This is an old revision of the document!
Table of Contents
Juvenile Idiopathic Arthritis Powerpoint
Juvenile Idiopathic Arthritis
Juvenile idiopathic arthritis (JIA), also known as juvenile rheumatoid arthritis (JRA) is a chronic form of arthritis that can be seen in children between the ages of 1-16 (Shiel, n.a). This disease refers to a group of conditions that pertain to joint inflammation (Genetics Home Reference, 2015). According to The Genetics Home Reference, “It is classified as an autoimmune disorder which means that the immune system malfunctions and attacks the body’s organs and tissues, in this case joints (Genetics Home Reference, 2015).” Through much research, it has been determined that there are seven types of JIA which are classified in accordance to their signs and symptoms, number of affected joints, results from medical tests and familial history (Genetics Home Reference, 2015). All seven types of JIA are chronic, thus individuals must develop coping methods that are long lasting and effective. The prevalence of the seven types of JIA are shown in Figure 2. <style float-right> </style>
Subtypes
Systemic JIA
Systemic juvenile idiopathic arthritis causes inflammation in one or more joints, and its symptoms include high daily fevers that can last up to two weeks either preceding or accompanying the arthritis. A skin rash or enlargement of lymph nodes, liver or spleen are symptoms that differentiate this type of juvenile arthritis from other types (Genetics Home Reference, 2015).
Oligoarticular JIA
Oligoarticular juvenile idiopathic arthritis refers primarily to the inflammation of joints. This form of arthritis is prevalent in four or fewer joints in the first six months from when the disease was diagnosed. Depending on the onset of the condition, this form of arthritis can be divided into two subtypes. If the arthritis has not spread to more than four joints after six months, it is considered to be persistent oligoarthritis. If more than four joints are affected, it is classified as extended oligoarthritis (Genetics Home Reference, 2015).
Rheumatoid Factor Positive Polyarticular JIA
When inflammation is present in five or more joints within the first six months of the disease, it is considered rheumatoid factor positive polyarticular JIA. Patients with this condition have a positive blood test for proteins called rheumatoid factors. A rheumatoid factor is the amount of protein found in the blood that may attack healthy tissues in the human body. This type of JIA displays symptoms similar to the predominant types of arthritis in adults (Genetics Home Reference, 2015).
Rheumatoid Factor Negative Polyarticular JIA
This type of arthritis is similar to the rheumatoid factor positive polyarticular JIA as it also affects five or more joints. As evident in its name, it tests negative for the rheumatoid factor in the blood (Genetics Home Reference, 2015).
Psoriatic JIA
Psoriatic juvenile idiopathic arthritis is usually detected in combination with a skin disorder called ‘psoriasis’. This condition is understood by the red patches and irritated skin that are covered by flaky, white scales. Depending on the individual, some are affected by this skin disease prior to developing arthritis, and others notice the the skin condition while first developing arthritis. Other symptoms of this type of arthritis include abnormalities of the fingers and nails like uneven lengths and deformed fingers or vision problems (Genetics Home Reference, 2015).
Enthesitis-related JIA
Enthesitis-related juvenile idiopathic arthritis is classified by tenderness where the bone meets the tendon, ligament, or other connective tissue. This is usually accompanied by inflammation in joints and other related areas (Genetics Home Reference, 2015).
Undifferentiated Arthritis
Undifferentiated arthritis is given to patients who have symptoms that are not explained by the descriptions of any of the above forms of JIA or who have fit the criteria for more than one of the given descriptions of JIA (Genetics Home Reference, 2015).
Epidemiology
There are two broad categories for genetic susceptibility genes: human leucocyte antigen (HLA) genes and non HLA-related genes. As a polygenic disease, JIA is mostly affected at the HLA region, while the non-HLA loci exhibit moderate or weak genetic influence on susceptibility (Prahalad and Glass, 2008). JIA is influenced by both HLA class I and HLA class II alleles, which contain certain peptides leading to the activation of certain autoreactive T cells (Wedderburn et al., 2001). Several genetic studies have shown the contribution of polymorphisms in the major histocompatibility complex (MHC). The MHC region is on chromosome 6 and is packed with more than 200 genes, many of which are essential to the immune system. Since MHC class II genes play a great role as a genetic risk factor for JIA, CD4+ T cells play a crucial role in disease development. Associations between HLA polymorphisms and JIA subtypes have been reported in multiple populations (Figure 8) (Prahalad and Glass, 2008).
[1]
In a study done by Saurenmann et al, questionnaires pertaining to ethnicity were distributed to patients with JRA and then followed up at the Hospital for Sick Children in Toronto (Saurenmann, 2007). When the data was collected, the relative risk of developing JRA was calculated and the results were compared with data from the age matched general population in the Toronto region (Saurenmann, 2007). The frequency at which JRA has been perceived shows that European descendants had about 69.7% of their patients diagnosed with JRA, which patients in the Toronto region has about 54.7% (Saurenmann, 2007). Statistically lower percentages were shown to patients who were of the black, Asian, or Indian subcontinental origin (Saurenmann, 2007). Kids from the European origin had a higher relative rate for developing any of the subtypes of juvenile arthritis, except oligoarthritis or psoriatic (Saurenmann, 2007). Patients of the Asian origin showed to have a greater chance of being diagnosed with enthesitis-related JIA while those of black or Native North American origin were more likely to develop polyarticular rheumatoid positive JIA (Saurenmann, 2007).
Symptoms & Diagnosis
JIA is diagnosed once symptoms are persistent for at least six weeks since the diagnosis (Shiel, n.a). Common symptoms of JIA include swelling, redness, and warmth of joints, however, many researchers and scientists attempt to formulate a criteria for the precise diagnosis of JIA (Nelson & Kilegman, 2016). The proposed criteria includes six requirements. Firstly, polyarticular or monoarticular arthritis must be present for at least six weeks or in the presence of the following: Iritis, rash, flexion contractures, ankyloses, muscle wasting, anemia, white blood cell count of 20000, cervical spine pain (Grossman & Mukhopadhyay, 1975). The second criteria is expressed as polyarticular or monoarticular arthritis for 6 weeks or less having the following characteristics: nonmigratory for at least 1 week, no symptomatic response to therapeutic blood levels of salicylate (20 mg/100 ml or above) preponderance of small joint involvement, involvement of the temporomandibular joints, morning stiffness (Grossman & Mukhopadhyay, 1975). Next, polyarticular or monoarticular arthritis for 6 weeks or less accompanied by pericarditis in the absence of endocarditis (Grossman & Mukhopadhyay, 1975). Fourth would be classified as constitutional symptoms known as any combination of fever, weakness, or weight loss (Grossman & Mukhopadhyay, 1975). The fifth criteria mention the elevated erythrocyte sedimentation rate. Lastly the exclusion of all other diagnoses such as rheumatic fever, systemic lupus erythematosus, periarteritis nodosa, dermatomyositis, scleroderma, tuberculosis synovitis, leukemia, lymphoma, septic arthritis, osteomyelitis, sickle cell anemia and serum sickness (Grossman & Mukhopadhyay, 1975). This set of criteria was put together to ensure that the diagnosis of JIA was accurate and any symptoms shown couldn’t be associated with any other chronic disease. There are many symptoms that occur for JIA to be an option for diagnosis.
