This is an old revision of the document!
Table of Contents
What is Coronavirus?
The name “Coronavirus” was found in the mid-1960s and it was derived from the “corona” or the crown-like shape observed for these viruses. Coronaviruses are a large family of viruses that cause illnesses. There are four main sub-grouping of the virus: Alpha, Beta, Gamma and Delta. Fun fact! Corona means crown in Latin. The name represents the crown-like spikes on the surface of this virus (Centres for Disease Control and Prevention, 2020).
These illnesses range from the common cold to severe diseases such as the Middle East Respiratory Syndrome (MERS), Severe Acute Respiratory Syndrome, and the 2019 Novel Coronavirus (COVID-19).
Coronaviruses are zoonotic. Zoonotic viruses mean that they are transmitted between animals and people. In the past, SARS was transmitted from cats to humans. MERS was transmitted from camels to humans (Centres for Disease Control and Prevention, 2020).
COVID-19 is the novel coronavirus that emerged in Wuhan, China during late 2019. It is most likely from an unidentified animal in the live animal markets. A novel coronavirus means that this strain of coronavirus had not been previously identified in humans(Centres for Disease Control and Prevention, 2020;World Health Organization, 2020).
Severe Acute Respiratory Syndrome (SARS)
Overview of Epidemic
The SARS epidemic started with an index case (patient zero) in the city of Foshan, close to Hong Kong, within the southern Chinese province of Guangdong in January 2003 (NCBI, 2004). With a population of 113 million, Guangdong is the most populous province of China, which allowed the virus to spread rapidly through human contact. Public health interventions and containment were further complicated by the huge number of people traveling during the Chinese New Year.
SARS is a type of coronavirus consisting of a single strand of RNA. As with other types of coronavirus, SARS is classified as zoonotic, meaning it was carried by wild animals before transmitting to humans. The wild animals at question were believed to be sold at a local grocery market in Foshan (NCBI, 2004).
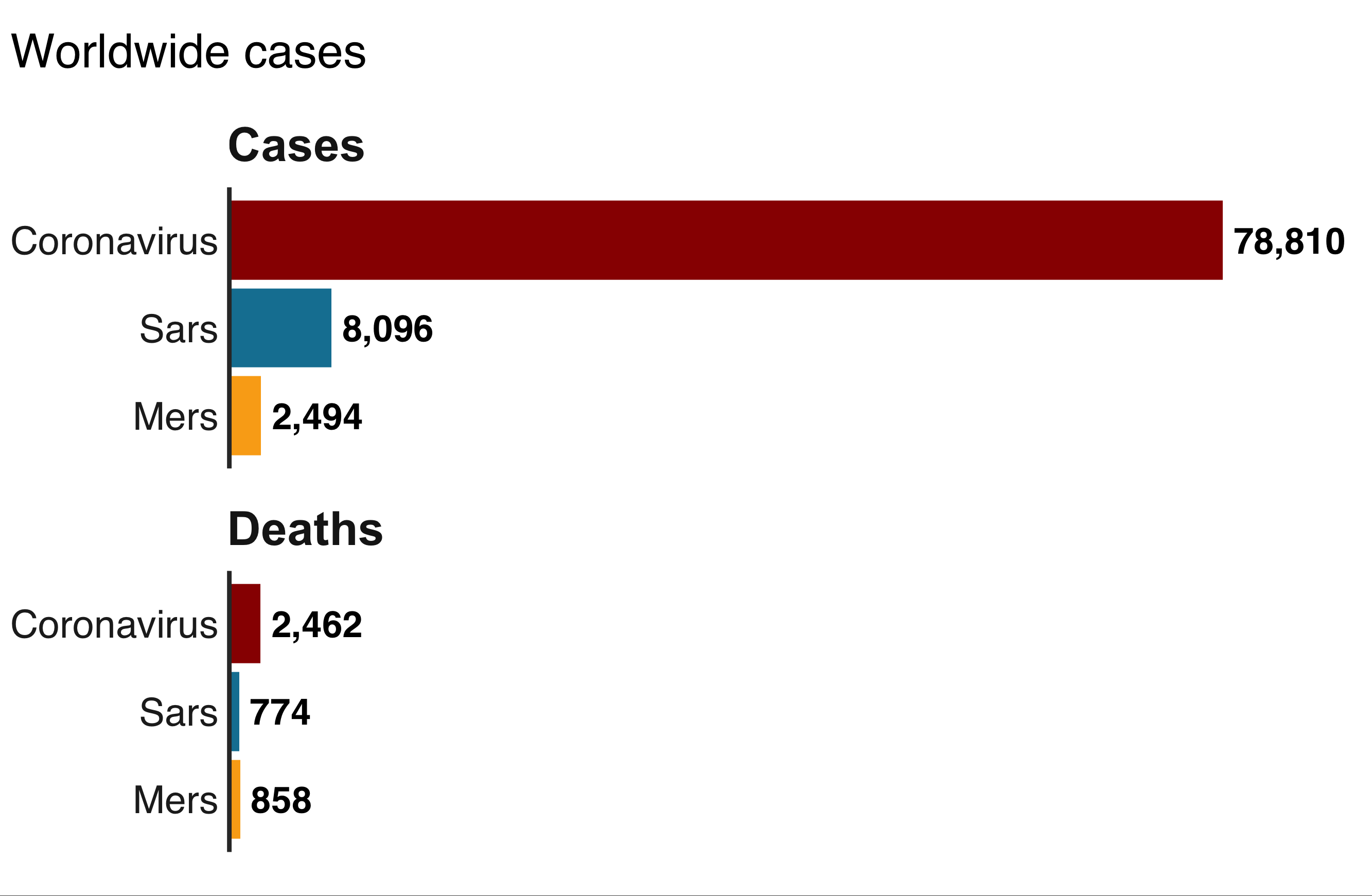
A total of 8098 cases were confirmed worldwide, 774 of which resulted in death. The case fatality rate was thus calculated at 9.6% (WHO, 2004).
