Table of Contents
High Protein Diets and Kidney Function
<style justify> The Acceptable Macronutrient Distribution Ranges (AMDR) are the proportion of one’s caloric intake which should come from each macronutrient. It is recommended that 10-35% of daily energy intake should be provided by protein (Whitney, Rolfes, Hammond and Piche, 2013). In a typical Western diet, more than twice the recommended levels of protein are often consumed, and some research supports that this may be associated with the increased prevalence of chronic kidney disease in Western society (Hariharan, Vellanki and Kramer, 2015). Conversely, high protein diets are increasingly recommended for weight loss and weight management programs, and there is much controversy regarding the safety of such long-term diets. An article written by Kamal Patel, and featured on examine.com (2014), attempts to demystify the claim that high protein diets lead to increased glomerular filtration rate (GFR) which is a measure of the amount of blood that filters through the glomeruli every minute (mL/min). There is speculation that an increase in GFR leads to stress on the kidneys, resulting in kidney damage.
</style>
<br> <br> <br> <br> <br> <br> <br> <br> <br> <br>
Animal studies suggest correlation between high protein intake and kidney damage
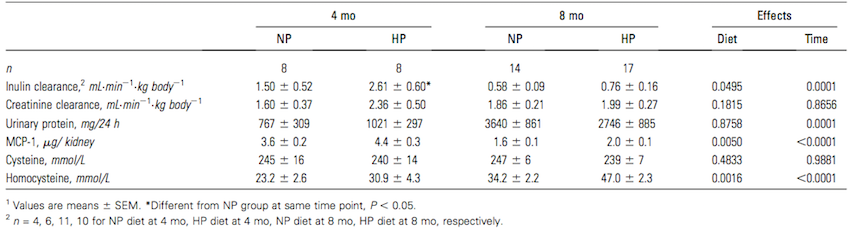
Figure 1: Renal function, MCP-1, and plasma homocysteine in pigs that consumed NP or HP diet for 4 or 8 months (Source: Jia et al, 2010) </style>
<style justify> Research has been conducted on animals, supporting the claim that high protein diets can lead to kidney damage.
<br>
Jia and colleagues (2010) tested the effects of a high protein diet on adult pigs. Pigs have very similar renal anatomy and physiology to that of humans, and thus are an appropriate test animal to use (Jia et al., 2010). Adult pigs were fed a diet consisting of either 15% of total calories from protein or 35% of total calories from protein for eight months. Protein came from a mixture of both plant and animal sources to closely resemble an average human diet. Between both the high and normal protein diets, lipid, fibre and micronutrient compositions were made equal to eliminate the presence of any confounding variables from diet. (Jia et al., 2010) After eight months, adult pigs fed the high protein diet had significantly higher kidney and glomerular volumes, however there was no significant difference in body mass between the high protein and normal protein groups. Additionally, after eight months, pigs fed the high protein diet exhibited more histological renal damage with 55% more fibrosis, and 30% more glomerulosclerosis in the kidney. There were also higher plasma homocysteine levels at 4 and 8 months. However, overall renal function as determined by inulin clearance, creatinine clearance, or proteinuria was not affected by a high protein diet, as any increase in values at 4 months did not persist in the long term and differences overall were not statistically significant (Figure 1). Due to the similarity between pig and human renal physiology, this study presents evidence that suggests high protein diets may potentially be harmful to human renal function. (Jia et al., 2010) </style>
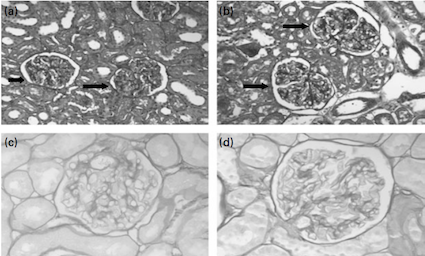
Figure 2: Glomeruli from rats given a) normal-protein or b) high protein diet
for 4 months; Glomeruli from rats given c) NP or d) HP diet for 17 months
(Source: Wakefield et al., 2011) </style>
<br> <br>
