This is an old revision of the document!
Table of Contents
INTRODUCTION TO ASTHMA
Asthma is a chronic inflammatory disease that leads to the constriction of the airways, as well as, airway hyperresponsiveness (Keller, 2002). Approximately 300 million people are affected worldwide and this number is expected to rise over the upcoming years (Lambecht & Hammad, 2015). As well, approximately 250,000 people die annually (Pawankar, 2014). Asthma most commonly affects infants (Reed, 2006). Reed (2006), found that babies in their first year of life had a 3% likelihood of developing asthma. This incidence rate drops to 0.9% for 1-4 year olds (Reed, 2006). Due to this, most of research is focused on the development of asthma in children as opposed to adults or seniors (Reed, 2006). Asthma can be divided into allergic asthma and non-allergic asthma. Allergic asthma is mostly commonly found in children, but are also found in 50% of adults (Lambrecht & Hammad, 2015). In children, the disease begins with allergic sensitization, which involves the interaction between the IgE antibody present in the body, and the inhaled or ingested allergin (such as dust mites, pollen) (Lambrecht & Hammad, 2015). This interaction leads to a cascade of allergic reactions, and is accompanied by atopic eczema in the early stages of life (Lambrecht & Hammad, 2015). In later life, these children develop allergic rhinitis, which leads to the progression of the disease. (Lambrecht & Hammad, 2015). Non-allergic asthma occurs later in life and does not involve an interaction between IgE antibodies and the allergen (allergic sensitization) (Lambrecht & Hammad, 2015). Non-allergic asthma is most commonly found in women (Lambrecht & Hammad, 2015). This form of asthma is more difficult and takes a longer time to treat (Lambrecht & Hammad, 2015). It also leads to chronic rhinosinusitis, nasal polyps as well as obesity (Lambrecht & Hammad, 2015).
EPIDEMIOLOGY
The prevalence of asthma varies worldwide (Keller, 2002). However, developed countries, such as Canada, Unites States, and Australia, have the highest prevalence rates of asthma (Keller, 2002). The world is exhibiting an increase in rates of this illness among all variables: age, gender and racial groups (Keller, 2002). As a result, it is leading to more deaths, and higher economic costs for countries (Keller, 2002). In the United States, there was a 75% increase in prevalence of asthma observed between 1980 and 1994, in which, greater increases were found in children and young adults (Keller, 2002). The prevalence of asthma in the United States is much higher than most other countries in the world, but drastically varies among ethnic groups (Gold & Wright, 2005). However, it has been speculated that this increase may be due to greater public awareness and improvements in detecting the disease in earlier stages (Keller, 2002).
RISK FACTORS
There are several factors that make one more prone to this disease:
- Heredity:A toddler has an 80 - 90% chance of contracting this illness if both parents are asthmatic, however, if one parent has the disease, then the toddler would be 30 - 40% at risk of contracting the illness (Duffy, 1997). There are several studies that looked at monozygotic and dizygotic twins and found that monozygotic twins have a 19% chance of presenting with the same disease, whereas dizygotic twins only have a 4.8% chance of presenting with the same disease (Edfors-Lubs, 1971). An individual with a family history of this disease is four times as likely of getting the disease (Ronmark et al., 1971).
- Fetal environment: Studies have found a relationship between the fetal environment and the development of the atopic disease later in life (Keller, 2002). It is more likely for the child to contract the disease if the mother has the disease as opposed to the father having it(Keller, 2002). The risk for a child to develop asthma in later life has been correlated with a mother’s exposure to allergins in the first 22 weeks of gestation (Warner et al., 2000). Bronchial hyperresponsiveness has been shown to be more commonly found in infants with lower birthweight as opposed to infants with a higher birthweight (Keller, 2002). Moreover, It has been found that mothers who smoke and are younger than 20 years, were more likely to have a child who suffers from asthma (Keller, 2002). Moreover, maternal prenatal stress has also shown to be a possible risk factor for developing asthma (Sears, 2014). Research also has looked at the relationship between different modes of delivery and the likelihood of developing asthma. It was found that mothers who had undergone a caesarean section, were 10% to 20% more likely at risk to have an asthmatic child (Sears, 2014).