Symptoms
Patients most commonly exhibit the following symptoms:
- High fever reaching 38°C and beyond
- Headache, body aches, chills
- Dry, hacking or nonproductive cough appears in the next few days. Dry cough does not involve any mucus secretions or phlegm
- Pneumonia or respiratory distress syndrome develops in most patients, with 20% of them being hooked up to mechanical ventilation (CDC, 2005)
- Hypoxia - decrease in blood oxygen levels due to reduced lung capacity
Less commonly, diarrhea was observed in roughly 20% of patients
Diagnosis
There were three major laboratory techniques used for testing clinical samples:
- RT-PCR, which stands for reverse transcription-polymerase chain reaction, was used to detect and quantify viral RNA in blood or stool samples.
- Serologic testing was used to detect antibodies produced in response to an infectious agent or virus.
- Viral culture was used to supplement the above two diagnostic techniques if needed. A sample of infected tissue or fluid is grown in cell cultures. If the virus is present and proliferates within the cells, morphological changes in the cells will be observed.
Transmission Route
The SARS coronavirus was primarily transmitted through respiratory droplets during short-distance human contact. The droplets are produced from coughing or sneezing, and can travel up to a radius of 3 feet/0.9m (CDC, 2005).
Respiratory droplets deposit on the mucous membranes lining the mouth and nose, where the virus enters the respiratory tract and triggers inflammation. The virus-laden droplets were also known to infect the mucous membrane of the eyes, though not as frequently.
The transmission rate, or R0, of SARS was estimated at around 3, meaning that a single patient can infect 3 other people on average. This puts SARS less infectious than influenza, but similar to smallpox (NCBI, 2004).
Superspreaders
A superspreader is commonly defined as one who spreads the virus to more than 10 people, far beyond the mean R0 of the infectious disease (Stieg, 2020).
At the beginning of the 2003 SARS outbreak, an infected Chinese doctor unwittingly passed on the virus to 12 other people while staying at a hotel in Hong Kong. The 12 people then traveled abroad and spread the infection to Southeast Asia, Western Europe, and North America. The resulting chain reaction accounts for most of the more than 8000 cases worldwide (NCBI, 2004). From Hong Kong, the infection spread to 5 countries within 24 hours, and to more than 30 countries on 6 continents within the following 6 months (WHO, 2003). The rapid spread was made possible by the ease of globalized travel from Hong Kong, a major airline hub, despite the virus having a lower transmission rate (R0) than many other infectious diseases.
Middle East Respiratory Syndrome (MERS)
Overview of the MERS-CoV
MERS stands for Middle East Respiratory Syndrome and it is highly lethal respiratory disease caused by novel single-stranded RNA coronavirus, specifically MERS-CoV (Zumla et al.,2015). This specific coronavirus is a zoonotic virus, transmitted between infected camels and human (Zumla et al.,2015). Until this day, origins of the virus are not fully understood, but theorized that it may have originated in bats and was transmitted to camels (World Health Organization,2019).
Virus first identified in a human in 2012. In June 2012, the sample of MERS- CoV obtained from a Saudi Arabian businessman who died from acute respiratory and renal failure (Memish & Al-Tawfiq, 2014). Middle East Respiratory Syndrome occurs more frequently among person with chronic underlying medical condition or immunosuppression and in health care settings (Zumla et al.,2015).
About 3 or 4 out of every 10 patients with MERS have died (CDC,2019).
