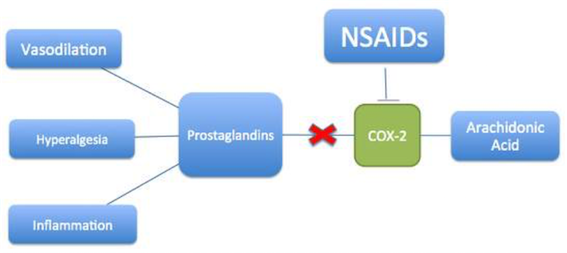
Figure 6: Mechanism of action of NSAIDs
</style>
<style justify> NSAIDs work by inhibiting the production of prostaglandins, which are the chemical messengers that initiate the pain and inflammation response (Whalen, K., 2012). Tissue in the human body produces prostaglandins in response to damage, and prostaglandins increase sensitivity in the nerves that send the pain response to the brain, thus establishing the pain threshold (Whalen, K., 2012). The mechanism by which NSAIDs prevent prostaglandin synthesis is by the inhibition of the cyclooxygenase (COX) enzymes that are found in their metabolic pathway [Figure 6] (European Neurological Review, 2011). There are two classes of COX enzymes, and most traditional NSAIDs that are used to treat migraines inhibit both COX-1 and COX-2. COX-1 is constitutive, while COX-2 is induced by injury (European Neurological Review, 2011). The reduction of prostaglandins inhibits pain signaling to the brain, ergo aiding in migraine management. </style>
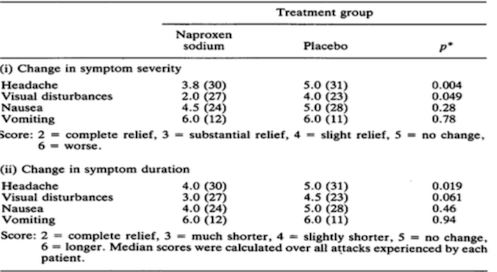
Figure 7: Effectiveness of NSAIDs in treatment of symptoms (Johnson et. al, 1985)
</style>
<style justify> Effectiveness of NSAIDs in the treatment of symptoms: Seventy patients with classical or common migraine were treated during their attacks with either naproxen sodium or placebo in a randomised, double-blind parallel group study (Johnson et. al, 1985). The initial dose of naproxen sodium was 825 mg followed one hour later by a further 550 mg, if symptoms were the same or had improved (Johnson et. al, 1985). Patients were seen at admission and then at monthly intervals until a total of ten attacks had been studied. During each attack the patient graded the severity of headache, visual disturbance, nausea and other important symptoms (specific to the patient) as none, mild, moderate or severe. In Figure 7, Naproxen sodium produced statistically significantly superior relief of headache in comparison with placebo (p= 0.004) and the duration of headache was significantly shorter in this group than in the placebo group (p= 0.019) (Johnson et. al, 1985). Patients in the naproxen sodium group also had a significant reduction in the severity of visual disturbances when compared with those in the placebo group (= 0.049). The differences detected between the groups with respect to the severity of nausea and vomiting and the duration of the visual disturbances, nausea and vomiting were not significant, but the score for the naproxen sodium group was numerically lower for the severity of nausea and for the duration of both visual disturbances and nausea (Johnson et. al, 1985). Scores for the severity and duration of vomiting were the same for both groups. In summary, naproxen sodium has proved to be a drug effective in relieving symptoms associated with common migraine when taken at the onset of an attack. </style>
Calcitonin gene related peptide antagonists
Currently CGRP1 antagonists hold promise as new anti-migraine drugs. Two recently introduced are: BIBN4096BS and Compound 1 (Kalra & Elliott, 2007). BIBN4096BS was tested in the trigeminal ganglion and found to inhibit vasodilatation (Kalra & Elliott, 2007). Other experiments support its possible role as an anti-nociceptor mediator in migraine. Compound 1 has similar properties but is less potent than BIBN4096BS in human tissues (Kalra & Elliott, 2007). A third smaller CGRP antagonistic molecule is SB-273779. It has similar properties as the other two but may have greater value for the study of migraine and CGRP activity in animal models (Kalra & Elliott, 2007). The efficacy of BIBN4096BS has been tested in humans in two studies published in 2004. In the first, the safety, tolerability and pharmacokinetics of BIBN4096BS were tested in healthy volunteers. After a single IV administration of gradually increasing dose, most of the adverse events occurred at the highest administered dose (10 mg) and were relatively mild and transient (Iovino et al 2004). In another controlled study, moderate or severe headache was treated with 2.5 mg of BIBN4096BS IV vs. placebo. The end-point of pain reduction within 2 hours to mild or no pain was achieved in 66% of BIBN4096BS treated patients vs. 27% of the placebo group (Doggrell 2004). In clinical practice, its potential use will be limited to settings appropriate for IV administration.
