This is an old revision of the document!
Table of Contents
Anterior Cruciate Ligament Injury
Figure 1: The green line represents the placement
of the ACL. (Source: http://www.leadingmd.com)
<br> <br>
</style>
What is the ACL? <style justify> The knee joint is made up of the tibia, femur, and patella. It is not a very stable joint and is prone to injury due its complexity and its weight bearing function. (Cimino et al., 2010) Thus, it is stabilized and strengthened by ligaments. Ligaments attach bone to bone, and are very strong but not very flexible. Thus, when stretched, they remain so, and can tear if stretched too far. The knee joint is stabilized by several ligaments, the medial collateral ligament, lateral collateral ligament, posterior cruciate ligament, and anterior cruciate ligament (ACL). (Cimino et al., 2010) The ACL is the primary stabilizer of the knee. It goes diagonally from the top surface of the tibia to the end of the femur. The ACL functions to stop the tibia from anterior translation and internal rotation, and also prevents the over-straightening of the femur on the tibia. (Cimino et al., 2010) </style>
<style float-right>
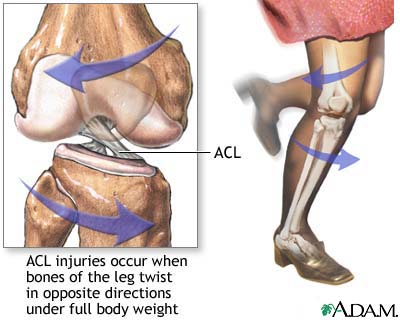
Figure 2: Shows the movement in leg that results in an ACL tear.
(Source: http://physioworks.com.au/)
</style>
<br>
How do ACL injuries occur?
<style justify> Sports activities are the primary source of ACL injuries. (Gianotti, 2009) Most ACL tears occur from non-contact injuries. 70% of ACL injuries are non-contact, while the remaining 30% result from contact. (Cimino et al., 2010) Non-contact ACL injuries occur primarily during deceleration of the lower extremity when the knee is at near full extension and the quadriceps are contracted. The hamstrings, which stabilize the ACL, are usually minimally contracted and the body weight is on the heel. (Cimino et al., 2010) Overall, the lower leg is fixed, and there must be enough torque rotating the tibia and femur in opposite directions to cause a tear. This kind of movement happens typically when there is a sudden change in direction. Common sports where non-contact injuries occur is in football, skiing, basketball, and gymnastics. (Cimino et al., 2010) In contact ACL injuries, where collision with another person or object occurs, there is hit to the leg where either the tibia is moved forward, or the femur backward, or the knee is over-extended. (Cimino et al., 2010) </style>
<br> <br> <br>
Epidemiology
<style justify> Incidence
In the U.S., there are about 100,000-200,000 ACL ruptures per year and about 100,000-150,000 ACL repairs per year. (Mall et al., 2014) These numbers are based on data from several years ago, thus may be higher today due to more younger individuals engaging in high-level sports and more older individuals staying active longer. The current incidence of ACL injuries and repairs is unknown. (Mall et al., 2014) The higher number of ruptures than repairs is due to those who opt for non-surgical treatment.
ACL injuries generally occur beginning in late adolescence. Ages leading up to late adolescence do not typically sustain ACL injuries, but rather sustain growth plate injuries due to the relative weakness of the cartilage at the epiphyseal plate compared with the ACL. (Cimino et al., 2010) </style>
<br>
Figure 3: Differences in female and male bodies leading to a difference in risk of sustaining an ACL injury.