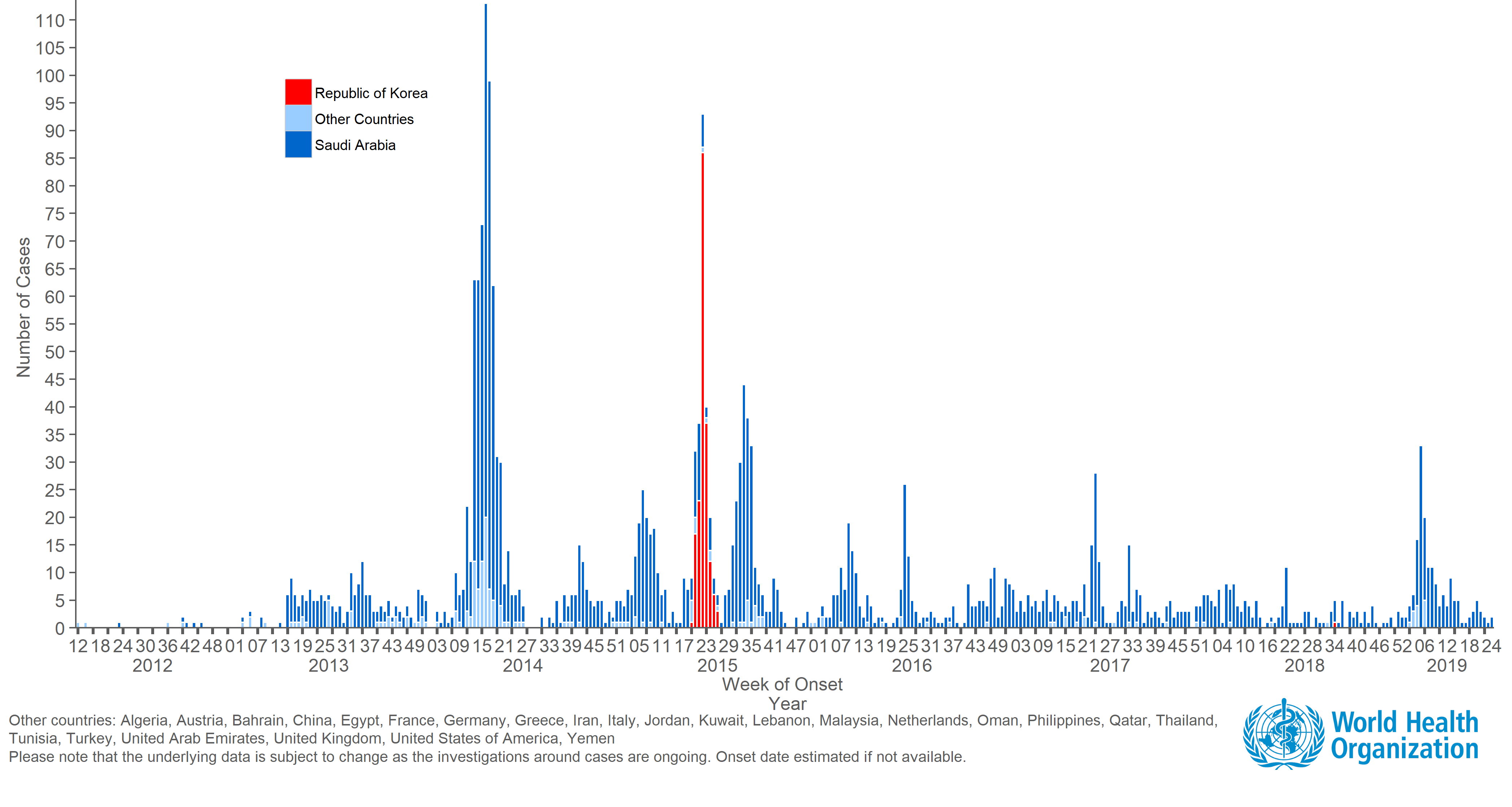
According World Health Organization, there were 2494 cases, 858 deaths and 27 countries have been reported with Middle East Respiratory Syndrome (World Health Organization, 2019).
MERS-CoV has the case- fatality rate of 34.4%, highest among the coronavirus outbreaks (World Health Organization, 2019).
Symptoms
Patients with MERS-CoV commonly present with the following symptoms in early stages:
- Fever above 38 degree Celsius
- Cough, Sore throat, Chills
- Diarrhoea, vomiting (CDC, 2019)
Then later on MERS-CoV infected patients mostly develop pneumonia. Similar to Severe Acute Respiratory Syndrome, third of the patients infected with MERS exhibit gastrointestinal symptoms like vomiting and diarrhoea (Zumla et al.,2015). In severe cases, patients with MERS present with an acute highly lethal pneumonia, renal dysfunction or failure(Zumla et al.,2015). This may require mechanical ventilation and care in the intensive care unit. However, some of the infected patients had mild symptoms or no symptoms at all (World Health Organization, 2019). Patients with diabetes, chronic kidney/ heart/ lung disease, hypertension, obesity, smoking, malignant disease and steroid use present with much severe symptoms and even more exposed to the risk of death (Hajjar et al.,2013).