<style justify> Wakefield and colleagues (2011) studied the effects of a high protein diet on Sprague-Dawley rats to investigate if the findings of Jia and colleagues’ (2010) pig model were species specific or more generalizable. 70 day old female Sprague-Dawley rats were randomized to either a normal-protein or a high protein diet for 4, 8, 12 and 17 months. The normal-protein diet consisted of 15% of calories from protein and the high protein diet consisted of 35% of calories from protein. The two diets were kept similar with regards to caloric content, lipids, fibre and micronutrient content. (Wakefield et al., 2011) The rats fed with a high protein diet displayed concerning kidney adaptations. Rats fed on a high protein diet had larger kidneys and glomeruli, and exhibited 33% more glomerulosclerosis compared to the rats fed a normal-protein diet (In Figure 2, d) shows a hardened glomerulus, compare to c)). This finding is consistent with the histological damage shown in Jia and colleagues' (2010) study with adult pigs. Rats fed high protein diets exhibited altered renal function with a 27% higher creatinine clearance. Creatinine clearance is a marker of glomerular filtration rate (GFR) and proteinuria, both of which were significantly elevated in the rats fed on the high protein diet. These findings contrast to Jia and colleagues' (2010) experiment where renal function in adult pigs was not affected. The evidence presented in this study suggests that in rats, high protein diets are associated with kidney damage, consistent to Jia and colleagues (2010) study with pigs, however this relationship cannot conclusively be generalized to humans. (Wakefield et al., 2011) </style>
<br> <br> <br> <br> <br>
Short and long-term effects of high protein diets
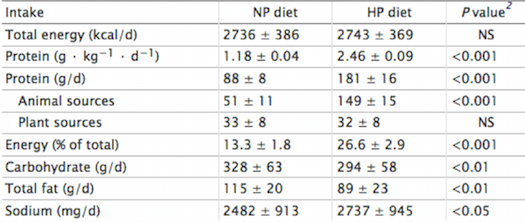
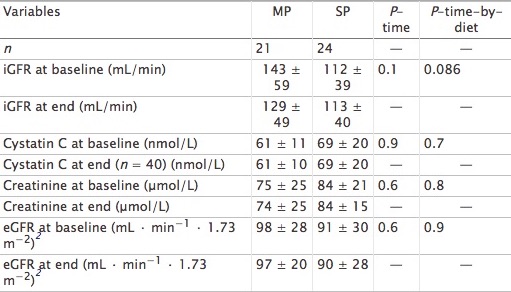
Figure 3: Total energy and macronutrient intakes during a 7-d normal-protein (NP) and high-
protein (HP) diet in 24 healthy normal-weight men </style>
<style justify> Frank and colleagues (2009) Investigated the effects of a short-term high protein diet on healthy kidney functions, such as renal hemodynamics and clinical-chemical factors. Young men were assigned to either a high protein diet containing 2.4 g/ kg•d or a normal protein diet containing 1.2 g/kg•d for a duration of seven days. The filtration fraction was taken from the 24 subjects on day seven. Researchers found that renal-dynamics were altered, with a significant rise in GFR (Glomerular filtration rate) and the filtration fraction. However, adaptive changes in renal function might be caused by sodium intake, which is significantly parallel to the high protein diet. Importantly, sodium is known for its possible effects on GFR through tubular reabsorption. This study suggests that further research should be conducted to analyze the effects of chronic high protein intake on GFR, while controlling for sodium. </style>
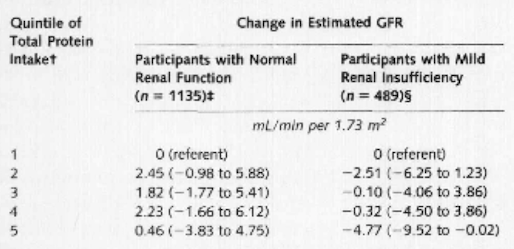
Figure 4: Multivariate linear regression results for change in estimated glomerular filtration
rate according to quintile of total protein intake </style>
<br> <br> <br> <br> <br> <br> <br> <br>
<style justify> Knight and colleagues (2003) A long-term study where protein intake had an impact on the change in rate of renal function in women over an 11 year period was examined. Over 1500 women between the ages of 42 and 68 enrolled in the Nurses’ Health study and gave blood samples, which measured creatinine levels. As protein intake increased, the change in estimated GFR became more pronounced as well as the confidence interval (1.14 mL/min per 1.73 m2 [CI, −3.63 to 5.92 mL/min per 1.73 m2]). Through multivariate linear regression analyses, it was shown that there was no significant relation between high protein intake and change in glomerular filtration rate in women with normal renal function. However, high intake of non-dairy animal protein might be linked with accelerated renal function decline in women with mild renal insufficiency. </style>
<br> <br> <br> <br>
High protein intake and at risk individuals