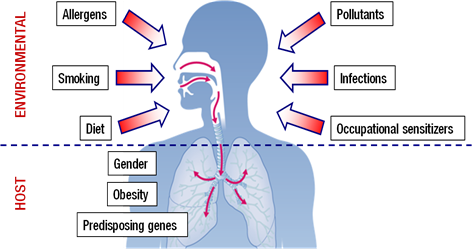
- Environmental Factors:There are several environmental and genetic determinants for Asthma, that interact together to form a genetic-environmental interface (Keller, 2002). Firstly, environmental exposures to allergens early in life can raise the risk of allergy in later life and increase the incidence for developing asthma (Keller, 2002). Infants who develop this disease later in life usually have an unbalanced immune system (Keller, 2002). In order to reduce an individual’s risk of developing asthma, they must ensure that they are living in a clean environment, and following a hygienic lifestyle (Keller, 2002). The overuse and misuse of medications such as antibiotics has also shown to increase the likelihood of developing this disease in children, by disrupting the normal development of the immune system (Keller, 2002). Moreover, research has also shown that diets low in Omega 3, vitamin C and high in fat has been linked to the development of asthma (Weiss, 1997). An indoor and sedentary lifestyle, which is typically seen in urban environments, can increase this likelihood as well (Keller, 2002). Exercise and an active lifestyle is essential for reducing an individual's risk of getting asthma (Keller, 2002). Studies have shown that exercise has the potential in protecting against wheezing illnesses which are attributed to the development of asthma (Skloot, 1995).
Figure: Asthma Risk Factors
PATHOGENESIS
What initiates the inflammatory process in the first place is still being investigated. However, new observations suggest that the origins of asthma occurs early in life. The expression of asthma is a complex, interactive process that depends on the interplay between two major factors—host factors (particularly genetics) and environmental exposures (that occur at a crucial stage in the development of the immune system) (National Heart, Lung, and Blood Institute 2007).
PATHOPHYSIOLOGY
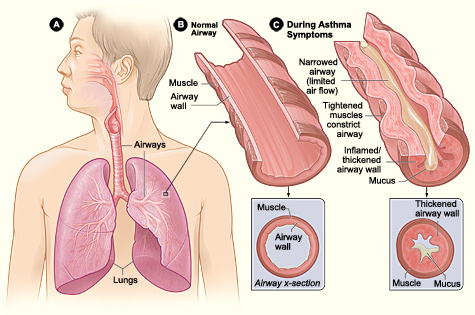
In general, Asthma is a chronic disease of the respiratory system involving: bronchoconstriction- narrowing of airway, overdeveloped mucous glands, airway thickening/bronchial inflammation, obstruction of the air flow and wheezing and shortness of breath (Cohn et al. 2004). It is a complex interplay and is the resultant of the combined effect of many cells and signals that will be discussed below.
Figure: Difference between normal and pathophysiological bronchiole. Shows tightened muscles which constrict airway, mucus accumulation, thickened airway wall. As a result, there’s a narrow airway and limited airflow.