Surgery and Devices
Surgery
<style justify> Recently Plastic surgeons have advertised nerve decompression surgery as an innovative new treatment of migraine headaches. In the 1990s, the use of the muscle relaxant Botulinum toxin became popular in the treatment of chronic migraine. Its effect was thought to occur through paralysis of muscles surrounding nerves in areas of pain. This operation involves the removal of a muscle in an area of the forehead where patients experience migraine pain. The idea for surgery began with patients reporting that their headaches were disappearing after forehead rejuvenation plastic surgery (Migraine surgery Centre London, 2016). Combined, these observations led to a theory that migraine headache pain can be triggered by compression of superficial nerves by surrounding tissues, such as muscle, fascia, and bone. During nerve-decompression migraine surgery, nerves at one or multiple common migraine headache trigger sites are released from surrounding structures such as bone, muscle, fascia, and vessels (Migraine surgery Centre London, 2016). The Surgical Migraine Procedure is the removal of the corrugator muscles (small muscles associated with the eyebrows) (Migraine surgery Centre London, 2016). However, the efficacy of this method beyond placebo has been debated in the medical community. </style>
Devices
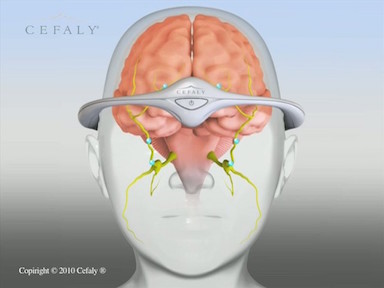
<style justify> Neurostimulation is the practice of applying gentle stimulation to nerves that have been identified as sending strong, frequent pain signals.
The Cefaly is a headband designed to deliver electrical impulses to nerves that transmit migraine pain and thereby theoretically suppress this trigger mechanism. To reduce the frequency of headaches, it is to be worn for 20 minutes every day (Didier et. al, 2015). The device consists of a battery-operated electrical pulse generator and a self-adhesive electrode (Didier et. al, 2015). The patient applies the electrode to the middle of the forehead and lowers a headband containing the electrical pulse generator over the forehead to engage a pin located on the electrode. Pressing a button on the band generates a pulsed electric current that stimulates the upper branches of the trigeminal nerve, producing a tingling or massaging sensation (Didier et. al, 2015). During the treatment, which has a fixed duration of 20 minutes, the intensity of the electric current gradually increases. </style>
http://www.cefaly.ca/#howitworks
https://www.youtube.com/watch?v=S_p0WlJd_dw
Conclusion
Overall, migraines are a heterogenous, burdensome disorder that are debilitating for the individuals experiencing them. There appears to be a strong link between genetics and environment in making individuals susceptible to migraine attacks. Symptoms can vary from one individual to the next and exacerbating factors can have different effects on different individuals. Our proposed course of treatment is to use non-steroidal anti-inflammatory drugs with caffeine administration to alleviate pain in migraine sufferers. Studies have shown that NSAIDs are significantly more effective at relieving symptoms of headache compared to other proposed therapeutics. NSAIDs, like Naproxen, are much more cost-effective, have a longer lasting effect, have a reduced likelihood of producing rebound headaches, show low reports of adverse affects and are non-addictive. It has been shown that co-administration with caffeine promote more effective intestinal absorption and a higher likelihood of a positive treatment response. Great progress has been made in understand migraine pathophysiology as well as defining new specific therapies. In recognition of the large market of migraine sufferers, the pharmaceutical and bioengineering industries are working towards newer and better approaches for affective interventions.
References
American Migraine Foundation. (n.d.). Retrieved February 27, 2016, from http://www.americanmigrainefoundation.org/resources-and-links/a-brief-sad-history-of-treatments-for-migraine/
Aminoff, Roger P. Simon, David A. Greenberg, Michael J. (2009). Clinical neurology (7 ed.). New York, N.Y: Lange Medical Books/McGraw-Hill. pp. 85–88.
Bartleson JD, Cutrer FM (May 2010). “Migraine update. Diagnosis and treatment”. Minn Med 93 (5): 36–41. PMID 20572569.