<style justify> According to the National Kidney Foundation (2015), a healthy GFR is approximately 90mL/min/1.73m2, while glomerular hyperfiltration results when GFR ranges from 125mL/min/1.73m2 to 175mL/min/1.73m2 (Helal, Fick-Brosnahan, Reed-Gitomer and Schrier, 2012). Glomerular hyperfiltration leads certain individuals with diabetes or hypertension to an increased risk of developing kidney disease. This can ultimately which can cause a decrease in the GFR (National Kidney Foundation, 2015). </style>
<br>
<style justify> Jesudason and colleagues (2013) They conducted a study to examine the effects of a high protein diet on weight loss in individuals with type 2 diabetes mellitus and early kidney disease. Approximately, forty-five individuals were selected for the study. These individuals were diagnosed with Type 2 Diabetes and showed symptoms of early Kidney Disease. They were then assigned to either a moderate protein diet (30% of total calories from protein) or a standard protein diet (20% of total calories from protein) for a duration of one year. Both groups demonstrated weight loss, however there was no significant difference in the weight loss between the two groups. The results demonstrated that weight loss was associated with changes to GFR. From Figure 5, it can be concluded that individuals with a normal baseline GFR (< 120mL/min/1.73m2) displayed an increase in GFR, while individuals with hyperfiltration experienced a decline in the GFR. Results were similar between both groups indicating that long-term diets that consisted of high proteins are not necessarily associated with hyperfiltration (Jesudason, Pedersen and Clifton, 2013). </style>
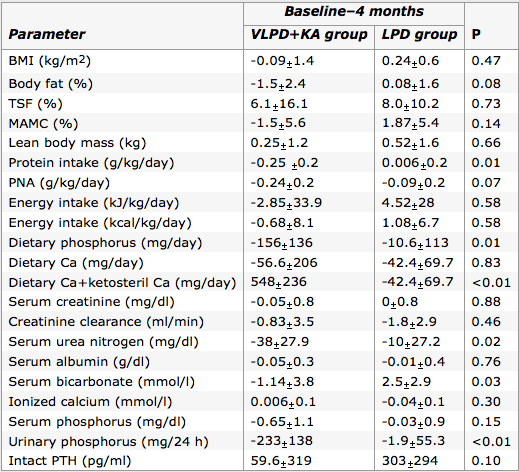
Figure 6: Comparison of the changes through 4 month period in VLPD+KA group with LPD
group on various parameters. (Source: Feiten et al., 2005) </style>
<style justify> At-risk individuals have been recommended to refrain from eating high protein diets (Schwingshackl and Hoffman, 2014), due to the presumed associated increase in GFR and the concept of increased GFR leading to higher risk of developing Kidney Disease in individuals with Diabetes (National Kidney Foundation, 2015). However, the research suggests that high protein diets associated with weight loss may be beneficial to individuals with Type 2 Diabetes and early stage Kidney Disease, since such diets appeared to normalize GFR in some individuals. Controversy exists regarding the association of hyperfiltration and Kidney Disease. It is suggested that an increase of GFR in the absence of renal hypertension is not associated with kidney pathology (Helal, Fick-Brosnahan, Reed-Gitomer and Schrier, 2012). Therefore, in order to demonstrate that high protein diets are associated with kidney damage, research would need to support that such diets result in increased GFR and increased renal blood pressure. </style>
Figure 5: Demonstrates the baseline and end GFR values of both moderate and standard
protein diet groups after 1 year period. (Source: Jesudason, Pedersen and Clifton, 2013 ) </style>
<br> <br> <br> <br> <br> <br> <br> <br> <br> <br> <br> <br> <br> <br> <br> <br> <br> <br> <br> <br>
<style justify> Feiten and colleagues (2004) It is important to note when the use of a Very Low Protein Diet would be more beneficial to an individual than a high protein diet. This is usually the case with individuals afflicted with chronic kidney disease (CKD). This study challenged the normal treatment of a Low Protein Diet (0.6g/kg/day) with that of a Very Low Protein Diet (0.3g/kg/day) supplemented with ketoacids. They had two groups of 12 subjects with one group undergoing the Low Protein Diet and the other with a Very Low Protein Diet & ketoacids supplementation for four months. The results highlighted in Figure 6, were able to conclude that the Very Low Protein Diet & ketoacid group had the same nutritional standing as the other group, however had better results with phosphorus and calcium metabolism while also leading to lower serum urea nitrogen levels. These results are indicative of an effective therapy for advanced CKD patients. It is important to recognize when a person requires a Very Low Protein Diet instead of a high protein diet because of the varying amount of short-term stress it causes on the kidney. </style>
