This is an old revision of the document!
Table of Contents
Migraines
<style justify> A migraine is a familial episodic brain disorder characterized by recurrent headaches. Genetic mutations in the CACNA1A gene, coding for voltage-gated calcium channels, have been implicated in about half the cases of familial hemiplegic migraine (FHM). The onset of migraines can be due to the hyperexcitability of trigeminal neurons and the abnormal integration of sensory information. Consequently, the individual may experience symptoms such as nausea, change in appetite, decreased cognitive ability, visual disturbances and lightheadedness. These symptoms may last anywhere from 4-72 hours. While there is no cure for migraines, there are drug therapeutics targeted at pain relief and prevention. Overall, migraine is underdiagnosed and undertreated and improvements from the clinical end are needed.
</style>
History
Migraines are one of the oldest documented illness being described as early as 1200 BCE by the Egyptians. Arataeus of Cappadocia is however the one credited with the discovery of migraines after having extensively described unilateral headaches with aura. Migraines have plagued humans throughout our history with little progress made in the area of treatment and cures. Several treatments have been tried with no avail, including hot irons, bloodletting, inserting garlic into incisions made in the temple and applying opium and vinegar solutions directly to the skull. Some have even gone as far as to perform surgeries such as lobotomies on migraine sufferers. Trepanation involves making a hole in the skull to let out evil spirits that presumably were causing the migraine. It is possibly the oldest surgery in history and may date as far back as 6500 BCE. The first known use of medication that has shown some success is use of ergotamine in the 1930s. Ergotamine constricts blood vessels in the brain and has been shown to provide pain relief in some individuals. Many drugs have been researched and experimented with since with little success. The first and currently only class of drugs developed and used solely for the treatment of migraines are Triptans, which were developed in the early 1990s.
Epidemiology
Migraines are more common in males before puberty and in females after puberty with 19% of adult women and 11% of adult males being affected (Vos, 2010). Migraines commonly begin between the ages of 15 and 24 and have an increased incidence in adults aged 35 to 45 (Bartleson, 2010). The incidence of migraines are slightly lower in Asian and African countries, but this may be partially due to lack of diagnostic resources in these areas (Wang, 2003). In the United States, 18% of men and 43% of women will experience migraines at some point in their lives with about 6% of men and 18% of women experiencing migraines in a given year. Europeans have a lifetime risk of migraine between 12 and 28%. Chronic migraines occur in about 1.4 to 2.2% of the population. Worldwide, migraines affect about 15% of the population (Vos, 2010).
Figure 1: Prevalence of migraines in Canada by age group and sex The above graph illustrates that females are significantly more likely to experience migraines compared to males after the age of 12. Individuals between the ages of 30 to 49 have the highest incidence rate for migraine attacks and act as the reference group to establish statistical significance between other age groups.
Risk Factors
There are several factors that make one more prone to getting migraines.
Family History: Upto 90% of people who suffer from migraines have family members who have had the same condition. If one or both of your parents have migraines, then there is a good chance that you would suffer from migraine attacks.
Age: One can develop migraines at any age, but most people who suffer from migraine attacks get their first attack during adolescence. By age 40, most people who suffer from migraines would got their first migraine attack.
Sex: Women are 3 times more likely to suffer from migraine attacks than men. Boys tend to get more headaches than girls during childhood, but during and after puberty, girls suffer from migraines overwhelmingly more than boys.
Hormonal changes: Women are more susceptible to migraines during the onset or immediately after menstruation.
