Table of Contents
Global Burden of Disease: Lower Respiratory Infections (LRI)
Lower Respiratory Infections (LRI) Powerpoint
Introduction
Global Burden of Disease
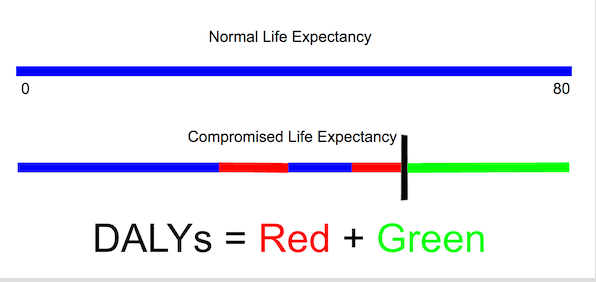
The global burden of disease measures the burden of a specific disease using the disability-adjusted-life-year (DALY) measurement. This measure combines the years of life lost due to premature mortality and the years of life lost due to time lived in states of less than full health.
Lower respiratory tract infections (LRTIs) are one of the prevalent and troublesome diseases around the world. There are numerous different types of LRTIs, but the most common ones are pneumonia and bronchitis.
LRTIs are one of the most frequent reasons for pediatric visits and hospitalization for children. (El-Azami-El-Idrissi et al., 2016). Also, males are more susceptible than females for LRTIs (Falagas, Mourtzoukou, & Vardakas, 2007).
Epidemiology
According to the World Health Organization (n.d.), LRTIs account for the second largest global burden of disability-adjusted life years (DALYs) in 2012. Since 2000, the global burden associated with LRTI has decreased by nearly 30% (WHO, n.d.). Unfortunately, roughly 95% of the episodes of childhood clinical pneumonia occur in developing nations (Rudan, Boschi-Pinto, Biloglav, Mulholland, & Campbell, 2008). In addition, it is estimated that childhood pneumonia is the single leading cause of childhood mortality (Rudan, Boschi-Pinto, Biloglav, Mulholland, & Campbell, 2008).
Unfortunately, Canada is not immune to the detrimental impact of LRTIs. In fact, Inuit infants within Canada have some of highest hospital admissions as a result of LRTIs in the entire world (Kovesi et al., 2007). More specifically, a recent study found that the annualized incidence rate of admission to hospital for LRTI for a particular Inuit population located on Baffin Island was 484 per 1000 infants under the age of 6 months (Banerji et al., 2001). After extensive research, it was determined that indoor air pollution, reduced ventilation, and overcrowding within a household are all risk factors associated with LRTI that are prevalent in most Inuit communities in Canada (Kovesi et al., 2007).
Pathophysiology
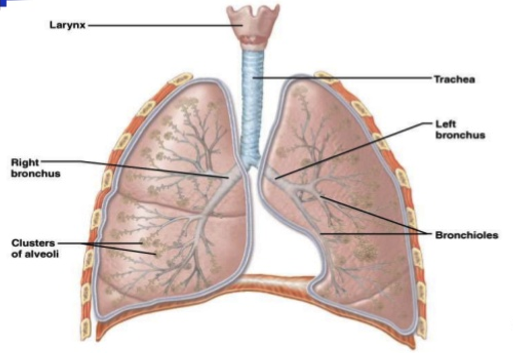
Lower respiratory system anatomy
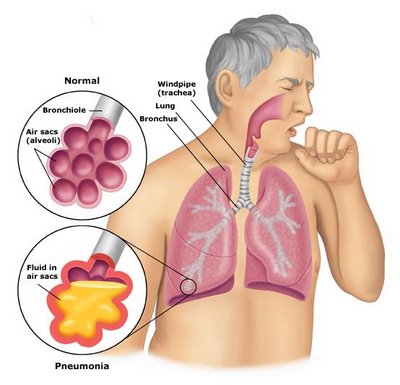
The lower respiratory system consists of the trachea, the bronchi and bronchioles and the alveoli which make up the lungs (Medicine plus, 201). The trachea, which is the largest tube in the respiratory tract, branches off into two bronchial tubes known as bronchus. The tubes of the bronchi branch subdivide further into secondary and tertiary bronchi and then into bronchioles. The ends of the bronchioles give rise to microscopic air sacs known as alveoli. Hundreds of alveoli exist inside each lung (Medicine plus, 201).