Flares
Flares are known as a classification of symptoms referring to joint pain and inflammation and can last from time periods ranging from weeks to months (Shiel, n.a). JIA patients tend to have periods of remission, where these symptoms aren’t as prevalent as they would have been in the past (Shiel, n.a). Following this grace period where pain is minimal, these symptoms can reappear and this is known as a relapse (Shiel, n.a). This notion of relapsing and remission varies from patient to patient and can also be a known trend with other symptoms as well (Shiel, n.a).
Fever
Fever is a common symptom for JIA and can be classified to many degrees. A fever in an individual who may have JIA can be recognized in three different states. “Intermittent fever with a daily single high spike of temperature to 104-105 ~ F, then returning down to a normal temperature. A remittent fever with a persistent elevation of 100-101 ~ F with occasional, somewhat irregular increases in temperature to 103-104 ~ F (Grossman & Mukhopadhyay, 1975). Lastly, low grade fever with periodic elevation of temperature to 100-101 ~ F, the elevations frequently occurring in the late afternoon or evening, the morning temperature being normal (Grossman & Mukhopadhyay, 1975).”
Morning Stiffness
Morning stiffness is a symptom that helps with the diagnosis of JIA. It constitutes as difficulty in moving muscles after a period of rest or inactivity (Miller, 1994). Individuals feel this pain in the morning after waking up from a night’s sleep and is not a result of pain (Miller, 1994). With activity and movement throughout the day it tends to disappear (Miller, 1994). It can vary in the time that it lasts from a few minutes to many hours (Miller, 1994). The degree to which morning stiffness occurs can also vary. It can be so sever that the child cannot move without help from another person (Miller, 1994). In these circumstances, the combination of a warm bath and an increase in activity will aid with the relief of the stiffness (Miller, 1994). Other times in the day where morning stiffness is prevalent is after a nap or sitting down for a prolonged period, however, this is usually not as sever as the morning occurrence (Miller, 1994). Morning stiffness is an important differential characteristic between JIA and rheumatic fever or septic arthritis and if it is noted to be happening, physicians and other medical assistance should take a further look into it (Miller, 1994).
Rheumatoid Rash
This symptom is extremely helpful when diagnosing JIA, especially in the acute onset of disease (Miller, 1994). According to Miller, “The characteristic rheumatoid rash is an erythematous, salmon-pink, evanescent, usually circumscribed macular (although occasionally maculopapular) eruption involving the trunk, neck, velar aspect to the arms, inner aspect of the thighs, buttocks and face. It may last for only a few minutes, a few hours or several years (Miller, 1994).” Again, the degree to which the rash may last varies, lasting from only a few minutes to many hours and appears strongly during times of high fever or during warm baths (Miller, 1994). Many times, the rash experienced in patients who have JIA can be mistaken for erythema annulare or marginatum, however, erythema annulare or marginatum does not spread to the face region which is prevalent in the rheumatoid rash of JIA (Miller, 1994).
Subcutaneous Nodules
Nodules have been observed in approximately 10% of children who have been diagnosed with JRA and can appear subcutaneously (Miller, 1994). Characteristics of nodules include varying in sizes (from a few millimeters to several centimetres in diameter) nontender, no attachment to overlying skin and therefore move freely under the skin (Miller, 1994). Many times, they are found over the extensor tendon sheath of the hands, specifically over the metacarpophalangeal, proximal interphalangeal and distal interphalangeal joints (Miller, 1994). They are also found near the olecranon process of the elbow, over the anterior tibial surfaces and around the wrists and when fever is prevalent in the patient, nodules are found along the tendons of the erector spinae group and over the aponeurosis of the scalp (Miller, 1994).
Uveitis Eye condition
Juvenile rheumatoid arthritis can also lead to an eye condition called uveitis, also named iridocyclitis or iritis (Goldstein et al, 2013). This may or may not lead to any symptoms arising, however, some symptoms of this condition are red eyes, eye pain, vision changes and sensitivity to light (Goldstein et al, 2013). Uveitis is known as the swelling and irritation of the uvea, which is the middle layer of the eye (Goldstein et al, 2013).
Blood Tests for JIA
Rheumatoid factor (RF) is a protein that is produced in the blood in some forms of arthritis (SickKids, 2012). This is more common in adults with rheumatoid arthritis, however, it is found in 5% of children with JIR (SickKids, 2012). The RF test is a test that is used to detect and measure levels of a specific antibody directed against the blood component immunoglobulin (Arthritis Foundation, 2016).
Liver function test (LFT) is a test that determines if the liver is healthy and working normally (Arthritis Foundation, 2016). There are many medications that are used to treat arthritis such as, methotrexate that are metabolized in the liver (Arthritis Foundation, 2016). These medications may play a role in overburdening the liver and therefore doctors may order an LFT in order to determine the medication that is causing the damage (Arthritis Foundation, 2016).
Antinuclear antibody (ANA) is a test used to look at autoantibodies in the blood (SickKids, 2012). Autoantibodies are proteins in the immune system and is also a good indicator to whether children and teenagers with JIA have an increased risk of eye disease (SickKids, 2012).
Complete Blood Count (CBC) measures three types of cells that are found in the blood; red cells (carry oxygen), white blood cells (fight infection) and platelets (cause blood clots) (Arthritis Foundation, 2016). This test is useful when discovering more about the condition, for example, kids with low red blood cell counts are usually ones who are suffering from JIA (Arthritis Foundation, 2016).
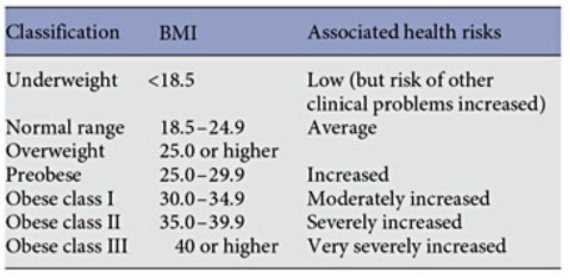
Figure 4: BMI Calculation Equation from http://www.heartnewslinks.com/editors-blog/body-mass-index-bmi-bad
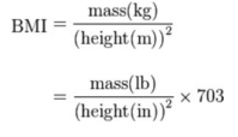
Figure 5: BMI-for-Age Percentile Ranges for Children from https://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html>
Causes and Risk Factors
It has been determined that most cases of JRA are sporadic, meaning that they occur in patients who don’t necessarily have a history of the disorder in their family (Genetics Home Reference, 2015). With that being said, there are many causes that occur prior to the diagnosis of JRA that have been mentioned to potentially lead to or affect the prevalence of JRA. Infectious agents, immunologic abnormalities of the host, physical trauma to joints, psychological trauma to the child, and allergy or reactions to drugs, foods, or toxins can all potentially lead to an individual to JRA (Schaller, 1997). Keeping in mind that there is no clear evidence that proves these are leadings causes of JRA (Schaller, 1997). JRA is not considered to be a familial disease, except in the place in which there is an onset of pauciarticular arthritis (Schaller, 1997). Also, there has been no evidence showing that JRA is transmissible. Various kinds of JRA have been shown to differ in sex, age, types of complications and prognosis, however, epidemiologic studies have not be able to clarify these observations (Schaller, 1997). A small percentage of cases of JRA have shown to have run in the family, however the inheritance pattern of the conditions is unclear (Genetics Home Reference, 2015).