Genetics: mutations in a number of difference genes have been implicated in migraines. These genetic changes tend to lead to channelopathies that make the neurovascular system hyperexcitable
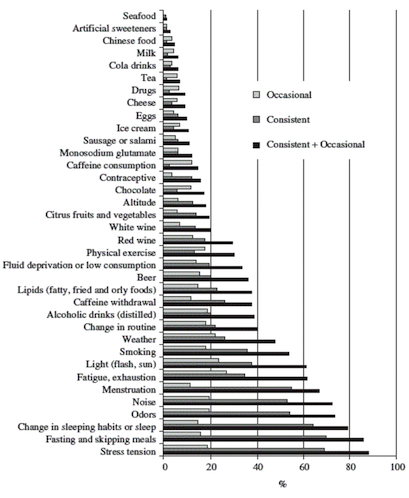
Exacerbating Factors
- Certain foods or lack of: Salty foods, aged cheese, processed foods, sweeteners such as aspartame and preservative such as monosodium glutamate can result in migraines. Fasting for an extended period of time can also result in migraine attacks.
- Stress
- Drinks: Alcohol especially wine, and excessively caffeinated beverages
- Changes in sleep pattern: Jet lag, missing sleep or getting too much sleep can trigger migraines.
- Changes in temperature and/or air pressure: Changes in weather and air pressure
- Physical activity: Intense physical activity
- Medications: Oral contraceptives and vasodilators such as nitroglycerin
Prognosis
Prognosis is extremely variable among migraine patients. They usually do not lead to further illness but can force sufferers out of work and lead to lost productivity, however migraines can either resolve completely or get progressively worse in select cases (Bigal, 2008) More recent research has found that migraines with aura may increase one’s risk for ischemic stroke and cervical artery dissection, though research is very premature and inconclusive (Schurks, 2009). Overall, migraines aren’t believed to increase risk of death due to heart disease or stroke (Weinberger, 2007). Migraine sufferers were found to have higher than average numbers of white matter brain lesions, though the significance of this finding is unknown (Hougaard, 2014).
Phases and Symptoms
Signs and symptoms of migraines can vary from one individual to another. The symptoms are represented in four different phases:
The Prodrome Phase: This is the phase that occurs from a few days to a few hours before a headache. The prodromal phase occurs to about 60% of migraine patients. Its symptoms include a wide variety of phenomena including change in mood and behaviour, irritability, depression, change in appetite and craving for certain food, and changes in fluid balance in the body. (Blau, J. N., 1980)
The Aura: The phase that occurs right before a headache. The aura is a neurological phenomenon that usually lasts less between 30 to 60 minutes. 13-18% of migraine patients experience aura in every single migraine they have, and 13 -18% of migraine patients experience aura in some of the migraines they have. Symptoms can be visual or sensory. The visual symptoms occur in 99% of the aura cases and include vision disturbance with partial alteration in the field of vision. The sensory symptoms occur in 30-40% of aura cases, and include pain, numbness, and tingling feeling in the hand and arm of one side, and the nose and mouth on the same side. (Hansen, J. M. et al, 2012)
The Pain: Also known as the attack, and is the headache phase. During the pain phase most people experience unilateral headache, with some people experience bilateral headache. The headache comes with different intensities and usually get more intense during physical activity. The pain lasts between 4 and 72 hours for adults and can be less than 4 hours for children. The headache is also usually associated with neck pain. (Jes Olesen, 2006)
The Postdrome: The final phase, which occurs after the migraine attack. During the postdromal phase one experiences soreness in the same area of the migraine. Some patients also experience cognitive difficulties, mood changes, and weakness. (Kelman L., 2006)
Pathophysiology
The limbic brain regions associated with mood and depression include the hippocampus and the prefrontal cortex. Studies suggest that stress and depression are associated with atrophy and loss of neurons and glia, which contribute to the decreased size and function of these brain areas. There are two main hypotheses for the underlying mechanism of depression.