(Source: http://www.braceability.com/)
<br> <br> <br> <br>
</style>
Risk Factors
<style justify> There is a 1.4-9.5 times increased risk of ACL tears in women compared to men. (Cimino et al., 2010) While males account for the majority of ACL injuries in the general population, when examining specific sports, females are observed to be at higher risk consistently. The higher number of male ACL injuries in the general population is due to the fact that they have greater exposure to athletic tasks that put one at risk of ACL injury (ex. cutting, jumping, contact sports). (Gianotti, 2009) Factors that play into a higher risk of sustaining an ACL injury in women compared to men include less hamstring strength, greater hormonal fluctuation, an increased Q angle, greater pelvic width, and greater quadriceps dominance. (Cimino et al., 2010) There are extrinsic and intrinsic factors that could increase likelihood of ACL injury in the general population. Some extrinsic factors include access to training facilities, playing field conditions (ex. uneven, wet, muddy), a higher level of competition, a more aggressive playing style, shoe surface that provide too much traction, and cold or rainy weather. (Cimino et al., 2010) Some intrinsic factors include body size, limb girth, flexibility, strength, reaction time, foot morphology, ligament dominance and laxity, and small ACL size. (Cimino et al., 2010) </style>
<br> <br>
Symptoms
<style justify> Symptoms of a severe and acute ACL injury include:
- Feeling or hearing a “pop” in the knee at the time of injury.
- Sudden instability in the knee. This may happen after a jump or change in direction or after a direct blow to the side of the knee.
- Pain on the outside and back of the knee.
- Knee swelling within the first few hours of the injury. This may be a sign of bleeding inside the joint. Swelling that occurs suddenly is usually a sign of a serious knee injury.
- Limited knee movement because of swelling and/or pain.
Following an acute injury, the patient will almost always have to stop whatever activity they are doing, however, they may still be able to walk.
If the ACL injury is chronic (long-lasting and recurrent), the knee buckles or gives out, sometimes with pain and swelling. This occurs more frequently over time. It is important to note that not everyone with an ACL injury develops a chronic ACL deficiency. </style>
<br>
Diagnosis
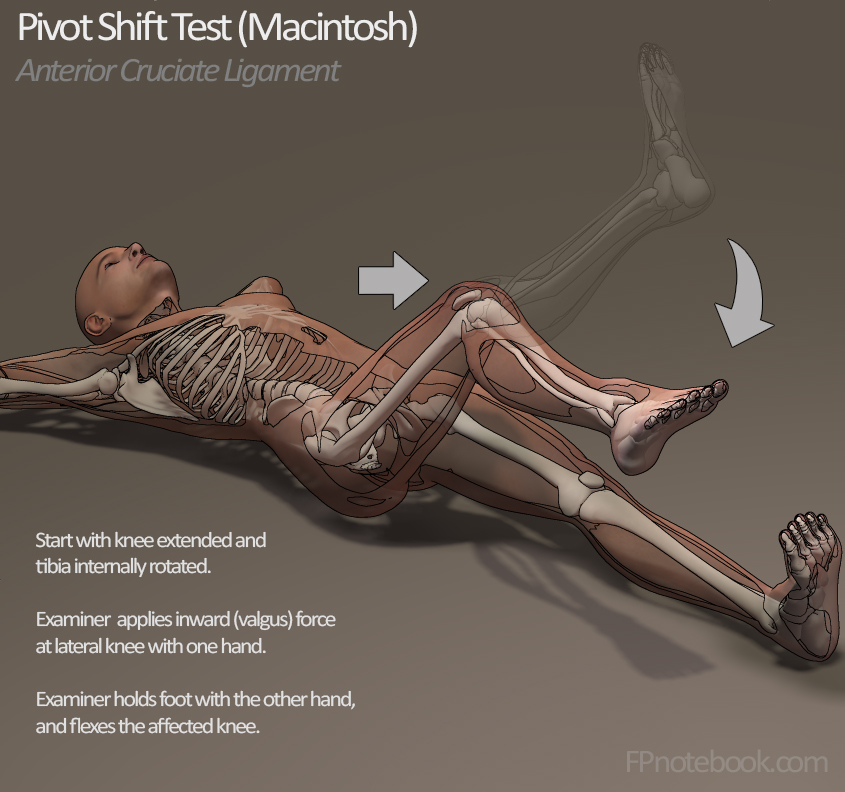
<style justify> For the clinical examination of a suspected ACL injury, the pivot-shift test, anterior drawer test and Lachman test are used.
The pivot shift is difficult to perform in the office, it is usually more helpful in the operating room with a patient under the influence of anesthesia. The pivot shift maneuver identifies abnormal motion of the knee joint when there is an ACL tear present. </style>
Figure X: Illustrates the steps for the pivot shift test (Source: Fpnotebook,2016)
<style justify> The drawer test is used in the primary clinical assessment of suspected rupture of the cruciate ligaments in the knee. During the test, the patient should be supine with the hips flexed to 45 degrees, the knees flexed to 90 degrees and the feet flat on table.