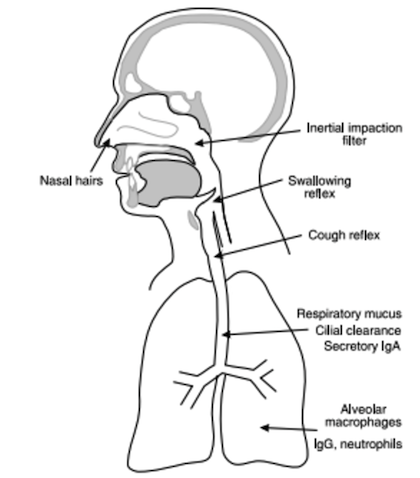
The primary function of the respiratory system is to exchange oxygen and carbon dioxide between the body and environment, and it takes place in the alveoli, also known as air sacs found in the lungs (Inglis, 2007). Therefore, the respiratory tract is constantly exposed to microorganisms such as bacteria, viruses, and fungi. The majority of particles are filtered out in the nasal hairs and by the inertial impaction, which is covered by mucus found in the posterior nasopharynx. The epiglottis applies a closure and cough reflex to reduce the risk of microorganisms reaching the lower respiratory tract. However, if small enough particles have reached the trachea and bronchi they then stick to the respiratory mucus lining their walls and are propelled towards the oropharynx by the cilia. Then, antimicrobial factors such as lysozyme, lactoferrin and secretory IgA present in respiratory secretions disable inhaled microorganisms from reaching further into the lungs (Inglis, 2007).
However, particles ranging from about 5-10 µm may be able to get further into the respiratory system into the alveolar air sacs (Inglis, 2007). Once they reach the alveolar air sacs, the alveolar macrophages phagocytose the pathogens, and the neutrophils may also be activated through the inflammatory response (Inglis, 2007).
Causes of LRI
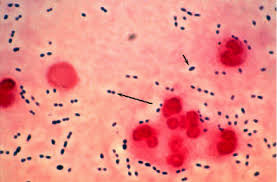
Nevertheless, pathogens have developed strategies to overcome the defense mechanisms in the respiratory system. For example, Streptococcus pneumonia, a gram-positive bacteria, and Haemophilus influenzae, a gram-negative bacteria both produce an enzyme known as IgA protease, which is capable of disabling mucosal IgA (Inglis, 2007). Streptococcus pneumonia and Haemophilus influenzae which are primarily known to cause pneumonia, in addition to other bacteria are resistant to phagocytosis. Therefore, they are able to get passed the defense mechanisms and penetrate to the lungs. Some microorganisms also release toxins which can cause further damage to the alveolar walls (Inglis, 2007).
Pneumonia can develop after inhalation of microorganisms primarily bacteria, viruses, and fungi or when bacteria from an infection elsewhere in the body spreads to the lungs, which overpower your immune system, thus infecting your lungs (Mayo Clinic, 2016). It is characterized by inflammation of the air sacs or alveoli, which are microscopic sacs in the lungs that absorb oxygen. The inflammation causes the alveoli to fill with fluid reducing the amount of air space in the lungs for air, and so the air coming is unable to exchange (Mayo Clinic, 2016).
Community and Hospital Acquired Pneumonia
Community-acquired pneumonia (CAP) is the most common type of pneumonia, which occurs outside of the hospital setting. It is caused by bacteria, fungi, and viruses. The most common cause of bacterial pneumonia is streptococcus pneumonia, and it usually occurs on its own or after having a cold or flu. Pneumonia caused by fungi is common in people with weak immune systems or chronic health problems and in those who have inhaled large doses of the organism. Viruses that cause cold and flu can cause pneumonia as well. Also, viruses are the most common case of pneumonia in children (Mayo Clinic, 2016). Pneumonia occurring during a hospital stay for another illness is termed hospital-associated pneumonia (HAP). It is mostly caused by a bacteria then by a virus.The bacteria causing the pneumonia may become resistant to antibiotics, making it dangerous.