Maternal smoking has also been observed to potentially cause or play a role in the onset of JRA through various ways (Symmons, 2005). Firstly, a mother who smokes while pregnant can induce some permanent immunological abnormality in the child which can later lead to arthritis (Symmons, 2005). Smoking while pregnant could also cause a low birth weight which could in turn lead to an increase in the susceptibility to infection and later, JRA (Symmons, 2005). Lastly, the continual smoking, even after a baby is born may lead to a contaminated environment which could ultimately lead to the onset of JRA later on during the early years of that child’s life (Symmons, 2005).
Pathophysiology
Genetic Susceptibility
JIA is believed to be a complex genetic trait. A complex genetic trait is defined as phenotypes not exhibiting classic mendelian inheritance patterns and therefore, cannot be attributed to variants in a single gene locus. Thus, JIA is a disease which is believed to be determined by a number of genetic and environmental factors (Glass and Giannini, 1999).
HLA and non-HLA Polymorphisms
There are two broad categories for genetic susceptibility genes: human leucocyte antigen (HLA) genes and non HLA-related genes. As a polygenic disease, JIA is mostly affected at the HLA region, while the non-HLA loci exhibit moderate or weak genetic influence on susceptibility (Prahalad and Glass, 2008). JIA is influenced by both HLA class I and HLA class II alleles, which contain certain peptides leading to the activation of certain autoreactive T cells (Wedderburn et al., 2001). Several genetic studies have shown the contribution of polymorphisms in the major histocompatibility complex (MHC). The MHC region is on chromosome 6 and is packed with more than 200 genes, many of which are essential to the immune system. Since MHC class II genes play a great role as a genetic risk factor for JIA, CD4+ T cells play a crucial role in disease development. Associations between HLA polymorphisms and JIA subtypes have been reported in multiple populations. (Table X) (Prahalad and Glass, 2008).
In addition to associations between numerous HLA variants and JIA, non-HLA polymorphisms have also shown to be linked to JIA. For example, genes such as PTPN22, tumor necrosis factor (TNF) alpha (TNFA), MIF, WISP3 and SLC11A6 have been associated with JIA (Figure 9) (Prahalad, 2004; Rosen et al., 2003).
Twin Studies
Family studies have provided strong evidence for genetic factors contributing to the susceptibility to JIA. For instance, twin and affected sibling pair (ASP) studies have supported the role for genetic susceptibility to JIA. Specifically, they have shown that monozygotic twin concordance rates for JIA vary between 25 to 40%, a stark contrast to the population prevalence of 1 in 1000 of having the disease (Ansell et al., 1969; Baum and Fink, 1968; Savolainen et al., 2000).
In the largest twin study from the JIA ASP registry conducted by Prahalad and colleagues in 2000, 14 pairs of twins concordant for JIA registered in the National Institute for Arthritis and Musculoskeletal and Skin Diseases were analyzed. Of these 14 pairs of monozygotic twins, 12 were concordant for presence or absence of anti-nuclear antibodies. Prahalad and colleagues found that the first twins to develop JIA did so with an average of 5.5 months before the second twins. This was statistically significant and different compared to the 104 non-twin affected siblings pairs in the registry, who showed a 37 month difference in age at onset between the first and second sibling (Prahalad et al., 2000). Together, these studies solidify evidence for genetic factors in the susceptibility to JIA.
Genetic Variables Underlying Autoimmunity
Several studies have shown that clinically distinct autoimmune phenotypes cluster in individuals and families. The data supports the hypothesis that common genetic factors might predispose to clinically distinct autoimmune phenotypes. There are genetic variants which influence susceptibility to multiple clinically distinct autoimmune disorders (Figure 10) (Prahalad and Glass, 2008).
Environmental Factors
The cause of JIA is assumed to be multifactorial, as in the case of most human autoimmune diseases. Unlike JIA, a healthy immune system consists of effector and regulatory mechanisms which are kept in balance. Therefore, the innate and adaptive immune systems closely interact. A genetically susceptible individual might develop a deleterious and uncontrolled response towards a self-antigen on exposure to an unknown environmental trigger. In JIA, it can lead to a self-perpetuating loop of activation of both innate and adaptive immunity, causing tissue damage (Prakhen, Albani, Martini, 2011).
Stress and Physiological Factors
The influence of stressful life events and psychological factors before the onset of JIA as a disease trigger has been studied. In a study by Henoch and colleagues which compared 88 children with JIA to 2952 geographically matched controls, results showed that children whose parents were unmarried due to divorce, separation, or death comprised 28.4% of the JIA population, compared to 10.6% in controls (Henoch, Batson, Baum, 1978).
Stress was also suggested as a contributing factor to the disease. It is a known stimulator to the sympathetic nervous system (SNS) and thus increases the production of interleukin 6, which is one of the most important inflammatory cytokines in JIA (Roupe et al., 2000).
Although psychological factors and stress may play a role for the onset of JIA, more research needs to be conducted since past studies have had several methodological shortcomings (Berkun, Padeh, 2010).
Smoking
Smoking is the strongest known environmental risk factor for developing rheumatoid arthritis (RA) in adults. The risk of RA from smoking has been showed by the number of shared epitope copies, which suggest gene-environment interaction. Specifically, the strongest known genetic risk factor for RA is a specific sequence of amino acids on HLA-DRB1 allele. In addition, the risk of developing RA from gene-environment interactions increases with the intensity of smoking (Liao et al., 2009).
All this suggests that smoke is a stimulator of the immune system and that the exposure to tobacco products during fetal life may influence the developing immune system of the fetus. This can lead to an increased susceptibility to infectious agents and thereafter, trigger arthritis as well as subsequent autoimmune diseases. Jaakkola and Gissler conducted a study assessing the relation between maternal smoking in pregnancy and the risk of inflammatory polyarthropathies, in particular JIA in the first years of life. 58 841 newborn Finnish children until the age of 7 were analyzed. Findings showed that there was a 2-fold higher rate of polyarthropathies during the first 7 years of life in children of smoking mothers, compared to non-smoking ones. In addition, the maternal smoking effect was found prevalent to girls, who experienced 6-fold greater likelihood for JIA compared to unexposed boys (Jaakkola and Gissler, 2005).