Diagnosis
To diagnose MERS, real- time reverse transcription PCR test needs to be performed. Middle East Respiratory Syndrome is confirmed by detection of viral nucleic acid or by serology (Zumla et al.,2015). Through real-time reverse-transcription polymerase chain reaction, active viral nucleic acid/ MERS-CoV can be detected. Under CDC standards, MERS patients have to test negative two times for active MERS-CoV under rRT-PCR test to be considered to be negative of MERS (CDC,2019). Serology tests is used to detect previous infection/ anti-bodies to MERS-CoV. However, the purpose of the serology test is for investigational purpose instead of diagnostic purpose. Therefore, to diagnose if the patient has MERS-CoV or not will be dependent on PCR testing (CDC,2019).
Transmission Route
Like SARS, MERS-CoV most likely spreads from an infected patients’ respiratory secretions like coughing and large droplets of bodily fluids (Zumla et al.,2015). Unlike SARS-CoV and Covid-19, MERS-CoV has a different receptor, DDP4, which further leads to transcription in the body (Zumla et al.,2015). All MERS-CoV cases have been linked to countries near the Arabian Peninsula (CDC, 2019). Most patients either lived in the Arabian Peninsula or traveled to Arabian Peninsula. 27 countries have been reported to have cases or MERS-CoV in their countries. However, the reproductive rate (R0) of MERS-CoV was relatively low, R0=0.7. This is substantially lower than the epidemic potential (R0=1)(World Health Organization, 2019). Therefore, the only country that was heavily affected by MERS was South Korea in 2015 with 186 confirmed cases and 38 deaths (largest outbreak outside of Arabian Peninsula)(Kim et al.,2017).
Four different transmission patterns in MERS
Animal to human transmission: about 25% of the cases of MERS are considered to be “primary” cases, animal to human transmission. These are accountable of sporadic cases from having contact with the camels. Camels’ milk may play a role of transmission of MERS-CoV due to 41.7% of 12 milk samples testing positive of MERS-CoV (Memish & Al-Tawfiq, 2014).
Community Outbreaks: Community outbreaks for MERS-CoV was limited to intra-familial transmission. Within family having close contact with each other, potentially sharing food creates a person-to-person transmission(Memish & Al-Tawfiq, 2014).
Health-care-associated transmission: This type of transmission is accountable for a large proportion of MERS-CoV cases. First hospital outbreak was Zarqa, Jordan (Memish & Al-Tawfiq, 2014). This was also accountable for the superspread in South Korea 2015 (Kim et al.,2017).
Travel Related: this type of transmission is accountable for the sporadic events around the different countries. Travel-associated infection was reported in Greece, Jordan, Malaysia and Philippines, United Kingdom, France, Tunisia, Italy, Egypt, United States, Netherlands, and South Korea(Memish & Al-Tawfiq, 2014).
Covid-19
The disease caused by the 2019-2020 coronavirus outbreak has officially been named Covid-19, while the strain of coronavirus is now known as SARS-Cov-2.
Source of Infection
SARS-Cov-2 bears genetic resemblance to SARS and is increasingly believed to be an evolved and mutated version of SARS. Nevertheless, the current SARS-Cov-2 and the 2003 SARS are still confirmed as two distinct strains of coronavirus.
Genetically, SARS-Cov-2 is most closely related to a bat-derived coronavirus sample from Eastern China, at 88% similarity. This indicates that bats are likely the original host of the virus before humans became susceptible, making Covid-19 another zoonotic infectious disease. SARS-Cov-2 is 79% similar to the SARS virus and 50% similar to the MERS virus (Lu et al., 2020).
Clinical manifestation
As the situation unfolds, several medical teams in China were the first to publish clinical characterization research based on sample sizes ranging from 100 to 1000 inpatients. Important findings are summarized as follows:
- Ground-glass opacity observed in CT scans from 50% of patients. Opacity indicates partial filling of the alveoli by fluids, or partial collapse of the alveoli, resulting in reduced lung capacity and respiratory distress (Zhong et al., 2020).