Bigal, ME; Lipton, RB (June 2008). “The prognosis of migraine”. Current Opinion in Neurology 21 (3): 301–8.doi:10.1097/WCO.0b013e328300c6f5. PMID 18451714.
Blau, J. N. (1980). Migraine prodromes separated from the aura: complete migraine. Br Med J, 281(6241), 658-660.
Dahlof, C. (1993). Placebo-controlled clinical trials with ergotamine in the acute treatment of migraine. Cephalalgia, 13(3), 166-171.
Diseases and Conditions: Migraines. (2013, June 04). Retrieved March 08, 2016, from http://www.mayoclinic.org/diseases-conditions/migraine-headache/basics/risk-factors/con-20026358
Didier HA, Di fiore P, Marchetti C, et al. Electromyography data in chronic migraine patients by using neurostimulation with the Cefaly® device. Neurol Sci. 2015;36 Suppl 1:115-9.
Doggrell SA. 2004. New drugs for the prevention and treatment of migraine: topiramate and BIBN 4096 BS. Expert Opin Pharmacother,5:1837–40.
Hansen, J. M., Lipton, R. B., Dodick, D. W., Silberstein, S. D., Saper, J. R., Aurora, S. K., … & Charles, A. (2012). Migraine headache is present in the aura phase A prospective study. Neurology, 79(20), 2044-2049.
European Neurological Review, 2011;6(4):265–9
Hougaard, A; Amin, FM; Ashina, M. 2014. “Migraine and structural abnormalities in the brain.” Current opinion in neurology 27 (3): 309–14.doi:10.1097/wco.0000000000000086.
Iovino M, Feifel U, Yong C-L, et al. 2004. Safety, tolerability and pharmacokinetics of BIBN4096 BS, the first selective small molecule calcitonin gene-related peptide receptor antagonist, following single intravenous administration in healthy volunteers. Cephalalgia, 24:645–56.
International Headache Society abstracts. Cephalalgia. 2015;35(6 Suppl):1-296.
Jes Olesen, (2006). The headaches. (3 ed.). Philadelphia: Lippincott Williams & Wilkins. p. 238.
Johnson, E.S, Ratcliffe, D.M & Wilkinson, M. (1985). Naproxen sodium in the treatment of migraine . Cephalalgia, 5(1), 5-10.
Johnston MM, Rapoport AM (August 2010). “Triptans for the management of migraine”. Drugs 70 (12): 1505–18. doi:10.2165/11537990-000000000-00000.PMID 20687618.
Kalra, A. & Elliott, D. (2007). Acute migraine: current treatment and emerging therapies . Therapeutics and clinical risk management , 3(3), 449-459.
Kelman L., (2006). “ The postdrome of the acute migraine attack”. Cephalalgia 26 (2): 214–20.
Noseda, R & Burstein, R. (2013). Migraine pathophysiology: Anatomy of the trigeminovascular pathway and associated neurological symptoms, cortical spreading depression, sensitization, and modulation of pain. Pain , 154(1), S44-S53.
Pfaffenrath V, Scherzer S. Analgesics and NSAlDs in the treatment of the acute migraine attack. Cephalalgia 1995; Suppl 15:14-20.
Rizzoli P. Preventive pharmacotherapy in migraine. Headache. 2014;54(2):364-9.
Schürks, M; Rist, PM; Bigal, ME; Buring, JE; Lipton, RB; Kurth, T (2009-10-27). “Migraine and cardiovascular disease: systematic review and meta-analysis”. BMJ (Clinical research ed.) 339: b3914.doi:10.1136/bmj.b3914. PMC 2768778. PMID 19861375.
Tfelt-hansen et al.. (2000). Ergotamine in the acute treatment of migraine: A review and European consensus . Brain, 123(1), 9-18.
Vos, T; Flaxman, AD; Naghavi, M; Lozano, R; Michaud, C; Ezzati, M; Shibuya, K; Salomon, JA; et al. (Dec 15, 2012). “Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010”. Lancet 380 (9859): 2163–96.doi:10.1016/S0140-6736(12)61729-2. PMID 23245607.
Wang SJ (2003). “Epidemiology of migraine and other types of headache in Asia”. Curr Neurol Neurosci Rep3 (2): 104–8. doi:10.1007/s11910-003-0060-7.PMID 12583837.
Weinberger, J (March 2007). “Stroke and migraine”.Current cardiology reports 9 (1): 13–9.doi:10.1007/s11886-007-0004-y. PMID 17362679.
Whalen, K., Finkel, R., & Panavelil, T. A. (n.d.). Pharmacology (6th ed.).