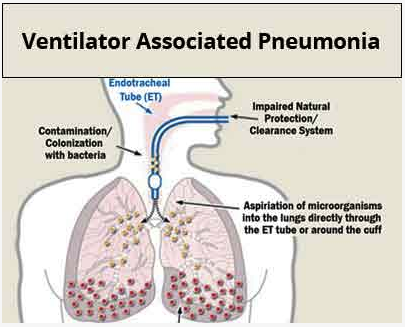
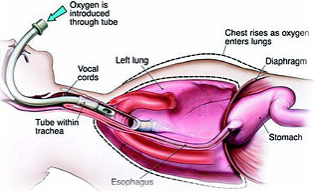
Ventilator-associated pneumonia is a type of HAP, which occurs in patients receiving mechanical ventilation through an endotracheal tube or tracheostomy (Amanullah, 2015). Thus, the mechanical ventilation increases the risk of developing bacterial pneumonia because it allows free passage of bacteria into the lower segments of the lung through the endotracheal tube and around the cuff which then enters the lungs with each breath (Amanullah, 2015).
Symptoms
The symptoms of pneumonia can vary from mild to severe. Many of the mild symptoms are very similar to that of a cold. However, they would last longer. Some of the symptoms of pneumonia may include; cough (some may cough up greenish or yellow mucus or bloody mucus) , nausea and vomiting, shortness of breath, chest pain which gets worse when you breath deeply or a cough, rapid breathing, shaking chills and fever which may be mild or high (Mayo Clinic, 2016);(American Lung Association, 2016).
Diagnosing CAD
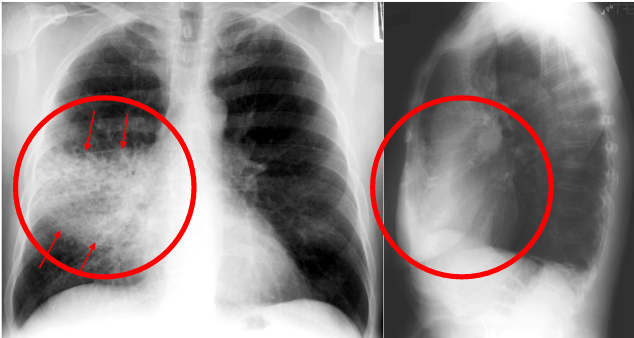
The first indication of lower respiratory tract infections is due to a recurring cough and chest irritation which does not stop after a short period of time. A physician will typically suspect an LTRI if the patient exhibits unusual wheezing or sound in the lungs (Mayo Clinic, 2014). The most important distinction to make when diagnosing an LTRI is to differentiate between a pneumonic and non-pneumonic condition. This will be important in helping to determine the course of treatment and severity of the infection. The main method of diagnosis without a chest radiograph is to focus on the category of symptoms (Anderson & Winter, 2009).
Physicians rely on other tests as will, such as painless skin monitoring to determine if the oxygen concentration in the patient's blood is lower than normal. Furthermore, blood tests can be performed to check for an elevated white blood cell count which would indicate a reaction to a virus, bacteria or another pathogen. The most popular method of diagnosing an LTRI, specifically pneumonia is a chest x-ray to check for the presence of fluid in the air-filled sacs (Mayo Clinic, 2014). The X-ray assists physicians in ruling out other causes of the symptoms such as acute bronchitis or a lung mass.
Interestingly, the practice guidelines of the American Thoracic Society (AST) and the Infectious Disease Society of America (IDSA) places emphasis on using patient's history and physical examination for diagnosis (Carrol, 2002). Lastly, microbiological tests have seen an increase in use due to the ease and accuracy of the tests performed. They require collection of sputum, which is a mixture of saliva and mucus coughed up from the respiratory tract. For example, Streptococcus pneumoniae, the bacteria which causes pneumonia is tested for by performing gram stains and cultures. Also, bacterial urinary antigen tests are available as they are highly specific and sensitive (Carrol, 2002). Overall, physicians rely on traditional methods for diagnosis of the disease, although laboratory tests are favored for their accuracy and ease of specimen collection.
Risk Factors
Physiological Risk Factors
Although individuals of all ages can develop pneumonia, age is a factor that influences both an individual’s likelihood of acquiring pneumonia and the severity of pneumonia that develops (NHLBI, 2016). The groups with the greatest risk are individuals under the age of two or over the age of sixty-five (NHLBI, 2016). Infants are more susceptible because their immune systems are still developing, and the elderly are more susceptible because their immune systems weaken as they undergo normal aging processes (NHLBI, 2016).
Individuals can also have a higher risk of developing pneumonia if they have had a recent viral respiratory infection (such as a cold or flu), or if they have a chronic lung or other serious disease such as cystic fibrosis, COPD, diabetes, or sickle cell disease (Healthline, 2015). Diseases such as these increase risk because they make breathing difficult, block airways, and have symptoms that are similar to and can be exacerbated by pneumonia (Healthline, 2015). In addition, individuals with these diseases may also be prescribed immunosuppressant drugs such as inhaled corticosteroids (Healthline, 2015). Having a cold or flu can cause bacterial pneumonia to develop on its own, most commonly from the Streptococcus pneumoniae bacteria (Mayo Clinic, 2016).