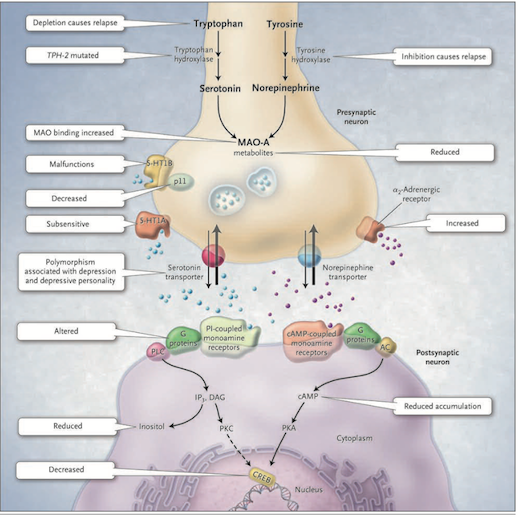
<style justify> The Monoamine-deficiency hypothesis: The first real indication that depression might result from a problem with the central nervous system modulatory systems came in the 1960s. A drug called reserpine, introduced to control high blood pressure, caused psychotic depression in about 20% of cases. Its mechanism of action involves the depletion of central catecholamines and serotonin by interfering with their loading into synaptic vesicles. Another class of drugs introduced to treat tuberculosis caused a marked elevation in mood. These drugs inhibit monoamine oxidase (MAO) which is the enzyme that degrades catecholamines and serotonin in the synaptic cleft. Furthermore, when it was discovered that the drug imipramine, introduced as an antidepressant years earlier, inhibits the reuptake of released serotonin and norepinephrine, thus promoting their action in the synaptic cleft. As a result of these observations, researchers developed the hypothesis that mood is closely tied to the levels of released monoamine neurotransmitters, norepinephrine and/or serotonin, in the brain. According to this monoamine hypothesis, depression is a consequence of a deficit in one of these diffuse modulatory systems [7]. </style>
Figure 1: The Monoamine-deficiency hypothesis (Source: Bedmaker & Agam, 2008) </style>
<style justify> This hypothesis postulates a deficiency in serotonin or norepinephrine neurotransmission in the brain. Serotonin is synthesized from tryptophan by the enzyme tryptophan hydroxylase; norepinephrine is synthesized from tyrosine which is catalyzed by the enzyme tyrosine hydroxylase. Both monoamine transmitters are stored in vesicles in the presynaptic neuron and released into the synaptic cleft, thereby affecting both presynaptic and postsynaptic neurons. Neurotransmission is mediated by serotonin (5-hydroxytryptamine 1A [5-HT1A] and 5-hydroxytryptamine 1B [5-HT1B]) or norepinephrine receptors [7].
There are several mechanisms by which the activity of these neurotransmitters can be terminated. One possibility is through reuptake through the specific serotonin and norepinephrine transporters and by feedback control of release through the presynaptic 5-HT1A and 5-HT1B regulatory autoreceptors for serotonin and the α2-noradrenergic autoreceptors for norepinephrine. Monoamine oxidase A (MAO-A) catabolizes monoamines presynaptically and thereby indirectly regulates vesicular content. The function of the 5-HT1B receptor is increased by the p11 protein and therefore a decrease in this p11 protein is thought to be implicated in depression [7].