- Lymphopenia in 63% of patients (Zhong et al., 2020)
- Common complications include acute respiratory distress syndrome, acute cardiac injury and secondary infection (Zhong et al., 2020)
- Bilateral pneumonia observed in 75% of patients (Chen et al., 2020)
- Fever, cough, shortness of breath (CDC, 2020)
- Dyspnoea/breathing difficulty in 55% of patients, one week after onset of symptoms (Huang et al., 2020)
Epidemiology
Significant epidemiological features of Covid-19 are summarized as follows:
- Covid-19 has a median incubation period of 3 days, though individual cases range from 1 to 24 days, as reported by top Chinese epidemiologist Dr. Nanshan Zhong, who is widely credited for discovering the SARS virus. However, a new case confirmed on February 22 involves a 70-year-old man who started experiencing symptoms 27 days after getting infected, raising concerns that the mean incubation period could be longer than 14 days (Reuters, 2020).
- Males older than 60 years of age with comorbidities are most susceptible to the disease (Chen et al., 2020).
- The epidemic doubling time, meaning the time it takes for the number of cases to double, is 6.4 days (Wu et al., 2020).
Public Health Interventions
"China Sacrifices a Province to Save the World from Coronavirus"
— Bloomberg News, February 5, 2020
The Chinese government imposed a lockdown on Hubei province, effectively putting 60 million residents into quarantine, the largest yet of its kind known to the world (Bloomberg, 2020). Stringent travel restrictions both within the province and along provincial borders were put into effect starting on January 23, 2020. Body temperature checks are implemented at all highway checkpoints, public venues, and gates to residential compounds within the province.
In the provincial capital Wuhan, a megacity of 11 million people, all travel by air, train, subway, and public buses were suspended until further notice on January 23. Private vehicles were banned from downtown areas starting on January 25. In the neighboring city of Huanggang, which has 7.5 million residents, one person from each family is allowed to shop in the streets every two days.
Covid-19 Talk with Dr. Matthew Miller
Dr. Matter Miller is an Associate Professor of Biochemistry and Biomedical Sciences at McMaster University. Dr. Miller was asked about the current coronavirus outbreak occurring around the world. He does not think that the public should be worried as both, the World Health Organization as well as other health authorities in Canada are hopeful that the spread is limited. When asked about a potential treatment/ cure, he responded with, “The unfortunate reality of these new virus outbreaks is that we don't have a vaccine to protect us against this virus and we don't really have great drugs to treat against this infection But, there are lots of labs around the world that have started attempting to make a vaccine but it is a lengthy process since vaccines have to be tested in model system before advancing to clinical trials.”
Covid-19 vs. SARS
Similarities
Cause & Timing
Both are zoonotic diseases, meaning they spread from wild animals to humans (Achenbach, 2020). Bats were the original host of SARS, from which the virus jumped to civet cats before reaching humans (Hui and Zumla, 2019). For Covid-19, most scientists suspect bats as the original host and pangolins as the intermediary carrier.
Both epidemic outbreaks coincided with Chinese New Year, often dubbed as the world’s largest annual human migration, during which almost 3 billion trips were made across the country in 2019 (CNN, 2019). Population density and mobility are critical to determining if an infectious disease can become an epidemic (Achenbach, 2020)
Transmission
Both infections are transmitted primarily through airborne respiratory droplets, produced when patients cough or sneeze. The droplets usually infect the mucous membranes of the mouth and nose upon contact. However, the respiratory tract is not the only transmission route. Both strains of coronavirus are also able to infect the ocular membrane, specifically the conjunctiva, of people not wearing protective eyewear (Lu et al., 2020).
Clinical Manifestation
SARS and SARS-Cov-2 belong to the same family of virus, coronavirus, which invades the respiratory tract and causes atypical pneumonia. Patients develop breathing difficulties due to inflamed alveoli of the lungs (Cleveland Clinic, 2019). Atypical pneumonia, also known as walking pneumonia, differs from typical pneumonia as it is caused by viral agents or atypical bacteria that lack normal cell structure. Patients with atypical pneumonia experience milder symptoms and resistance to normal antibacterial medications.
Differences
Incubation Period
- SARS: mean incubation period ranges from 1-5 days, which allows for faster diagnosis and medical isolation.
- Covid-19: longer mean incubation period that goes up to 14 days, during which infected individuals do not exhibit any symptoms. More difficult for detection and diagnosis.
- Covid-19: A 70-year-old Hubei resident started experiencing symptoms 27 days after getting infected, raising concerns that the mean incubation period could be longer than 14 days (Reuters, 2020).
Transmission during Incubation Period
Covid-19 carriers can be contagious before showing any symptoms.
- UK superspreader: British businessman Steve Walsh has been linked to 11 confirmed cases in 3 European countries: the UK, France, and Spain. He contracted the virus at a conference in Singapore, then stopped in France and Switzerland before going back to the UK. He was not symptomatic until several days back in the UK (Adam, 2020).
In comparison, there were no reports of SARS patients being contagious before the onset of symptoms (CDC, 2005).
Transmission Rate and Mortality
Covid-19 is less fatal, but likely more contagious.
- R0 (R-naught) is used as a measure of transmission rate that shows the average number of people a single patient can infect.