Infectious Agents and JIA
Infectious agents are believed to be important environmental factors in the development of autoimmunity. An infectious agent may induce a cross-reactive immune response, thereby leading to inflammation provoked by antigen-presenting cells (APCs). This can lead to increased immunogenicity, priming of T cells and subsequent autoimmunity (Berkun and Padeh, 2009). A study by Carlens and colleagues showed that infections during the first year of life and factors related to size and timing of birth were associated with increased risk of developing JIA (Carlens et al., 2009) . However, more research needs to be conducted to understand the role of environmental factors on JIA.
Immunology of JIA
The overarching mechanism in all Juvenile Idiopathic Arthritis (JIA) subsets is the activation of the immune system. Different components are involved in each subtype and additional variation may exist within subtypes (Malmström, Catrina & Klareskog, 2016). Over the years, there has been considerable progress in understanding the immune-inflammatory reaction.
Auto-Immunity
Much of the scientific community believe the disease is initiated as a result of molecular mimicry between epitopes on antigens present on infectious agents and autoantigens. Molecular mimicry, by epitope spreading, overcomes tolerance mechanisms and results in autoimmunity. Over the years, two major subtypes of JIA have been identified on the basis of the presence or absence of auto-antigens: antibodies to citrullinated protein antigens (ACPAs) and rheumatoid factor (RF) (Malmström, Catrina & Klareskog, 2016).
Both subsets have different disease courses. The seropositive form usually means severe pathology. The seronegative forms of arthritis are not well understood and appear to be more heterogeneous compared to the seropositive variant (Malmström, Catrina & Klareskog, 2016).
Antibodies to Citrullinated Protein Antigens (ACPA)
ACPAs are important for the diagnosis of JIA. These are the patient’s own antibodies which have been modified by citrullination, a process where proteins’ arginine residues are converted to citrulline post-translationally by the enzyme peptidyl arginine deiminase (PAD) (Figure 11). Once modified, the body recognizes its own antigens to be foreign, causing an immune response (Demoruelle & Deane, 2011).
Rheumatoid Factor (RF)
RF is an autoantibody derived from IgM that targets the Fc portion of IgG, specifically IgG1 to form immune complexes. These complexes are present in the synovial fluid along with IgG-producing B cells. Additionally, it can form complexes with complement proteins further promoting inflammation. Although RF has been associated with the pathogenesis of RA, it is possible for patients to develop arthritis without it (McInnes & Schett, 2011).
Interestingly, the literature suggests that RA-associated antibodies are present in the blood several years before joint inflammation signs are present. It is possible that anti-citrullination precedes the onset of joint inflammation which may be triggered in the lungs or other mucosal regions (Malmström, Catrina & Klareskog, 2016).
Inflammation
JIA is considered a T-cell mediated disease in which CD4+ T cells exacerbate inflammation in rheumatoid joints. Majority of the CD4+ T cells in joints appear to be of the Th1 type, with memory and activation markers. T cells in joints increase in number by recruitment, resistance to apoptosis and accumulation. For this process, cytokines are of importance.
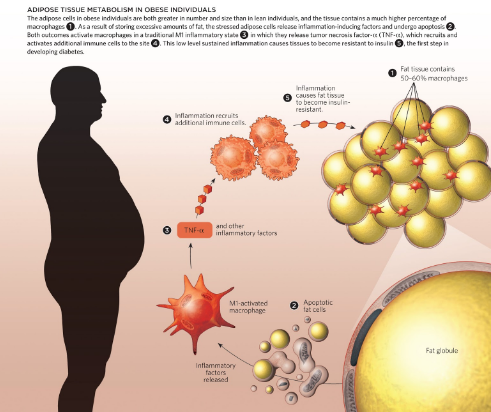
Cytokines are protein messengers that transmit signals from one cell to another by binding to specific receptors on the surface of cells. Both pro- and anti-inflammatory cytokines, chemokines, and mitogenic factors are produced, but proinflammatory mediators predominate during the active phase of disease.Tumor necrosis factor alpha (TNFα), IL-1, IL-6 and IL-17 are of key importance in the pathogenesis of inflammation in RA. IL-1 and TNFα are also key players in the regulation of mediators of connective tissue damage by synoviocytes, including matrix metalloproteinases (MMPs) and prostaglandins (Nath Maini, 2010).
ACPAs may also bind to citrullinated proteins directly in the synovial membrane. Immune complexes between citrullinated proteins ,such as fibrinogen, and ACPA-igG can drive inflammation (including the production of IL-6 and tumor necrosis factor) by engaging both toll-like receptor (TLR4) and Fc receptors (Nath Maini, 2010).
Furthermore, these cytokines in combination with the cytokines monocyte colony stimulating factor (M-CSF) and receptor activator of NF-κβ ligand (RANKL), activate osteoclasts leading to bone damage. TNFα regulates production of IL-1 and together these two cytokines induce rheumatoid inflammation and damage (Nath Maini, 2010).
Both ACPA- and RF-dependent events could contribute to the initiation and propagation of chronic synovial inflammation, and further synergize with T cell activation and enhance the local production of autoantibodies (McInnes & Schett, 2011).
Bone Destruction
Osteoclasts, cells that line the bone and are responsible for the breakdown of bone tissue, have an important role in ACPA-dependent pathology. ACPAs generated from B cells found in the synovial fluid of patients with RA are able to promote osteoclastogenesis and bone resorption. The effects of these antibodies are mediated both by direct recognition and activation of Fc receptors on osteoclasts. Antibodies can exert a specific function on osteoclasts at the earliest stages of disease development and before joint inflammation appears (McInnes & Schett, 2011).
The literature suggests that osteoclasts and osteoclast precursors might be the major cell types that express citrullinated antigens on their surface in the normal non-inflamed bone and joint compartment, making precursor cells prime targets for circulating ACPAs. This feature is associated with the role of PADs but the exact role of PADs and citrullination in osteoclast differentiation is unknown (Malmström, Catrina & Klareskog, 2016).