On the postsynaptic neuron, serotonin and norepinephrine bind G-protein coupled receptors including the cyclic AMP (cAMP)-coupled receptor and the phosphatidylinositol-coupled receptor. The downstream effects of the cAMP-coupled receptor are to activate adenylyl cyclase which generates cAMP which in turn activates protein kinase A (PKA). The phosphatidylinositol pathway activates phospholipase C which generates two second messengers, IP3 (activates Ca2+ release) and diacylglycerol (activated protein kinase C (PKC)). The two protein kinases affect the cAMP response element–binding protein (CREB). Findings in patients with depression that support the monoamine-deficiency hypothesis include a relapse of depression with inhibition of tyrosine hydroxylase or depletion of dietary tryptophan, an increased frequency of a mutation affecting the brain-specific form of tryptophan hydroxylase (TPH-2), increased specific ligand binding to MAO-A, subsensitive 5-HT1A receptors, malfunctioning 5-HT1B receptors, decreased levels of p11, polymorphisms of the serotonin-reuptake transporter associated with depression, an inadequate response of G-proteins to neurotransmitter signals, and reduced levels of cAMP, inositol, and CREB in postmortem brains [7] [Figure 1]. </style>
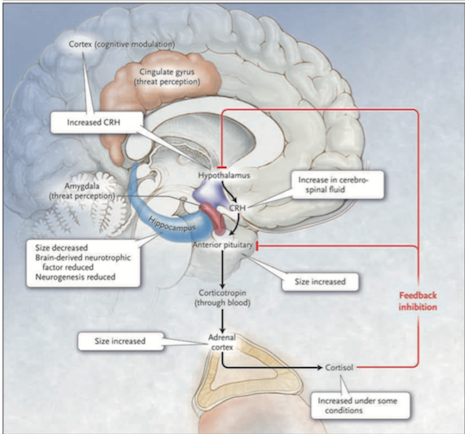
<style justify> The Diathesis-stress hypothesis: According to this hypothesis, the hypothalamic-pituitary-adrenal (HPA) axis is the main site where genetic and environmental influences converge to cause mood disorders. As mentioned earlier, depression can run in families and our genes can predispose us to mental illness. Furthermore, early childhood abuse or neglect, and other stresses of life, are important risk factors in the development of depression in adults. Hyperactivity of the HPA axis results in elevated blood cortisol levels as well as higher concentrations of corticotropin-releasing hormone in the cerebrospinal fluid. Injected CRH into the brains of animals produces behavioural effects that are similar to those of major depression: insomnia, decreased appetite, decreased interest in sex and increased behavioural expression of anxiety.[7] </style>
Figure 2: The HPA system in depression (Source: Bedmaker & Adam, 2008) </style>
<style justify> Abnormalities in the cortisol response to stress may underlie depression. The black arrows in Figure 2 show that in response to stress, which is perceived by the brain cortex and the amygdala and transmitted to the hypothalamus, corticotropin-releasing hormone (CRH) is released. This induces the anterior pituitary gland to secrete corticotropin into the bloodstream. Corticotropin stimulates the adrenal cortexes to secrete the glucocorticoid hormone cortisol. The red line in Figure 2 shows that cortisol, in turn, induces feedback inhibition in the hypothalamus and the pituitary, suppressing the production of CRH and corticotropin, respectively. Activation of hippocampal glucocorticoid receptors by cortisol normally leads to feedback inhibition of the HPA axis. In depressed patients this feedback is disrupted thus leading to the hyperactivation of HPA. A molecular basis for the diminished hippocampal response to cortisol is a decreased number of glucocorticoid receptors. The number of receptors is regulated by genes, monoamines and early childhood experiences. Findings in patients with depression that support the hypothalamic–pituitary–cortisol hypothesis include the following: cortisol levels are sometimes increased in severe depression, the size of the anterior pituitary and adrenal cortex is increased, and CRH levels in the cerebrospinal fluid and CRH expression in the limbic brain regions are increased. Furthermore, hippocampal size and the numbers of neurons and glia are decreased, possibly reflecting reduced neurogenesis due to elevated cortisol levels or due to reduced brain-derived neurotrophic factor. [7] </style>
<br> <br> <br> <br> <br> <br> <br> <br> <br> <br>
Treatment
There are several known, effective treatments for depression that vary from medicinal to psychological in nature. Despite these known methods, fewer than half of those affected in the world receive them. Barriers to effective care include a lack of resources, misdiagnosis, a lack of trained health care providers, and social stigma associated with mental disorders. [12]
Antidepressant: Two of the major classes of drugs used to treat this disorder are Selective Serotonin Reuptake Inhibitors (SSRIs) and Serotonin–norepinephrine reuptake inhibitors (SNRIs). The mechanisms of these drugs are described below.