The Normal Physiological Response
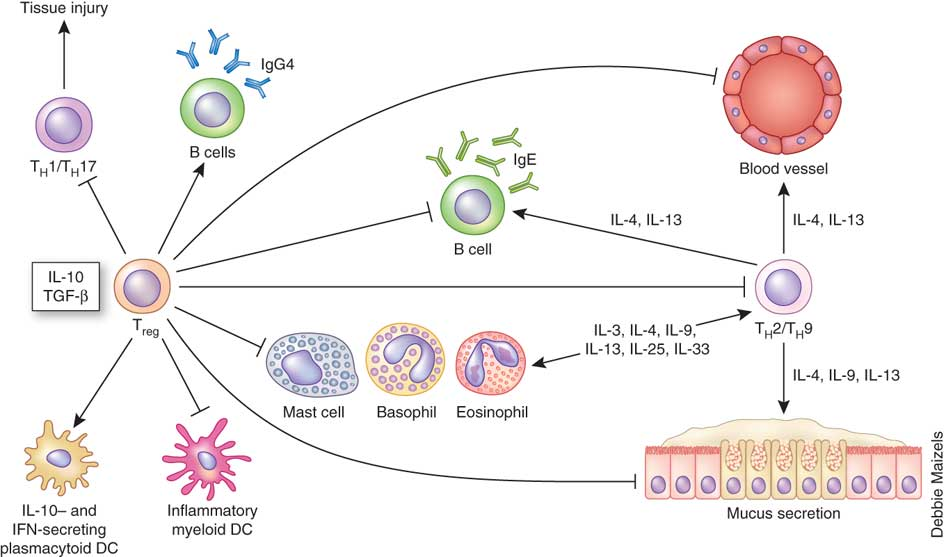
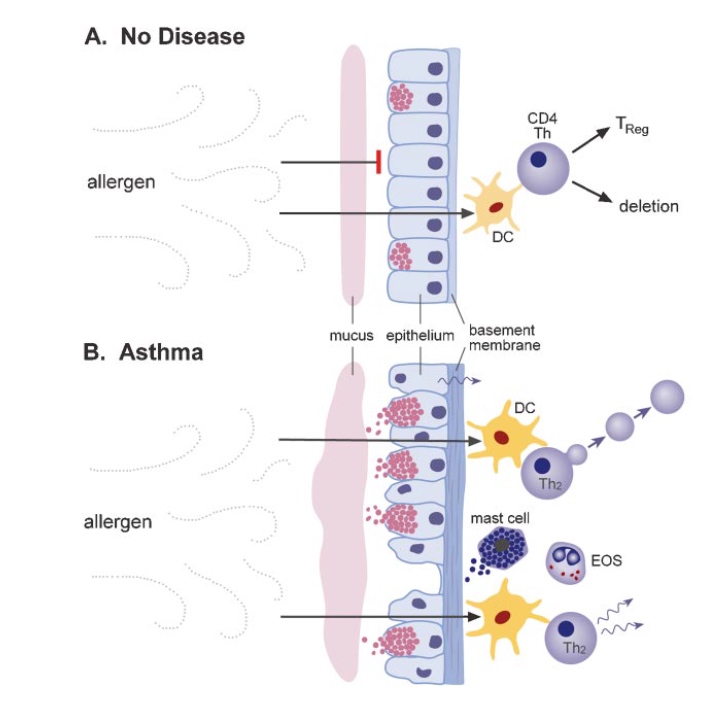
Normally airborne antigens are sampled by antigen presenting cells (i.e. dendritic cells) at the bronchial mucosa. The barrier function of the mucosa remains intact via tight junctions and ensures mucociliary clearance. Treg cells induce self tolerance and suppress allergy and immune response. Treg cells are non-inflammatory regulatory T cells which help mediate immunological tolerance. Treg cells secrete IL-10 or TGF-beta signals (Cohn et al. 2004).
T reg cells inhibit dendritic cells, inhibit T cells which promote inflammation of airway and bronchoconstriction, inhibit B cells from producing IgE which leads to inflammation caused by histamine production, and inhibit mast cells, eosinophils and basophils which cause inflammation and mucous via histamine and prostaglandin release. Overall this helps suppress the overall inflammation and bronchoconstriction in the pathophysiological asthmatic response (Cohn et al. 2004).
Figure: Flat-end arrows show the inhibitory effect of T-reg cells on B cells, dendritic cells, mast cells, basophils, eosinophils and mucus secretion during the normal response to allergens.
The Pathophysiological Asthmatic Response
Asthma is characterized by limited airflow which can be caused by any of the following: 1. Bronchoconstriction: the dominant pathophysiological event in asthma is the narrowing of the airway. Bronchoconstriction is contraction of the bronchial smooth muscle and this process narrows the airways in response to a variety of stimuli such as allergens or irritants. Allergies-induced bronchoconstriction results from IgE (Immunoglobulin E) dependent release of mediators from mast cells that include: histamine, tryptase, leukotrienes and prostaglandins that directly contract airway smooth muscle (National Heart, Lung, and Blood Institute 2007). Non-steroidal anti-inflammatory drugs such as aspiring can also cause similar effects and mediator release from airway cells (National Heart, Lung, and Blood Institute 2007). Other factors such as exercise, stress, cold air and irritants can cause the same acute airflow obstruction but the mechanisms regulating the response to these factors are less defined.
2. Airway edema: This is characterized by a collection of excess watery fluid. Factors such as edema, inflammation, mucus hyper secretion and formation of thickened mucus plugs (also structural changes involving hypertrophy and hyperplasia of airway smooth muscle cells).