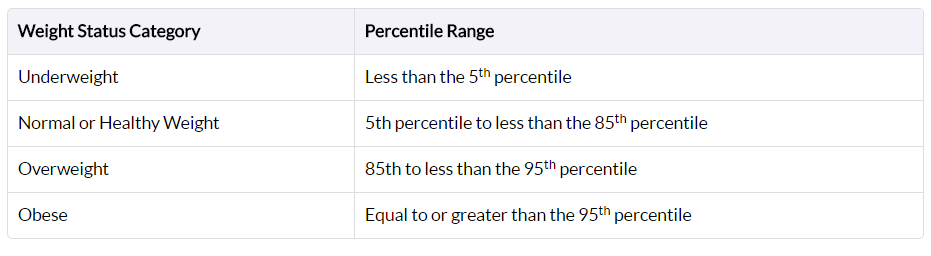
Figure 9: Human obesity gene map, updated in 2005. From http://onlinelibrary.wiley.com.libaccess.lib.mcmaster.ca/doi/10.1038/oby.2006.71/full
start
Treatments
Goals of Weight Loss and Management
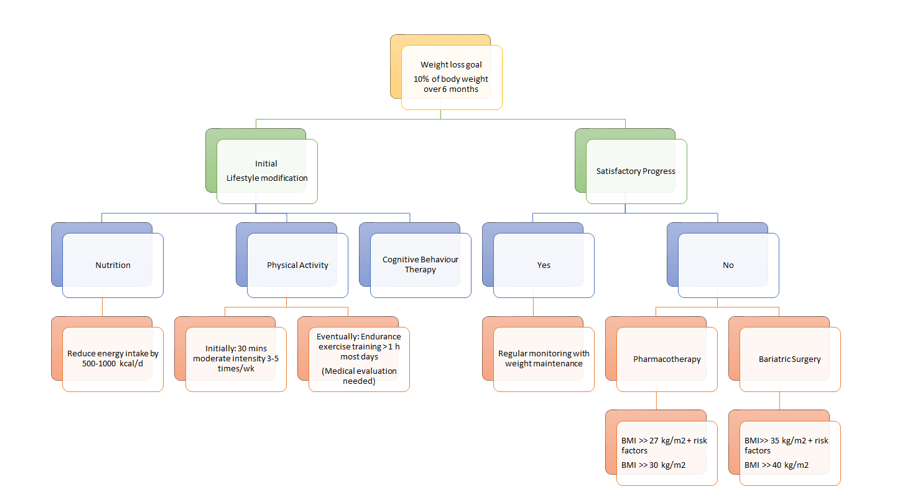
When undergoing weight loss therapy, practice guidelines issued by the National Heart, Lung and Blood Institute and the North American Association for the Study of Obesity recommend an initial weight loss goal of approximately 10% from baseline over a period of 6 months of therapy [25].
A weight loss of 10% has the potential to improve glycemic control, blood pressure control and lipid levels, especially in individuals with Type 2 diabetes or hypertension. Additionally, it might help to reduce symptoms from comorbidities, such as gastroesophageal reflux and osteoarthritis. If weight loss is maintained over a long period of time, adverse clinical outcomes, such as myocardial infarction, stroke and cardiovascular-related deaths, can be reduced [26].
Intervention
For the optimal weight loss and health benefits, it is important to adopt lifestyle modifications, such as dietary therapy, physical activity and cognitive behaviour therapy. Typically, health care practitioners recommend their patients to pursue the lifestyle modifications for 6 months. Thereafter, clinicians assess whether they have reached the weight loss goal of 10% from baseline estimates. If patients have attained a satisfactory progression upon evaluation, it is recommended that they maintain their lifestyle modifications for sustainable weight loss results. Regular monitoring is a crucial aspect of ensuring a healthy lifestyle, as the influences of side effects must also be considered. In the case that patients have not attained their recommended weight after 6 months, health care practitioners typically recommend pharmacotherapy and/ or bariatric surgery to achieve their weight loss goal. The most conclusive results are seen when either pharmacotherapy or bariatric surgery are used in conjunction with lifestyle modifications [25].
Diet
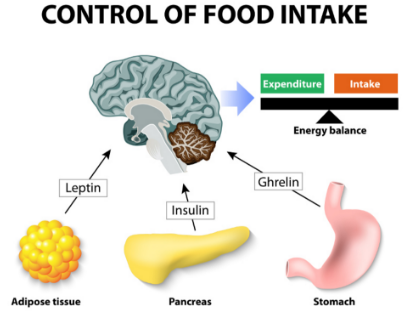
The first component of lifestyle modifications to treating obesity is undergoing dietary therapy (Figure 10). When assessing diet management in obese patients, weight reduction is highly dependent upon energy intake in comparison to energy expenditure [27].
According to a study conducted by Poirier and Despres (2001), it has been concluded that approximately 1 pound of mass can be lost within a week without any changes being made to the level of physical activity [27]. There are various types of diets that an individual can choose to pursue. Each type of diet is subjective to the patient, therefore it can produce differing results. Three diets that are typically suggested to obese patients are the low carbohydrate diet, the low-fat diet and the high protein diet.
The low carbohydrate diet is consists of a reduced carbohydrate consumption [28]. Long-term studies have shown that low carbohydrate diets produce significant results at the 3 and 6 month points. However, results become insignificant at about a year onwards [29]. When examining the weight reduction that high protein diets produced, the results were indifferent [29]. Patients were losing a significant amount of weight up until about a year and then the results started to decrease [29]. Studies about the low-fat diet have shown that patients saw a significant weight reduction for about three years and then results were insignificant [30].
Although all three of these diets show promising results, the low carbohydrate and high protein diets show short term effects, while the low fat diet seems to display long term fat reduction. In conclusion, it is important to note that many individuals are susceptible to regaining their weight, thus a sustainable lifestyle is integral. Managing weight loss through dietary means can be difficult, however it can be made easier when incorporating physical activity into the daily routine.
Weight Loss Programs
Due to the vast technological advances of our time, there are many weight loss programs available that are highly accessible. Although there are a wide variety of programs to choose from, it is always encouraged to keep in mind that not every weight loss program will produce the same kinds of results for everyone. It is always important to consult with a family physician when trying to find a weight loss program that will have a positive effect on a personal weight reduction.
Some examples of weight loss programs that are available for further investigation are listed below:
The Paleo Diet: It works to incorporate whole foods, lean protein, veggies, fruits, nuts, and seeds and encourages to stay away from foods with sugars, dairy and grains.
The Vegan Diet: It is an ‘extreme’ vegetarian diet that works to eliminate dairy, eggs, and animal derived products, such as gelatin, honey, whey, and vitamin D3.
The Low Carbohydrate Diet: It encourages individuals to eat an unlimited amount of protein and fat, while completely eliminating carbohydrates.
The Ultra Low-Fat Diet: It consists of a diet where 10% or less calories come from fat. This diet is almost entirely made up plant based food items, with a very limited intake of animal products.
The Zone Diet: This diet encourages participants to balance each meal with one third of protein, and two thirds of fruits and veggies. A small amount of fat that comes from natural and healthy sources, such as avocado, almonds, or olive oil can also be consumed.
Intermediate Fasting: This diet challenges its participants to fast during portions of the day, while restricting the calorie intake during the times you do choose to eat. This diet is most efficient when you aren’t overeating during the times where the fast has been broken.