- The Chinese Academy of Sciences puts the R0 of Covid-19 at 4.08, higher than that of SARS which was approximately 3 (WHO, 2003). However, a study published by the University of Hong Kong estimates the R0 for Covid-19 at 2.68 (Wu et al., 2020).
- As of Feb 12, the case fatality rate of Covid-19 in China is 3.2% (China National Health Commission, 2020), compared to the overall SARS fatality at 9.6% (WHO, 2004).
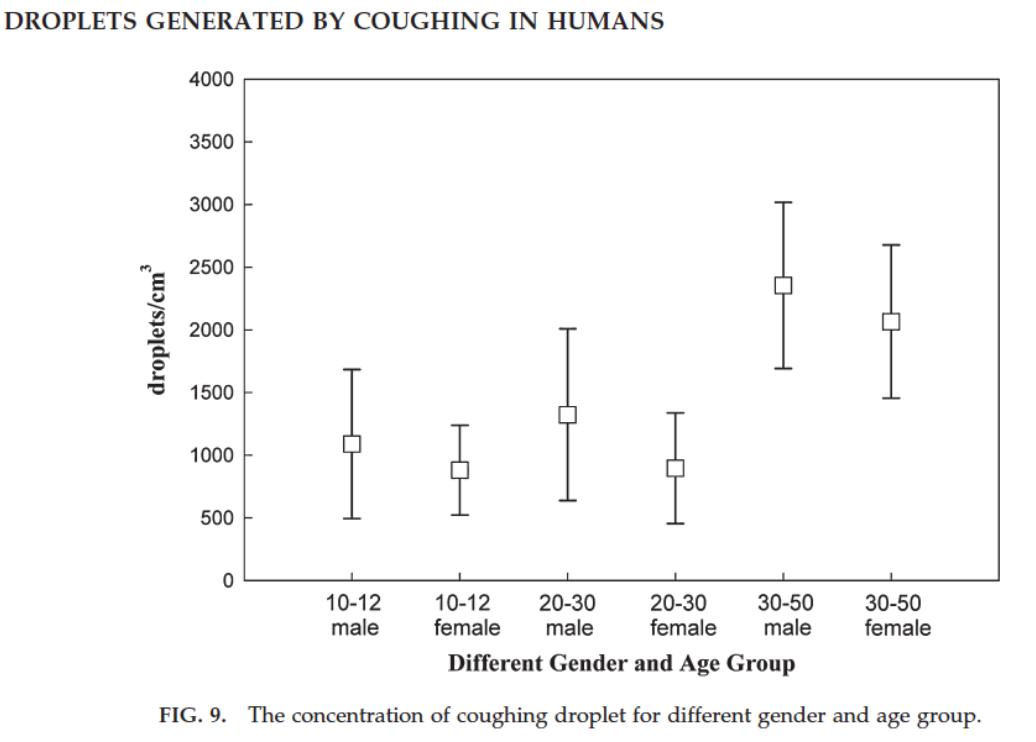
Prevention and Protection
Let’s first look at how coughed droplets travel in air. the average concentration of droplets coughed is 1000-2000 droplets per cm^2 (fig. 7)(Yang, Lee, Chen, Wu, & Yu, 2007). The average size these coughed droplets can range from 0.74 um to 2.12 um (fig. 8)(Yang, Lee, Chen, Wu, & Yu, 2007) which is 60 times the width of a human hair. They can travel for more than 2 meters in a calm environment. While travelling, the coughed droplets containing the viruses, dispersed in air and finally attached to surfaces for a long period of time. The distance that a droplet travelled is dependent on the droplet’s size, smaller droplets scatter in the air, larger droplets are more concentrated.
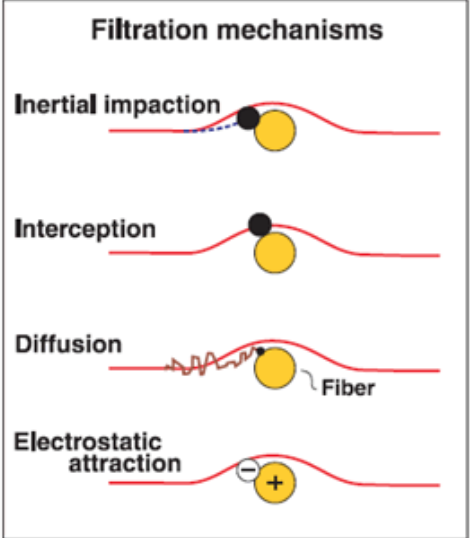
Masks
To prevent contact with these droplets that contain viruses, wearing a mask is certainly a good idea. The multilayer structure of the mask can effectively block large particles, the smaller particles can be attracted to an oppositely charged fiber in the mask (fig. 9).