Inflammation has an important role in the pathophysiology of asthma. Airway inflammation involves an interaction of many cell types and mediators within the airways that eventually results in the pathophysiological features of the disease: bronchial inflammation and airflow limitation that cause recurrent coughing, wheezing, and shortness of breath. Also, even though distinct types of asthma exist (e.g., intermittent, persistent, exercise-associated, aspirin-sensitive, or severe asthma), airway inflammation remains a consistent feature. The cellular activities and the response of the structural cells in asthma are quite consistent. The pattern of airway inflammation in asthma does not necessarily change depending upon disease severity, disease duration and persistence (National Heart, Lung, and Blood Institute 2007)..
At the bronchial cellular level, the mucosal barrier is disrupted causing leaky basement membrane and no mucociliary clearance. This contributes to an increase in the number of dendritic cells which gives rise to T helper 2 cells (Th2) cells which activate inflammatory cells. This causes inflamed airways, release of inflammatory mediators, and epithelial damage (Cohn et al. 2004).
The Role of Inflammatory Cells
1. Lymphocytes: T helper 1 cells and T helper 2 cells (Th1 and Th2) have distinct inflammatory mediator profits and effects on airway function. After the discovery of these distinct lymphocyte subpopulations in animal models of allergic inflammation, evidence emerged that, in human asthma, a shift, or predilection, toward the Th2-cytokine profile resulted in the eosinophilic inflammation characteristic of asthma. Also, generation of Th2 cytokines (e.g., interleukin-4 (IL-4), IL-5, and IL-13) could also explain the overproduction of IgE, presence of eosinophils, and development of airway hyper-responsiveness. There also may be a reduction in a subgroup of lymphocytes, regulatory T cells, which normally inhibit Th2 cells, as well as an increase in natural killer (NK) cells that release large amounts of Th1 and Th2 cytokines (National Heart, Lung, and Blood Institute 2007).
2. Mast cells: Activated mucosal mast cells releases bronchoconstrictor mediators such as histamine, cysteinyl-leukotrienes and prostaglandin D2 (National Heart, Lung, and Blood Institute 2007). Mast cells can also release cytokines that promote inflammation.
3. Eosinophils: Increased numbers of eosinophils exist in airways of most people with asthma (National Heart, Lung, and Blood Institute 2007). Eosinophils contain inflammatory enzymes, they produce leukotrienes and express a wide variety of pro-inflammatory cytokines. An increase in eosinophils often correlates with a greater severity of asthma. Studies have shown that treatment of asthma with corticosteroids reduces the number of circulating eosinophils and causes improvement. At the same time, another study has found an anti IL-5 (interleukin 5) treatment that has significantly reduced the number of eosinophils but did not control asthma (National Heart, Lung, and Blood Institute 2007). So perhaps eosinophils, along with being a primary effector cell in asthma, have different roles in different phases of the disease.
4. Neutrophils: Increased numbers of neutrophils are seen in the airways and sputum of people with asthma (also during acute exacerbations and smoking). The exact definitive role and mechanism of neutrophils is still being studies but leukotriene B4 may contribute to these processes (National Heart, Lung, and Blood Institute 2007).
5. Dendritic cells: These are antigen-presenting cells that interact with allergen from the airway and then migrate to regional lymph nodes to interact with regulatory cells that eventually stimulate T helper 2 cell production from naive T cells (National Heart, Lung, and Blood Institute 2007).
6. Macrophages: These are the most numerous cells in the airway and can be activated by allergens through low affinity IgE receptors to release pro-inflammatory mediator and cytokines (National Heart, Lung, and Blood Institute 2007).
The Role of Inflammatory Mediators
1. Chemokines: important in the recruitment of inflammatory cells into airways, expressed mainly in airway epithelial cells. Eotaxin is selective for eosinophils. Thymus and activation-regulated chemokine (TARCs) and macrophage derived chemokine (MDCs) recruit T helper 2 cells (National Heart, Lung, and Blood Institute 2007).