There are a few options when trying to reduce weight loss. All of the diets that are listed above prove to have a positive impact on weight reduction. However every diet has its consequences. When the body is restricted from having certain kinds of foods, nutrients, minerals and vitamins are compromised. For example, if an individual were to go on the paleo diet, the restriction of whole grains and dairy prevents individuals from consuming certain vitamins. A family physician or a dietician would be able to provide the most representative diet plan for each individual [31].
Physical Activity
The second component of the lifestyle modifications approach to treating obesity is to be physically active. The purpose behind weight loss and management programs is to stop future weight gain, decrease body weight and permanently maintain a lower body weight [32]. Maintaining a physically active lifestyle is known to be key to a long term weight maintenance, because it increases the energy expenditure through caloric deficit [33]. When incorporating physical activity into a daily routine with hopes of maintaining the reduction of body weight, it is important to remember that different training modalities such as walking, cycling and swimming can have a different impact on different individuals [34].
When involved in physical activity, many adaptive responses take place, which cause a more efficient system for oxygen transfer to muscle [32]. In addition, reduced adipose tissue mass representing an important mechanical advantage, allows better long-term work [32]. Physical training helps counteract the permissive and affluent environment that predisposes reduced-obese subjects to regain weight [32]. Many studies have recommended thirty to forty-five minutes of moderately intensive physical activity, to be done 3-5 times a week [35]. In particular, public health interventions have promoted walking as a physical activity, since it is safe, accessible and a low intense aerobic exercise that results in high fat loss [32]. Losing weight through physical activity can be very difficult, especially for obese patients and therefore, it is important to set realistic weight loss goals of about 0.5-1 pound per week, with the assistance [32]. Because it may seem like small steps are made in weight reduction while working out, it is important for patients to remain determined and persevere to reach their goals [32]. Keeping a positive attitude during this process can be very difficult and so, it is extremely important for the patient to have one-on-one interaction between the clinician or healthcare professional on a regular basis [32].
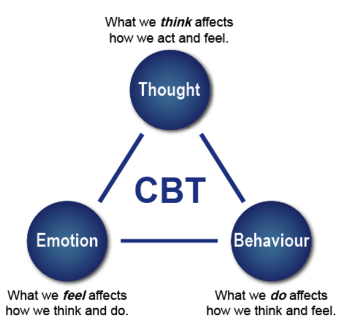
Cognitive Behaviour Therapy
The third component of lifestyle modifications is to undergo cognitive behaviour therapy (CBT) to assess one’s current habits and identify factors, stressors or situations that may trigger one’s overeating habits and contribute to their obesity (Figure 11). With a CBT approach, patients suffering from obesity can get help through counseling, support groups, as well as adopt the family-based approach [25,26].
The purpose of the CBT treatment is not to eliminate a psychiatric disorder but to change eating and exercise behaviours [36]. This intervention aims to educate individuals on how to change problematic behaviours. Firstly, CBT is based on the cognitive conceptualization of the processes that lead to overeating. Specifically, thoughts and thinking patterns that are considered central to the problem. Secondly, CBT is focused on altering the cognitive and behavioural mechanisms that maintain the problem behaviour. Lastly, CBT uses both cognitive and behavioural techniques to maintain healthy mechanisms [37]. The diagram here shows different components that contribute to CBT.
Counselling is one way a patient can undergo CBT. It can either be delivered on a one-on-one basis, or in a group setting of approximately 10 participants with a trained healthcare professional [38,39]. A study conducted by Renjilian and colleagues comparing the two treatment modalities concluded that participants who were randomized to receive group-based therapy lost more weight after 26 weekly sessions compared to those who were treated individually. Specifically, those receiving group therapy lost about 11 kg after 26 weekly sessions, in comparison to 9 kg for those who were individually treated [40].
In addition to counselling, having a support network is important. This is especially true if the individual is undergoing drastic changes. Receiving encouragement from family, friends and health care practitioners can be very motivating during challenging times of the weight loss and maintenance programs. Furthermore, patients can also join support groups with other people undergoing weight loss [25].
Family-based obesity treatment has also been proven to be a very effective and sustainable approach, especially when treating pediatric obesity. The role of this treatment is to target eating and activity change in both child and parent. Programs using this approach teach parents behavioural skills to facilitate child behaviour change and utilize family resources to improve the efficacy of childhood obesity treatments. Simultaneously treating the child and parent helps create positive relationships between them as they both aim to reach their weight loss goal together [41,42].
Pharmacotherapy
The Canadian Clinical Practice Guidelines on the Management and Prevention of Obesity in Adults and Children recommends that in addition to lifestyle modifications such as dietary changes, physical activity and behaviour therapy, overweight individuals with BMIs greater than 27 kg/m^2 but with life threatening diseases, or obese individuals with BMIs greater than 30 kg/m^2 can undergo pharmacotherapy [2].
A meta analysis investigated 21 randomized control trials (RCT) that involved a total of 11 533 participants using either one of the two drugs: orlistat or sibutramine, or a placebo. These RCTs had a follow-up period of at least 1 year in obese and overweight adults.
Olistat functions as a gastrointestinal lipase inhibitor and reduces fat absorption by approximately 30% (Figure 12). Patients can use it for up to two years [43]. On the other hand, sibutramine functions as a serotonin and noradrenaline reuptake inhibitor which induces weight loss through enhanced satiety and increased basal energy expenditure. Sibutramine is approved for clinical use for up to 1 year [44].
Pharmacotherapy trials comparing the effect of combined dietary and pharmacotherapy treatment to dietary treatment alone, showed that patients who received treatment underwent a greater weight loss compared to those who only had a reduced-energy diet. This was when orlistat or sibutramine was combined with a reduced-energy diet. More specifically, the long term weight loss for those receiving combined therapy of dietary and pharmacotherapy was about 6 to 7 kg, compared to about 2 to 3 kg for those who received dietary therapy only [26].
Maintenance of weight loss
Studies that assessed orlistat therapy for at least 2 years and up to 5 years showed that weight loss attained by year 1 was better maintained over the subsequent 3 years in patients who received ongoing drug therapy. Specifically, Davidson et al. showed that patients who had ongoing treatment of orlistat for 2 years were associated with less regain of weight loss (32%) compared with diet only therapy (63%) [45].
In addition, a 2-year study conducted by James et al., showed that 43% of patients who received 6 months of weight loss induction using diet-only therapy, followed by sibutramine-diet therapy had better maintained 80% or more of weight loss, compared to only 16% in the diet-only group who received diet-placebo therapy [46]. This shows that combined therapy is more effective than diet-only group.