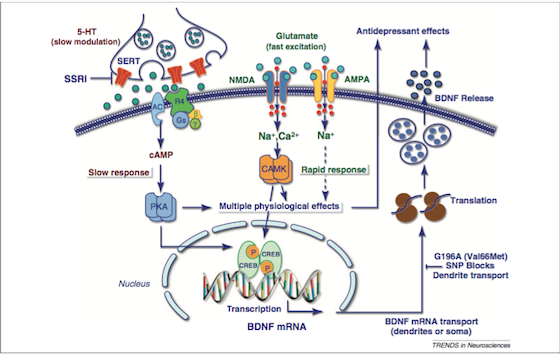
SSRIs: As the name suggests, these drugs prevent the reuptake of serotonin. They do this by inhibiting a monoamine transporter protein, SERT [Figure 3], that transports serotonin from the synaptic cleft to the presynaptic neuron. The SSRIs block the reuptake of serotonin, leading to increased concentrations of the neurotransmitter in the synaptic cleft [Figure 3] and, ultimately, to greater postsynaptic neuronal activity. SSRIs are actually a “successor” to SNRIs, as they are “selective” to serotonin, and usually do not affect other hormones in the nervous system. They are by far the most common drugs prescribed. Some examples of SSRIs include: Fluoxetine (Prozac), sertraline (Zoloft), and citalopram (Celexa). Side effects include: Sexual Dysfunction, Sleep Disorders, and headaches if treatment is suddenly stopped [13].
<html>
Figure 3: Signalling pathways and the treatment of depression (Source: Duman & Voleti, 2012)
</style>
<style justify> SNRIs: Like SSRIs, SNRIs prevent the reuptake of serotonin by inhibiting the activity of neurotransmitters. Unlike SSRIs, SNRIs also prevent the reuptake of the neurotransmitter Norepinephrine. These can be thought of as the less refined predecessor to SSRIs. Another class of antidepressants, known as tricyclic antidepressant (TCAs), also act in the same way as SNRIs. [13]
Psychotherapy: In the clinic, psychotherapy is often used as an alternative or in conjunction to pharmacological treatment. The main forms of psychotherapy used are cognitive behavioural therapy (CBT) and Interpersonal psychotherapy (IPT).
Cognitive Behavioural Therapy (CBT): CBT is founded on the principle that initial thoughts and perspectives are the root of associated behaviour. In CBT, the psychotherapist and patient work together to determine the patterns and markers of detrimental thought patterns. The focus on thought patterns allow it to be used to deal with the feelings of worthlessness in depression.[9]
Interpersonal psychotherapy (IPT): IPT is based on the principle that depressive symptoms are influenced by the relationships the patient holds with other people. The therapy acts to identify and analyze how disruptions in a patient’s relationship with another party plays a role in their behaviour. For example, the challenges of pregnancy often put a strain on the relationship between the new mother and the relationship with her spouse. The economic and personal challenges of having a child may affect the relationship between the new parents, and lead to depressive symptoms in the mother (or even father). Interpersonal therapy analyses relationships from the perspectives of
attachment, communication, and social importance. [9]
</style>
Conclusion
Overall, depression is a heterogenous, burdensome disorder that exhibits a highly variable course, an inconsistent response to treatment and an incomplete understanding of the underlying neurobiology. Its onset is gradual and it can manifest itself not only in psychological symptoms but physical symptoms as well. Future initiatives are focusing on novel treatments that can start to take effect quicker than the 4-5 weeks required for antidepressants. Research is beginning to look at the use of theta-burst stimulation which involves delivering magnetic pulses to the brain. It is a fast acting, simple, non invasive form of treatment. These magnetic pulses stimulate electric current in the brain and the hope is that repeated treatment can capitalize on the brain's neuroplasticity by changing the way in which the brain's neurons fire. However, this is a very new field and much more research needs to be done surrounding the efficacy and safety of this treatment.