The Lachman test is known by most authorities as the most reliable and sensitive test, and usually a better alternative to the anterior drawer test. The ACL can also be detected using a magnetic resonance imaging scan (MRI scan).
Even though clinical examination if done by a professional can be accurate, the diagnosis is usually confirmed by MRI scan, which has significantly narrowed the need for diagnostic arthroscopy and which has a greater accuracy than clinical examination. It may also show a graphic of other structures which may have been involved in the injury, such as a meniscus, or collateral ligament, or posterolateral corner of the knee joint. </style>
<br>
Treatment
<style float-right>

Figure X: Illustrates a typical knee brace looks like.
(Source:Better Braces, 2016). </style>
<style justify> Nonsurgical Treatment: Torn ACL are not able to healed without surgery, however surgery may not always be a viable option for elderly patients or patients with low activity levels. In this situation, non-surgical treatment methods would be more beneficial. These methods are only recommended if the overall stability of the knee is intact (UCSF, 2016). Some of these non-surgical treatment methods can include:
- Use of Knee Braces: This can be recommended by your doctor. Knee braces help support and protect the knee and the ACL from further damage. Furthermore, crutches may be implemented to transfer your weight away from your injured knee. This further protects and prevents more damage.
</style>
<style justify>
- Physical Therapy: This is usually recommended by doctors when swelling and inflammation of the knee go down (American Academy of Orthopaedic Surgeons, 2016). This program involves a series of exercises that will help improve function of the knee joint and strength surrounding muscles. Some of these exercises focus on training the Gluteus Maximus and Gluteus Medius in non-weight scenarios, followed by weight bearing scenarios. This helps to improve the control of the hip movements. In addition, exercises that focus on strengthening the Quadriceps muscles are also implemented. This is because this helps with improved bending of the knee. These exercises are also being implemented in ACL prevention programmes.
ACL Surgery: ACL reconstruction is recommended for those:
- Who are young and active
- Who suffer from persistent knee pain
- Who suffer pain during routine activities (ex- Walking)
- Who are aspiring athletes
</style>
<style justify> Surgical Treatment: The most common method to repair a torn ACL is through ACL reconstructive surgery. This surgery is required to replace the torn anterior cruciate ligament with either another ligament from your body or from a tissue sample from a cadaver. This tissue graft will help with the growth of a new ligament. Ultimately, this surgery helps restore knee function and stability (Kranz, 2016). </style>
<style float-right>
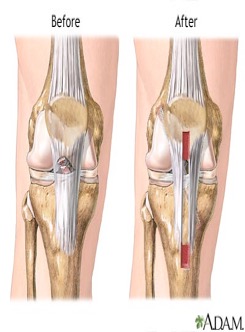
Figure X:Demonstrates the knee and ACL
before and after surgery. (Source:A.D.A.M, 2013). </style>
<style justify> Tissue grafts can be retrieved from many sources. Some of these sources can include:
- Patellar tendon: Graft can be taken from the tendon that attaches from the bottom of the patella to your tibia.
- Hamstring: The graft can be taken from the tendon that connects the hamstring muscle to back of the knee.
- Quadriceps: A graft from the tendon that connects the quadriceps muscle.
- Cadaver: It is retrieved from a corpse, and is called an allograft (Kranz, 2016).
</style>
<style justify> Allografts: Risks and Benefits: An allograft is when a tissue graft is retrieved from a member of the same species but are not genetically identical to the recipient. The increased in the development of new techniques and research are one of the main reasons for the rise in the use of allografts in surgery. Some of the advantages of using allografts are very beneficial in cases requiring multiple ligament reconstruction surgeries and they have a very low rate of donor morbidity. However, this type of tissue graft does have some disadvantages. Primarily, this method is very costly and takes a longer time to treat and prepare for the procedure. Furthermore, the sterilization process involves radiation, which can potentially alter the biomechanical properties of the graft. Most importantly, this type of tissue graft has been associated with elongation and rupturing after surgery. A study was conducted on 120 young active adults that were cadets at the U.S. Military Academy at West Point. This study observed that an allograft ACL surgery was approximately 7 times more likely to fail compared to an autograft ACL reconstruction (Mayo Clinic, 2016). </style>
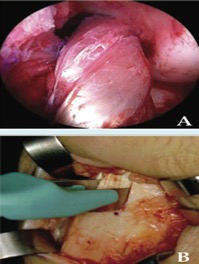
<style float-left>

Figure 4: Illustrates the different type of
allografts that can be used for this surgery.