<br> <br>
High protein diet and obesity
<style justify> Zhaoping and colleagues (2010) They conducted a research experiment which investigated the adverse effects of a high protein diet on kidney function during weight loss. The experiment integrated 100 obese men and women who were monitored for the duration of one year. During the experiment, high protein consumption was clearly defined at 2.2g/kg versus standard protein ingestion, which was at 1.1g/kg. As for results, researchers had not found a direct or indirect correlation between inhibited renal function and high protein diet. Furthermore, no variation was found in creatinine clearance, which suggests an unmodified GFR rate. Thus, it is evident that this study supports the idea that a high protein diet safely reduces an obese individual’s Body Mass Index with no adverse concerns regarding kidney function. </style>
<style justify> Friedman and colleagues (2012) It was a controlled study that examined whether low-carbohydrate high protein diets led to any harmful renal effects. People that took part in the study were healthy obese individuals who followed the high protein diet for two years, as well as, another group who followed a low fat diet. The primary focus for the researchers was the GFR measured by creatinine clearance and albuminuria. The researchers found that even though the levels of solute excretion such as calcium and sodium were slightly raised in the high protein diet subjects, it was still lower than the low fat diets. In addition, they also measured urinary calcium excretion and found that despite an increase, there was no presence of new kidney stones. Besides that, small reductions in serum creatinine at three months (4.2% relative to low fat diet), as well as serum urea at two years (8.2%) were observed, indicating kidney adaptation. Upon review of all collected data, the researchers concluded that low carbohydrate and high protein diets in healthy obese individuals does lead to weight loss without causing renal damage to the kidney. </style>
Does Protein source Affect Renal Function?
<style justify>
There are many different types of protein sources available to humans today. Perhaps some sources of protein provide better protection for renal function than others. Aukema et al. (2010) compared the effects of soy based protein diets to those of plant based protein diets on renal protection. They used Weanling Han rats who were afflicted with kidney disease, and subjected them to hemp, pea, soy, and casein protein sources. Upon review of the experimental data they found that hemp and soy protein sources resulted in the least amount of kidney inflammation, as well as a more normal serum creatinine level, and smaller cyst sizes. This allowed them to conclude that there was a difference in kidney disease protection when it came to the source of the protein. Despite using rat test subjects instead of humans, the study still provides valuable insight into human chronic kidney disease treatment. There is a strong misconception that vegetarian diets are the healthiest type of diet, and while acquiring the necessary nutrients from a vegetarian diet is possible, it is crucial to include soy based protein for chronic kidney disease patients. Limiting one’s self to a single source of protein would be an opportunity passed to slowing renal disease progression.