- Inertial impaction: With this mechanism, particles having too much inertia due to size or mass cannot follow the airstream as it is diverted around a filter fiber. This mechanism is responsible for collecting larger particles.
- Interception: As particles pass close to a filter fiber, they may be intercepted by the fiber. Again, this mechanism is responsible for collecting larger particles.
- Diffusion: Small particles are constantly bombarded by air molecules, which causes them to deviate from the airstream and come into contact with a filter fiber. This mechanism is responsible for collecting smaller particles.
- Electrostatic attraction: Oppositely charged particles are attracted to a charged fiber. This collection mechanism does not favor a certain particle size.
(Brosseau & Brosseau 2009)
If we plot the particle diameter on x-axis, and the filtration efficiency on the y-axis, the filtration effects of masks exhibit as U-shaped curves (fig. 10). The hardest particles to filter are the ones around 0.3 micrometers. Which is why most masks use 0.3 micrometers as a performance indicator(Brosseau & Brosseau 2009).
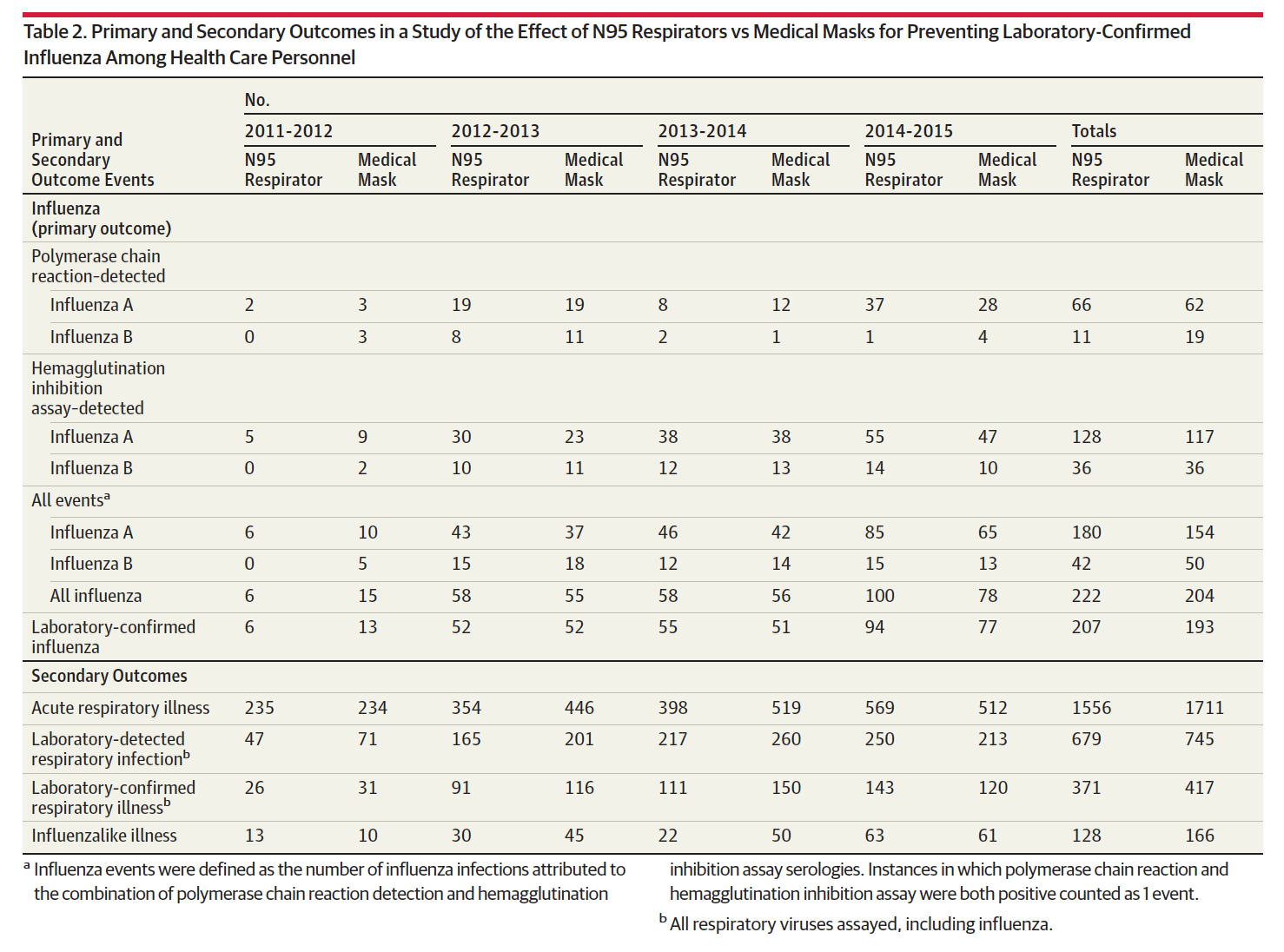
To protect against most coughed droplets, a regular medical mask is enough. In a randomized clinical trial with more than 2800 influenza health care providers, the flu infection rates of those who wore N95 masks and regular medical masks actually showed no significant differences, if compare the total outcomes of both masks in fig. 11. (Radonovich, et al., 2019).