(Source: Mayo Foundation for Medical
Education and Research, 2016).
</style>
<style justify> Autografts: Risks and Benefits: An autograft is when a tissue graft is retrieved from one part of the recipient’s body and placed in another part. Some common autograft sites can include patellar, hamstring and quadriceps tendons. Some of the associated advantages with this type of graft are minimal contamination, disease transmission and less structural alteration due to not irradiating the graft. The disadvantage associated with this type of graft is there is an increased post-surgery pain and recent research has indicated that if the hamstring tendon is used as a graft and the diameter is less than 8 millimetres, then there is increased risk of failure of the graft (Mayo Clinic, 2016). </style>
<style justify> How to Prepare for ACL reconstruction: Throughout this whole process, you will always be meeting with various health practitioners to help prepare you for this procedure. Before the surgery, the doctor and surgeon will discuss treatment options as well advising on medical and personal decisions required. Also, using medical imaging techniques several knee examinations occur before and after the surgery. During the day of the surgery, it is recommended you fast for 12 hours and refrain from aspirin and other blood thinning medications, as this may cause complications during the surgery. It is also recommended to have someone else with you so they can support you and help with post-surgery instructions to follow. The most important advice would be to ask questions and for advice from your health practitioner, as this may reduce some of the burden associated with the procedure (Krans, 2016). </style>
<style float-right>
Figure X:Illustrates the retrieval and
extraction of an autograft.
(Source:Mayo Foundation for
Medical Education and Research, 2016). </style>
<style justify> How ACL Reconstruction is Performed: This procedure involves the use of intravenous (IV) lines, which are used to administer and inject medication as well as sedatives. Next, the allograft or autograft is prepared to be implanted into the knee. The tendon is prepared with bone plugs, which can anchor the tendon to the knee. Next, an incision is made into the front of the knee to allow for a thin tube that can allow for a fiber optic camera and surgical tools to pass through. Furthermore, the surgeon will remove the torn ACL and remove debris from the area. The surgeon will then drill small holes into your tibia and femur so the bone plugs can be attached with posts, screws, staples, or washers. After, the attachment of the new ligament, the surgeon will assess the knee’s motion and will ensure that the graft is secure. In addition, after the knee is assessed, the surgeons will suture the wound up. They will then place a brace on your knee to stabilize it. This procedure length can vary as there are many various techniques and versions of this procedure. It all depends on the various factors involved (Krans, 2016). </style>
<br>
<style justify> Risks of ACL Reconstruction: There are some risks associated with ACL reconstruction surgery. These can include: </style>
<style float-left>
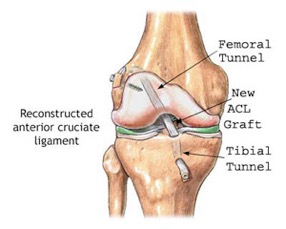
Figure X: Illustrates the surgical repair of the ACL
and knee.
(Source:Tower Orthopaedics, 2016).
<br>
</style>
<style justify>
- Excessive Bleeding and blood clotting
- Persistent Knee Pain
- Possible Infections
- Loss of Knee motion
- Rejection of tissue graft, causing inflammation
There are other risks that are also associated with this procedure. If someone is a young growing child, they can have potential growth plate injuries, preventing the growth of their bones in affected areas. One way to prevent this is that doctors advise children to wait until they are older to have this procedure. Although there are risks associated with this procedure, this procedure has been labelled a gold standard solution to persistent knee injuries. This procedure has approximately 82 to 90% success rate (Krans, 2016).