Lifestyle Risk Factors
There are many lifestyle-related habits that can influence an individual’s risk of developing pneumonia. In healthy young individuals, smoking cigarettes is the largest risk factor for developing pneumonia (NHLBI, 2016). Alcohol abuse can also increase an individual’s chance of developing pneumonia because long-term alcohol use lowers levels of the white blood cells that can fend off pneumonia (NHLBI, 2016). Other conditions, such as having HIV/AIDS, an organ or blood/marrow transplant, chemotherapy, or long-term steroid use all increase risk as well, as they weaken or suppress the immune system (NHLBI, 2016). Being undernourished can also increase risk levels for the same reason (NHLBI, 2016).
Risk can also be increased if an individual is regularly exposed to chemicals, pollutants, or fumes (WHO, 2016). Indoor air pollution caused by cooking, asbestos, or heating using biomass fuels (wood, dung) can both increase risk (WHO, 2016). Air pollution in the form of second-hand smoke can also increase an individual’s risk of developing pneumonia (WHO, 2016). Fungal-based pneumonia can also develop if an individual is frequently exposed to fungi found in bird droppings or soil (Mayo Clinic, 2016).
Healthcare Factors
Individuals may develop pneumonia while in the hospital because they have a weakened immune system and may be on immunosuppressant medication (Mayo Clinic, 2016). Hospital-acquired pneumonia can be especially dangerous because the bacteria involved may be more resistant to antibiotics because the patient is already sick (Mayo Clinic, 2016). Individuals using ventilators, which are often used in intensive care units, are at a higher risk of developing this type of pneumonia (Mayo Clinic, 2016). Bacterial pneumonia can also occur in healthcare settings such as outpatient clinics, kidney dialysis centers, and long-term care facilities (Mayo Clinic, 2016).
Treatments
The treatments for pneumonia can be categorized into lifestyle modifications, pharmacological options, and medical procedures.
Lifestyle Modifications
Lifestyle modifications are important in the prevention and treatment of pneumonia. Pneumonia can be prevented through various vaccinations. A vaccination can be administered to prevent pneumococcal pneumonia, which is a common form of bacterial pneumonia (National Heart, Lung, and Blood Institute, 2016). Since pneumonia is commonly caused by the seasonal influenza, it is important to be vaccinated against it. Moreover, it is crucial to quit smoking as the tobacco damages the lung’s ability to fight off infection (National Heart, Lung, and Blood Institute, 2016). Healthy eating and regular exercise is important in keeping a strong immune system to effectively fight infections.
Pharmacological Options
In the early stages of pneumonia, managing symptoms is equally important as curing pneumonia. Coughing is one of the body’s mechanisms to eliminate infection through the movement of mucus. Therefore, cough medications should be avoided, as they will suppress coughing. To relieve coughing, home remedies such as chewing garlic with honey can be implemented. Furthermore, drinking plenty of fluids will complement the treatment of pneumonia, as it will help loosen secretions and dilute phlegm. The type of pharmacological treatment used to cure pneumonia depends on the type and severity of pneumonia. The goal of medications is to cure the respiratory infection and prevent complications. Pneumonia caused by bacteria is treated with antibiotics like azithromycin, clarithromycin and erythromycin (National Heart, Lung, and Blood Institute, 2016). These antibiotics bind to the bacterial 50S subunit to inhibit peptidyl transferase activity and they interfere with the translocation of amino acids during translation and the assembly of proteins (DrugBank, 2005). This prevents regular bacterial growth. These antibiotics improve symptoms in one to three days. It is important to take antibiotics as prescribed by the doctor to completely eliminate the infection and prevent its reoccurrence. One limitation with using antibiotics is that it can be ineffective towards antibiotic resistant bacteria. Furthermore, pneumonia caused by a virus is treated with antiviral drugs such as oseltamivir (National Heart, Lung, and Blood Institute, 2016). Oseltamivir inhibits influenza virus neuraminidase by altering virus particle aggregation and release (DrugBank, 2005). This drug improves symptoms within one to three weeks.