Another study done by Moe et al. (2011) looked at animal based protein and plant based protein with respect to phosphorus homeostasis in chronic kidney disease. Increases in parathyroid hormone (PTH) and fibroblast growth factor-23 (FGF23) induce phosphaturia which maintains phosphorus levels in an appropriate range. Moe et al. (2011) performed a crossover trial involving nine patients who had an average GFR at 32 ml/min to allow for a fair comparison of both diets. They found that after a week of implementing the vegetarian diets, there was a decrease in serum phosphorus and FGF23 levels. Progressive deterioration of renal function is usually indicative in an increase in FGF23 levels. This study was able to show the significant effect on phosphorus homeostasis in patients which might be due to decreased bioavailability of phytate-bound phosphorus or the higher availability of protein in meat-based diets, placing strain on the kidney. High FGF23 were more prevalent in the meat based diet, and could have possibly inhibited PTH. These studies show the importance of phosphate and protein source that the phosphate comes from, especially regarding those with chronic kidney disease. Future studies should look at the long term effects of high protein intake on phosphorus levels.
<br>
High Protein Diets Do Not Affect Kidney Function
Through systematic review and meta-analysis, Schwingshackl and Hoffman (2014) investigated the effects of high protein versus low/normal protein diets in relation to renal function on subjects who did not have any form of CKD. Many literatures were performed using the electronic databases MEDLINE, EMBASE, and the Cochrane Trial Register until February 27th, 2014. Thirty studies which included 2160 subjects were used. High protein diets resulted in a significantly higher GFR, serum urea, and calcium excretion in comparison to low protein/normal protein diets. A limitation that exists in the present review consist of the limited number of studies and their heterogeneity of design. The many studies included in the analyses varied in terms of type(s) of diets used, definition of high protein and low protein/normal protein diets, study population, intervention time, as well as nutritional assessment. Additionally, the sample size of 2160 subjects in the current meta-analysis establishes statistically significant mean differences. Although, the subjects experienced an increase in GFR, nobody reported clinical symptoms of kidney pathology. These changes can be associated with physiological adaptive mechanisms induced by high protein diets without any clinical relevance.
Poortmans and Dellalieux (2000) investigated the relationship between high protein intake and renal function in both body-builders and athletes. The range of protein intake for the two groups was between 1.35 to 2.8 g/kg•b•wt. Through blood and urine analysis, they found no significant differences between the test groups regarding concentrations of plasma protein, creatinine and uric acid. High concentrations of these variables are indicative of protein absorption and potential renal impairment. Despite high plasma variables in both groups, there was no accumulation of urea, thus indicating that they were within the upper limit of normal. In addition, the GFR assessed by creatinine clearance suggested no sign of glomerular hyperfiltration. This supports that the high protein diet under 2.8 g/kg•b•wt does not adversely affect kidney physiology.
</style>
<br>
Conclusion
<style justify> There is significant evidence presented in many scientific studies that recognizes high protein diets alter renal function in humans. However, there are inconsistencies between the results of short-term and long-term studies. Short term studies demonstrate an accompanied increase of GFR with high protein diets, whereas long-term studies lack statistical significance for a change in GFR, suggesting adapting renal physiology during chronic high protein intake. Additionally, source of protein and health status are important confounding variables that must be considered when evaluating the effects of kidney function of such diets. Despite the controversy surrounding the safety of high protein diets, there is no conclusive evidence supporting a direct causation between such diets and renal damage. </style>
References
Aukema, H. M., Gauthier, J., Roy, M., Jia, Y., Li, H., & Aluko, R. E. (2011). Distinctive effects of plant protein sources on renal disease progression and associated cardiac hypertrophy in experimental kidney disease. Molecular nutrition & food research, 55(7), 1044-1051.