Post ACL Reconstruction: The road to recovery from surgery involves rehabilitation. Also, to deal with some of the other symptoms such as excessive pain, pain suppression medications are prescribed. Furthermore, to prevent infections to the wound, it is suggested that you clean the wound and keep it clean. In addition, to alleviate pain and reduce inflammation to the knee, it is recommended that you ice this area, as advised by the doctor. After a few weeks, the patient should be able to regain range of motion in the knee. Athletes typically return to full fitness within 6 to 12 months. Finally, this is all followed by physical therapy and rehabilitation, which is very vital to the success of recovering (Krans, 2016).
</style>
<br> <br> <br>
Rehabilitation
<style justify> When rehabilitating an ACL injury, it is important to ensure that therapy begins immediately after surgery. The PRICE method is most commonly used to help reduce swelling and discomfort. Physical therapy revolves around strengthening the muscles surrounding the knee. The ACL itself is simply a ligament and so it is difficult to target it directly with rehabilitation, instead by strengthening the surrounding muscles such as the quadriceps, hamstrings, and gastrocnemius, we hope to help stabilize the knee and alleviate unnecessary strain on the knee and its ligaments. There are numerous exercises which can be done to strengthen these muscles and are easily found and well known, so instead of discussing different exercises we will look at open vs kinetic chain exercises and which will be better in rehabilitating the newly grafted ACL.
A kinetic chain exercise is simply one which has more than one joint moving at once to contract or extend a target muscle. Open kinetic chain exercises differ from closed kinetic chain exercises by the degree of freedom of the distal limb. In most cases this will either be the hands or the feet. With open kinetic chain exercises you have a varying degree of freedom in the distal end which simply means that it isn’t fixed to anything. An example of this could be a dumbbell press where at the top of the motion the hands are not restricted to the same spot each time. Open kinetic chain exercises are generally non-weight bearing, and are more targeted to restore mobility and full range of motion. On the other hand, closed kinetic chain exercises have the distal limb attached to a fixed component, for example something like a bar in a pull up. The hands are holding on to a bar which is fixed in space. There are benefits to both open and closed kinetic chain exercises which really depends on the goals of training and strengthening.
When specifically looking at an ACL injury and which type of exercise would be best it is important to note the various forces acting on the knee. In an open kinetic chain exercise, such as the leg extension we have the quadriceps being activated to move the foot forward. This is an excellent exercise for quad development however the open kinetic aspect allows for an increased shearing force on the ACL as the motion being performed is one where the tibia is moving anteriorly and the femur is moving posteriorly. So, despite being an excellent exercise for strengthening the quadriceps, the leg extension would not be one of the best options for rehabilitation. Instead something like a squat which is a closed kinetic chain exercise is a much better option. This is because of the activation of the posterior chain including the hamstrings, and soleus. They help produce a posterior shearing force which counteracts the anterior force generated by the quadriceps and so there is a lower shearing force on the ACL which means it is under less stress during the squat than the leg extension. By doing something like the squat it is more beneficial for rehabilitation as progressive overload will be achievable in a shorter timeframe. Therefore it can be concluded that closed kinetic chain exercises can provide better results for rehabilitating an ACL injury.
</style>
<br>
References
Cimino, F., Volk, B. S., and Setter, D. (2010). Anterior cruciate ligament injury: Diagnosis, management, and prevention. American Family Physician, 82(8), 917-918.
Gianotti, S. M., Marshall, S. W., Hume, P. A., and Bunt, L. (2009). Incidence of anterior cruciate ligament injury and other knee ligament injuries: A national population-based study. Journal of Science and Medicine in Sport, 12, 622-627.
Mall, N. A., Chalmers, P. N., Moric, M., Tanaka, M. J., Cole, B. J., Bach, B. R., and Paletta, G. A. (2014). Incidence and trends of anterior cruciate ligament reconstruction in the united states. The American Journal of Sports Medicine, 42(10), 2363-2370.
Mayo Clinic. (2016). Clinical updates. Retrieved from http://www.mayoclinic.org/medical-professionals/clinical-updates/orthopedic-surgery/anterior-cruciate-ligament-reconstruction-graft-selection
Zazulak, B. T., Hewett, T. E., Reeves, P. N., Goldberg, B., and Cholewicki, J. (2007). Deficits in neuromuscular control of the trunk predict knee injury risk. The American Journal of Sports Medicine, 35(7), 1123.