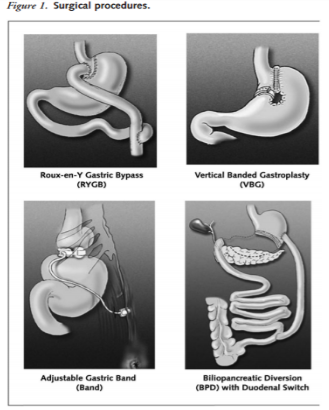
Bariatric Surgery
Bariatric surgery is a treatment method that is considered for adult patients who have a BMI over 35kg/m^2 with severe comorbid diseases such as life-threatening cardiopulmonary problems, severe sleep apnea, or severe diabetes mellitus, or for those in the severely obese category with a BMI greater than 40 kg/m2. For teenagers, the Canadian Clinical Practice Guidelines on the Management and Prevention of Obesity in Adults and Children recommends that bariatric surgery be limited to an appropriately trained and experienced surgical team. After 6 months of using lifestyle modifications, healthcare practitioners assess the health of the patient and evaluate whether a satisfactory progress of weight loss or goal of 10% of body weight has been reached. In the case that satisfactory progress or goal has not been achieved, physicians will consider the eligibility of patients to undergo bariatric surgery. This is only considered if other nonsurgical weight loss attempts have failed. The goal of bariatric surgery is to relieve a patient suffering from obesity from his or her morbid body weight, improve their comorbidity and improve their quality of life. There are different surgical procedures (Figure 13). It is important to note that this treatment option requires lifelong medical surveillance [26].
A study on obese Swedish patients investigated the conventional, nonsurgical management with surgery for morbid obesity in 2004 found that surgical management is more efficacious than medical management. Patients who received surgical treatment produced greater weight loss, improved lifestyle and dramatic improvement of comorbid disease. At 10 years of follow-up, the surgical cohort showed that they maintained a weight loss greater than 16.1% of their original body weight. In contrast, those who received the conventional, nonsurgical management had a weight gain of 1.6%. This 16.3% weight difference demonstrates the effectiveness and maintenance of surgical procedures [47].
Summary of Treatment Options
As seen in figure 14, there are different approaches to treating obesity. First, it is important to set a weight loss goal to reduce body weight by approximately 10% from baseline during the first six months of treatment. Healthcare practitioners typically recommend their patients to first undergo lifestyle modifications: proper nutrition, physical fitness, and cognitive behaviour therapy. After six months of treatment, healthcare practitioners will assess the patient’s progress and determine whether satisfactory progress or weight loss goal has been reached. In the case that it has been reached, the patient would be closely monitored on a regular basis to make sure that their weight is maintained. In the event that satisfactory progress is not attained, physicians will assess the patient’s eligibility to either undergo pharmacotherapy or bariatric surgery. Physicians typically opt for bariatric treatment in the event that nonsurgical treatments have failed. It is important to note that best weight loss and maintenance results are achieved when pharmacotherapy or bariatric treatment is used in conjunction with lifestyle modifications.
Figure 14: A holistic approach to treating obesity.
References
1. Ng, M., Fleming, T., Robinson, M., Thomson, B., Graetz, N., & Margono, C. et al. (2014). Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013.The Lancet, 384(9945), 766-781. http://dx.doi.org/10.1016/s0140-6736(14)60460-8
2. Seidell, J. & Halberstadt, J. (2015). The Global Burden of Obesity and the Challenges of Prevention. Annals Of Nutrition And Metabolism, 66(2), 7-12. http://dx.doi.org/10.1159/000375143
3. WHO: Global Database on Body Mass Index. (2017). Apps.who.int. Retrieved 1 February 2017, from http://apps.who.int/bmi/index.jsp?introPage=intro_3.html
4. Child & Teen BMI | Healthy Weight | CDC. (2017). Centers for Disease Control and Prevention. Retrieved 1 February 2017, from https://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html
5. Jitnarin, N., Poston, W., Haddock, C., Jahnke, S., & Tuley, B. (2012). Accuracy of body mass index-defined overweight in fire fighters. Occupational Medicine, 63(3), 227-230. http://dx.doi.org/10.1093/occmed/kqs213
6. Spiegelman, B. & Flier, J. (2001). Obesity and the Regulation of Energy Balance. Cell, 104(4), 531-543. http://dx.doi.org/10.1016/s0092-8674(01)00240-9
7. Pietiläinen, K., Kaprio, J., Borg, P., Plasqui, G., Yki-Järvinen, H., & Kujala, U. et al. (2008). Physical Inactivity and Obesity: A Vicious Circle. Obesity, 16(2), 409-414. http://dx.doi.org/10.1038/oby.2007.72
8. Cohen-Cole, E. & Fletcher, J. (2008). Is obesity contagious? Social networks vs environmental factors in the obesity epidemic. Journal Of Health Economics, 27(5), 1382-1387. http://dx.doi.org/10.1016/j.jhealeco.2008.04.005
9. Masuo, K. (2000). A family history of obesity, a family history of hypertension and blood pressure levels. American Journal Of Hypertension, 13(6), S164. http://dx.doi.org/10.1016/s0895-7061(00)01125-0
10. Weaver, J. (2008). Classical Endocrine Diseases Causing Obesity. Obesity And Metabolism, 212-228. http://dx.doi.org/10.1159/000115367
11. Schwartz, T., Nihalani, N., Jindal, S., Virk, S., & Jones, N. (2004). Psychiatric medication-induced obesity: a review. Obesity Reviews, 5(2), 115-121. http://dx.doi.org/10.1111/j.1467-789x.2004.00139.x
12. Dare, S., Mackay, D., & Pell, J. (2015). Relationship between Smoking and Obesity: A Cross-Sectional Study of 499,504 Middle-Aged Adults in the UK General Population. PLOS ONE, 10(4), e0123579. http://dx.doi.org/10.1371/journal.pone.0123579
13. Vermeulen, A. (2005). The epidemic of obesity: Obesity and health of the aging male. The Aging Male, 8(1), 39-41. http://dx.doi.org/10.1080/13685530500049037
14. Schumann, N., Brinsden, H., & Lobstein, T. (2014). A review of national health policies and professional guidelines on maternal obesity and weight gain in pregnancy. Clinical Obesity, n/a-n/a. http://dx.doi.org/10.1111/cob.12062
15. Why Is Sleep Important? - NHLBI, NIH. (2017). National Heart, Lung and Blood Institute. Retrieved 1 February 2017, from https://www.nhlbi.nih.gov/health/health-topics/topics/sdd/why
16. Gurevich-Panigrahi, T., Panigrahi, S., Wiechec, E., & Los, M. (2009). Obesity: pathophysiology and clinical management. Current Medical Chemistry, 16, 506-521. Retrieved from http://liu.diva-portal.org/smash/get/diva2:583167/FULLTEXT01.pdf
17. Odegaard, J., & Chawla, A. (2012). Adipose tissue metabolism in the obese. TheScientist. Retrieved 18 January 2017, from http://www.the-scientist.com/?articles.view/articleNo/33653/title/adipose-tissue-metabolism-in-the-obese/
18. Kahn, B. B., & Flier, J. S. (2000). Obesity and insulin resistance. Journal of Clinical Investigation, 106(4), 473–481.