Feiten, S. F., Draibe, S. A., Watanabe, R., Duenhas, M. R., Baxmann, A. C., Nerbass, F. B., & Cuppari, L. (2005). Short-term effects of a very-low-protein diet supplemented with ketoacids in nondialyzed chronic kidney disease patients. European journal of clinical nutrition, 59(1), 129-136.
Frank, H., Graf, J., Amann-Gassner, U., Bratke, R., Daniel, H., Heemann, U., & Hauner, H. (2009). Effect of short-term high-protein compared with normal-protein diets on renal hemodynamics and associated variables in healthy young men. The American journal of clinical nutrition, 90(6), 1509-1516.
Friedman, A. N., Ogden, L. G., Foster, G. D., Klein, S., Stein, R., Miller, B., … & Wyatt, H. R. (2012). Comparative effects of low-carbohydrate high-protein versus low-fat diets on the kidney. Clinical Journal of the American Society of Nephrology, 7(7), 1103-1111.
Halbesma, N., Bakker, S. J., Jansen, D. F., Stolk, R. P., De Zeeuw, D., De Jong, P. E., & Gansevoort, R. T. (2009). High protein intake associates with cardiovascular events but not with loss of renal function. Journal of the American Society of Nephrology, 20(8), 1797-1804.
Hariharan, D., Vellanki, K., & Kramer, H. (2015). The Western Diet and Chronic Kidney Disease. Current hypertension reports, 17(4), 1-9.
Helal, I., Fick-Brosnahan, G. M., Reed-Gitomer, B., & Schrier, R. W. (2012). Glomerular hyperfiltration: definitions, mechanisms and clinical implications.Nature Reviews Nephrology, 8(5), 293-300.
Jesudason, D. R., Pedersen, E., & Clifton, P. M. (2013). Weight-loss diets in people with type 2 diabetes and renal disease: a randomized controlled trial of the effect of different dietary protein amounts. The American journal of clinical nutrition, 98(2), 494-501.
Jia, Y., Young Hwang, S., House, J. D., Osborn, M. R., Weiler, H. A., O, K., and Aukema, H. M.(2010). Long-term high intake of whole proteins results in renal damage in pigs. The Journal of Nutrition. 140: 1646-1652. sease. Current hypertension reports, 17(4), 1-9.
Knight, E. L., Stampfer, M. J., Hankinson, S. E., Spiegelman, D., & Curhan, G. C. (2003). The impact of protein intake on renal function decline in women with normal renal function or mild renal insufficiency. Annals of internal medicine, 138(6), 460-467.
Li, Zhaoping, Treyzon, L., Chen, S., Yan, E., Thames, G., & Carpenter, C. L. (2010). Protein-enriched meal replacements do not adversely affect liver, kidney or bone density: an outpatient randomized controlled trial. Nutr J, 9, 72.
Moe, S. M., Zidehsarai, M. P., Chambers, M. A., Jackman, L. A., Radcliffe, J. S., Trevino, L. L., … & Asplin, J. R. (2011). Vegetarian compared with meat dietary protein source and phosphorus homeostasis in chronic kidney disease.Clinical Journal of the American Society of Nephrology, 6(2), 257-264.
Poortmans, J. R., & Dellalieux, O. (2000). Do regular high protein diets have potential health risks on kidney function in athletes?. International Journal of Sport Nutrition, 10(1), 28-38.
Schwingshackl, L., & Hoffmann, G. (2014). Comparison of high vs. normal/low protein diets on renal function in subjects without chronic kidney disease: a systematic review and meta-analysis.
Wakefield, A. P., House, J. D., Ogborn, M. R., Weiler, H. A., & Aukema, H. M. (2011). A diet with 35% of energy from protein leads to kidney damage in female Sprague–Dawley rats. British journal of nutrition, 106(05), 656-663.
Whitney E., Rolfes, S. R., Hammond, G. and Piche, L. A. (2013). Understanding nutrition. Toronto: Nelson Education Ltd.