2.Cytokines: direct, modify and determine the severity of the inflammatory response in asthma. Th2 derived cytokines include interleukin 5 which is needed for eosinophil differentiation and survival, interleukin 4 which is important for Th2 cell differentiation and interleukin 13 which is important for IgE formation. Other key cytokines include IL-1-beta and tumour necrosis factor-alpha which increase the inflammatory response, and granulocyte-macrophage colony-stimulating factor (GM-CSF) which prolongs the survival of eosinophils in airways.
3.. Cysteinyl-leukotrienes: potent bronchoconstrictors that are derived from mast cells. Inhibition of this mediator has been linked with an improvement in lung function and asthma symptomology (National Heart, Lung, and Blood Institute 2007). Also, studies have shown leukotriene B4 to contribute to the inflammatory response by recruiting neutrophils (National Heart, Lung, and Blood Institute 2007). IgE: important for allergic diseases and the development and persistence of inflammation. It attaches to a cell surface via a high affinity receptor. The mast cell has large numbers of IgE receptors and when activated after interacting with an antigen, there’s a release of mediators to initiate acute bronchospasm and the release of pro-inflammatory cytokines to induce airway inflammation (National Heart, Lung, and Blood Institute 2007). Other cells such as basophils, dendritic cells and lymphocytes also have high affinity IgE receptors. The development of antibodies against IgE has proved that reducing IgE is effective in treating asthma (National Heart, Lung, and Blood Institute 2007).
4. IgE: important for allergic diseases and the development and persistence of inflammation. It attaches to a cell surface via a high affinity receptor. The mast cell has large numbers of IgE receptors and when activated after interacting with an antigen, there’s a release of mediators to initiate acute bronchospasm and the release of pro-inflammatory cytokines to induce airway inflammation (National Heart, Lung, and Blood Institute 2007). Other cells such as basophils, dendritic cells and lymphocytes also have high affinity IgE receptors. The development of antibodies against IgE has proved that reducing IgE is effective in treating asthma (National Heart, Lung, and Blood Institute 2007).
Figure: Difference between no disease condition. In particular, there is no mucociliary clearance and increase of T helper 2 cells in asthmatic conditions.
References
Cohn L, Elias JA, Chupp GL. Asthma: mechanisms of disease persistence and progression. Annu Rev Immunol. 2004; 22: 789-815. Review
Duffy DL. (1997). Genetic epidemiology of asthma. Epidemiol Rev, 19, 129–143.
Edfors-Lubs M. (1971). Allergy in 7000 twin pairs. Acta Allergol, 26:249–285
Gold DR & Wright R. (2005). Population disparities in asthma. Annu Rev Public Health 26: 89–113.
Keller, M., Lowenstein, S. (2002). Epidemiology of Asthma. eminars in Respiratory and Critical Care Medicine, 23(4). 317-329.
Lambrecht, B., Hammad, H. (2015). The Immunology of Asthma. Nature Immunology, 16(1), 45-56.
National Asthma Education and Prevention Program, Third Expert Panel on the Diagnosis and Management of Asthma. Expert Panel (Report 3): Guidelines for the Diagnosis and Management of Asthma, Bethesda (MD): National Heart, Lung, and Blood Institute (US); 2007 Aug. Section 2, Definition, Pathophysiology and Pathogenesis of Asthma and Natural History of Asthma. Available from: http://www.ncbi.nlm.nih.gov/books/NBK7223/
Pawankar. (2014). Allergic diseases and asthma: a global public health concern and a call to action. World Allergy Organ J., 7(1), 12.
Ronmark E, Lundback B, Jonsson EA, et al. (1997). Incidence of asthma in adults—report from the Obstructive Lung Disease in Northern Sweden study. Allergy, 52:1071–1081.
Reed, C. (2006). The natural history of asthma. Journal of Allergy and Clinical Immunology, 118( 3), 549-550.
Sears, M. (2014). Trends in the Prevalence of Asthma. Chest, 145(2), 219-225.
Skloot G, Permutt S,Togins A. (1995). Airway hyperresponsiveness in asthma: a problem of limited smooth muscle relaxation with inspiration. J Clin Invest, 96, 2393–2403.
Warner JA, Jones CA, Jones AC, et al. (2000). Prenatal origins of allergic disease. J Allergy Clin Immuno. 2(2), 493–498.
Weiss ST. Diet as a risk factor for asthma. In: Chadwick D, Cardew G, eds. The Rising Trends in Asthma. New York: Wiley; 1997:244–253