Medical Procedures
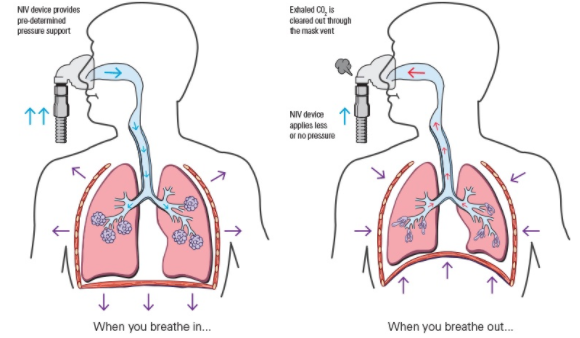
In very serious cases, oxygen therapy may be used to facilitate breathing with a non-invasive ventilation or invasive ventilation. A non-invasive ventilator provides oxygen support to a patient through a tightly fitted facial or nasal mask to improve breathing. A study tested the effectiveness of noninvasive ventilation in treating pneumonia. It concluded that the use of ventilation significantly reduced respiratory rate and the duration of stay in the intensive care unit (ICU) (Confalonieri et al., 1999). Some side effects with this therapy include dry or bloody nose, tiredness and morning headaches (Zhang et al., 2012). Whereas, an invasive ventilator provides oxygen through a tube inserted into the trachea through the mouth or the nose. As compared to the non-invasive ventilation, invasive ventilation has a higher infection risk and increased bleeding. Both ventilation methods provide a larger tidal volume with the same inspiratory effort, thus improving alveolar ventilation and decreasing the work of breathing (Zhang et al., 2012). It allows increased oxygen concentrations in the lungs, which is then delivered to the blood. To complement the oxygen therapy, antibiotics and fluids are delivered intravenously through a drip.
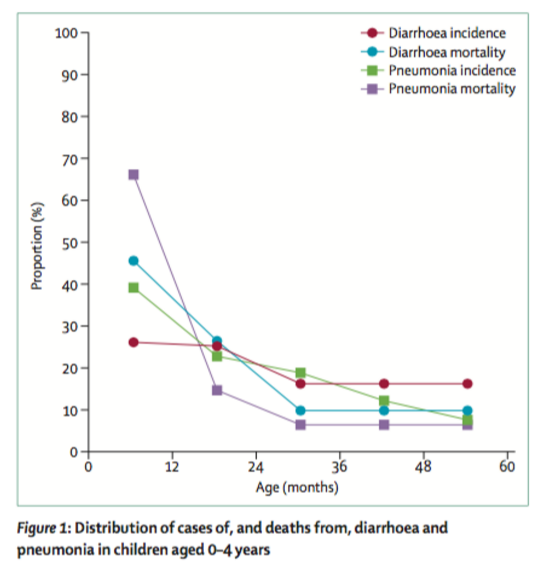
Future Global Burden
As indicated earlier, LTRs were the second highest global burden of disease in 2012 and this number is comprised of many cases of childhood pneumonia. A large scale, systematic literature review conducted in 2013 studied the Global Burden of Childhood Pneumonia and Diarrhea. The results were divided based on global and regional burden and burden by age and number. The authors found incidence and case-related fatality ratios were higher in low and middle income families, suggesting economic status played a large role in disease determinance. As seen in the below figure, younger age groups (0-2 years) currently make up 81% of the youth lives lost to pneumonia. Studies have found that currently, the greatest burden of disease for childhood pneumonia is in Southeast Asia and Africa due to poor hygienic conditions, malnutrition, and sub-optimal breast-feeding (which prevents children from acquiring passive immunity). As of now, 15 developing countries contribute to 64% of total global cases of pneumonia. Lastly, nearly ⅓ severe diarrhoea and pneumonia cases are vaccine-preventable suggesting the need for political and societal intervention. Although the burden of childhood pneumonia is expected to decrease in the future, largely due to increasing awareness and better healthcare facilities, action is required immediately on a global scale to actively reduce the prevalence of this mostly preventable illness.
References
Amanullah. (2015).Ventilator-Associated Pneumonia Overview of Nosocomial Pneumonias. Retrieved from http://emedicine.medscape.com/article/304836-overview
American Lung Association. (2016). Pneumonia symptoms, causes and Risk Factors. Retrieved from: http://www.lung.org/lung-health-and-diseases/lung-disease-lookup/pneumonia/symptoms-causes-and-risk.html?referrer=https://www.google.ca/
Anderson, W., & Winter, J. (2009). Managing LRTI in adults in the community. The Practitioner, 253(1723), 21-26.