19. Després, J., & Marette, A. (1999). Obesity and Insulin Resistance. Insulin Resistance, 51-81. doi:10.1007/978-1-59259-716-1_4
20. Klok, M. D., Jakobsdottir, S., & Drent, M. L. (2007). The role of leptin and ghrelin in the regulation of food intake and body weight in humans: a review. Obesity Reviews, 8(1), 21-34. doi:10.1111/j.1467-789x.2006.00270.x
21. Kaszmi, A., Sattar.A., Hashim, R., Khan., S.P.., Younus, M., Khan, F.A. (2013). Serum Leptin values in the healthy obese and non-obese subjects of Rawalpindi. J Pak Med Assoc. 63(2), 245-8
22. Tschop, M., Weyer, C., Tataranni, P. A., Devanarayan, V., Ravussin, E., & Heiman, M. L. (2001). Circulating Ghrelin Levels Are Decreased in Human Obesity. Diabetes, 50(4), 707-709. doi:10.2337/diabetes.50.4.707
23. Walley, A.J., Blakemore, A.I.F. & Froguel, P. (2006). Genetics of obesity and the prediction of risk for health. Human Molecular Genetics. Retrieved 27January, 2017, from https://academic.oup.com/hmg/article/15/suppl_2/R124/626082/Genetics-of-obesity-and-the-prediction-of-risk-for
24. Rankinen, T., Zuberi, A., Chagnon, Y.C., Weisnagel, S.J., Argyropoulos, G., Walts, B., Perusse, L., & Bouchard, C. (2006). The human obesity gene map: the 2005 update. Obesity, 14(4), 529-644.
25. Pi-Sunyer, F. X., Becker, D. M., Bouchard, C., Carleton, R. A., Colditz, G. A., Dietz, W. H., … & Higgins, M. (1998). Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. American Journal of Clinical Nutrition, 68(4), 899-917.
26. Lau, D. C., Douketis, J. D., Morrison, K. M., Hramiak, I. M., Sharma, A. M., Ur, E., & members of the Obesity Canada Clinical Practice Guidelines Expert Panel. (2007). 2006 Canadian clinical practice guidelines on the management and prevention of obesity in adults and children [summary]. Canadian Medical Association Journal, 176(8), S1-S13.
27. Poirier, P., & Després, J. P. (2001). Exercise in weight management of obesity. Cardiology clinics,19(3),459-470.
28. Hey, H., Petersen, H. D., Andersen, T., & Quaade, F. (1987). Formula diet plus free additional food choice up to 1000 kcal (4.2 MJ) compared with an is energetic conventional diet in the treatment of obesity. A randomised clinical trial. Clinical Nutrition,6(3),195-199.
29. Lau, D. C., Douketis, J. D., Morrison, K. M., Hramiak, I. M., Sharma, A. M., Ur, E., & members of the Obesity Canada Clinical Practice Guidelines Expert Panel. (2007). 2006 Canadian clinical practice guidelines on the management and prevention of obesity in adults and children [summary]. Canadian Medical Association Journal, 176(8), S1-S13.
30. Toubro, S., & Astrup, A. (1997). Randomised comparison of diets for maintaining obese subjects' weight after major weight loss: ad lib, low fat, high carbohydrate diet fixed energy intake. Bmj,314(707329.
31. 9 Popular Weight Loss Diets Reviewed by Science. (2016, October 04). Retrieved January 27, 2017, from https://authoritynutrition.com/9-weight-loss-diets-reviewed/
32. Poirier, P., & Després, J. P. (2001). Exercise in weight management of obesity. Cardiology clinics, 19(3), 459-470.
33. Tremblay, A., Nadeau, A., Despres, J. P., St-Jean, L., Theriault, G., & Bouchard, C. (1990). Long-term exercise training with constant energy intake. 2: Effect on glucose metabolism and resting energy expenditure. International journal of obesity, 14(1), 75-84.
34. Gwinup, G. (1987). Weight loss without dietary restriction: efficacy of different forms of aerobic exercise. The American journal of sports medicine, 15(3), 275-279.
35. Pate, R. R., Pratt, M., Blair, S. N., Haskell, W. L., Macera, C. A., Bouchard, C., … & Kriska, A. (1995). Physical activity and public health: a recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. Jama, 273(5), 402-407.
36. Nozaki, T., Sawamoto, R., & Sudo, N. (2013). Cognitive behavioral therapy for obesity. Nihon rinsho. Japanese journal of clinical medicine, 71(2), 329-334.
37. Cooper, Z., Fairburn, C. G., & Hawker, D. M. (2003). Cognitive-behavioral treatment of obesity: A clinician's guide. Guilford Press.
38. Diabetes Prevention Program (DPP) Research Group. (2002). The diabetes prevention program (DPP). Diabetes care, 25(12), 2165-2171.
39. Look AHEAD Research Group. (2003). Look AHEAD (Action for Health in Diabetes): design and methods for a clinical trial of weight loss for the prevention of cardiovascular disease in type 2 diabetes. Controlled clinical trials,24(5), 610-628.
40. Renjilian, D. A., Perri, M. G., Nezu, A. M., McKelvey, W. F., Shermer, R. L., & Anton, S. D. (2001). Individual versus group therapy for obesity: effects of matching participants to their treatment preferences. Journal of consulting and clinical psychology, 69(4), 717.
41. Wrotniak, B. H., Epstein, L. H., Paluch, R. A., & Roemmich, J. N. (2004). Parent weight change as a predictor of child weight change in family-based behavioral obesity treatment. Archives of pediatrics & adolescent medicine, 158(4), 342-347.
42. Epstein, L. H., Roemmich, J. N., Stein, R. I., Paluch, R. A., & Kilanowski, C. K. (2005). The challenge of identifying behavioral alternatives to food: clinic and field studies. Annals of Behavioral Medicine, 30(3),201-209
43. Guerciolini, R. (1997). Mode of action of orlistat. International journal of obesity and related metabolic disorders: journal of the International Association for the Study of Obesity, 21, S12-23.
44. Finer, N. (2002). Sibutramine: its mode of action and efficacy. International Journal of Obesity, 26(S4), S29.
45. Davidson, M. H., Hauptman, J., DiGirolamo, M., Foreyt, J. P., Halsted, C. H., Heber, D., … & Heymsfield, S. B. (1999). Weight control and risk factor reduction in obese subjects treated for 2 years with orlistat: a randomized controlled trial. Jama, 281(3), 235-242.
46. James, W. P. T., Astrup, A., Finer, N., Hilsted, J., Kopelman, P., Rössner, S., … & STORM Study Group. (2000). Effect of sibutramine on weight maintenance after weight loss: a randomised trial. The Lancet, 356(9248), 2119-2125
47. Sjöström, L., Lindroos, A. K., Peltonen, M., Torgerson, J., Bouchard, C., Carlsson, B., … & Sullivan, M. (2004). Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. New England Journal of Medicine, 351(26), 2683-2693.