Banerji, a, Bell, a, Mills, E.L., McDonald, J., Subbarao, K., Stark, G., Eynon, N., and Loo, V.G. (2001). Lower respiratory tract infections in Inuit infants on Baffin Island. CMAJ 164, 1847–1850
Carroll, K. C. (2002). Laboratory diagnosis of lower respiratory tract infections: controversy and conundrums. Journal of clinical microbiology, 40(9), 3115-3120.
Confalonieri, M., Potena, A., Carbone, G., Porta, R., Tolley, E., & Meduri, U. (1999). Acute Respiratory Failure in Patients with Severe Community-acquired Pneumonia. ATS Journals, 160(5), 1585-1591.
DrugBank. (2005, June 23). Pharmacology . Retrieved from https://www.drugbank.ca/drugs/DB01211
El-Azami-El-Idrissi, M., Lakhdar-Idrissi, M., Chaouki, S., Atmani, S., Bouharrou, A., & Hida, M. (2016). Pediatric recurrent respiratory tract infections: When and how to explore the immune system? (About 53 cases). Pan African Medical Journal, 24. http://doi.org/10.11604/pamj.2016.24.53.3481
Falagas, M. E., Mourtzoukou, E. G., & Vardakas, K. Z. (2007). Sex differences in the incidence and severity of respiratory tract infections. Respiratory Medicine. http://doi.org/10.1016/j.rmed.2007.04.011
Healthline. 2015. Bacterial Pneumonia: Risk Factors. Retrieved from: http://www.healthline.com/health/bacterial-pneumonia#Overview1. Inglis, T. J. J. (2007). Microbiology and infection: a clinical core text for integrated curricula with self-assessment. Elsevier Health Sciences
Kovesi, T., Gilbert, N. L., Stocco, C., Fugler, D., Dales, R. E., Guay, M., & Miller, J. D. (2007). Indoor air quality and the risk of lower respiratory tract infections in young Canadian Inuit children. CMAJ : Canadian Medical Association Journal = Journal de l’Association Medicale Canadienne, 177(2), 155–60. http://doi.org/10.1503/cmaj.061574
Mayo Clinic. (2016). Pneumonia. Retrieved from: http://www.mayoclinic.org/diseases-conditions/pneumonia/symptoms-causes/dxc-20204678
Mayo Clinic. (2014). Respiratory Syncytial virus (RSV) Test and Diagnosis. Retrieved from: http://www.mayoclinic.org/diseases-conditions/respiratory-syncytial-virus/basics/tests-diagnosis/con-20022497
Mayo Clinic. 2016. Symptoms and causes of Pneumonia. Retrieved from: http://www.mayoclinic.org/diseases-conditions/pneumonia/symptoms-causes/dxc-20204678
Medicine Plus. (2017).Lower respiratory tract. Retrieved from: https://medlineplus.gov/ency/imagepages/19379.htm
National Heart, Lung, and Blood Institute. (2016, October 12). Pneumonia. Retrieved from https://www.nhlbi.nih.gov/health/health-topics/topics/oxt
National Heart, Lung, and Blood Institute (NHLBI). 2016. Risk Factors: Pneumonia. Retrieved from: https://www.nhlbi.nih.gov/health/health-topics/topics/pnu/atrisk.
Rudan, I., Boschi-Pinto, C., Biloglav, Z., Mulholland, K., & Campbell, H. (2008). Epidemiology and etiology of childhood pneumonia. Bulletin of the World Health Organization. http://doi.org/10.2471/BLT.07.048769
Walker, C. L. F., Rudan, I., Liu, L., Nair, H., Theodoratou, E., Bhutta, Z. A., … & Black, R. E. (2013). Global burden of childhood pneumonia and diarrhoea. The Lancet, 381(9875), 1405-1416.
World Health Organization. (n.d.). Estimates for 2000-2012: Disease Burden. Retrieved from: http://www.who.int/healthinfo/global_burden_disease/estimates/en/index2.html
World Health Organization (WHO). 2016. Pneumonia Fact Sheet. Retrieved from: http://www.who.int/mediacentre/factsheets/fs331/en/. Zhang Y, Fang C, Dong BR, Wu T, Deng JL. (2012). Oxygen therapy for pneumonia in adults. Cochrane Database of Systematic Reviews, 3.