Personal Hygiene
What’s more important than whether you wear a N95 or not, is did you wash your hands? Washing hands are critical because your hands can carry live coronavirus from the contaminated surfaces. When you rub your eyes and pick your nose with your hands, the viruses can complete the infection. So, please take your time to wash your hands and avoid touching eyes, nose and mouth (World Health Organization, 2020).
Treatment
During the SARS epidemic in 2003, hospitalized patients received the same treatment as recommended for severe atypical pneumonia (CDC, 2005). Antiviral medications are sometimes given to reduce the swelling of the lungs but there are no studies that prove this is effective for every individual affected by SARS. No effective pharmacological interventions against the virus exists at this time. However, antiviral medications were later developed to combat the MERS outbreak in 2012.
Remdesivir
Remdesivir is known to be an effective drug against the coronavirus, specifically the one related to the Middle Eastern Respiratory Syndrome (MERS-CoV). Studies in the past have shown that Remdesivir prevented MERS in monkeys when it was administered before exposing the monkeys to the virus. Furthermore, when the drug was administered after the infection, it reduced the severity of the disease, virus replication and the amount of damage to the lungs (Wit et al., 2020).
Remdesivir functions by inhibiting the replication of MERS-CoV in respiratory tissues and preventing the formation of lung lesions. In vitro studies involving mice infected with the hepatitis virus suggests that Remdesivir works against the coronavirus by interfering with the viral polymerase responsible for replication to occur (Wit et al., 2020).
Lopinovir and Ritonavir
Lopinavir and Ritonavir are protease inhibitors that blocks key enzymes that are necessary for viral replication (Coronavirus Treatment- HIV Protease Inhibitors, n.d.). The combination of these drugs are normally used to treat HIV/AIDS, however, current in vitro and animal studies have led researchers to believe they may be effective against MERS-CoV (Arabi et al., 2018).
Conclusion
In conclusion, coronavirus is an ongoing concern. Although treatments are being research, it will be a long way until a solution is reached. Therefore, preventative methods should be taken seriously. With the current outbreak slowly becoming a concern, it is crucial to wash hands thoroughly and maintain overall personal hygiene. The best way to receive immediate medical care is to get treated early for symptoms.
References
Advice for public. (n.d.). Retrieved from https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public
Arabi, Y. M., Alothman, A., Balkhy, H. H., Al-Dawood, A., AlJohani, S., Al Harbi, S., Kojan, S., Al Jeraisy, M., Deeb, A. M., Assiri, A. M., Al-Hameed, F., AlSaedi, A., Mandourah, Y., Almekhlafi, G. A., Sherbeeni, N. M., Elzein, F. E., Memon, J., Taha, Y., Almotairi, A., … And the MIRACLE trial group. (2018). Treatment of Middle East Respiratory Syndrome with a combination of lopinavir-ritonavir and interferon-β1b (MIRACLE trial): Study protocol for a randomized controlled trial. Trials, 19(1), 81. https://doi.org/10.1186/s13063-017-2427-0
Arabi, Y. M., Balkhy, H. H., Hayden, F. G., Bouchama, A., Luke, T., Baillie, J. K., Al-Omari, A., Hajeer, A. H., Senga, M., Denison, M. R., Nguyen-Van-Tam, J. S., Shindo, N., Bermingham, A., Chappell, J. D., Van Kerkhove, M. D., & Fowler, R. A. (2017). Middle East Respiratory Syndrome. The New England journal of medicine, 376(6), 584–594. https://doi.org/10.1056/NEJMsr1408795
Brosseau, Lisa Berry, and Roland Berry Brosseau. “N95 Respirators and Surgical Masks.” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, 14 Oct. 2009, blogs.cdc.gov/niosh-science-blog/2009/10/14/n95/.
Centers for Disease Control and Prevention. (2020, January 10). Coronavirus. Retrieved from https://www.cdc.gov/coronavirus/types.html
Coronavirus – Simple Precautions to Take care for loved ones. (2020, February 7). My22BMI. https://my22bmi.com/coronavirus-simple-precautions-to-take/
Coronavirus Treatment- HIV Protease Inhibitors. (n.d.). Retrieved February 26, 2020, from http://www.natap.org/2020/newsUpdates/020420_02.htm
Donovan, M. (2020, January 24). Explaining the coronavirus. Retrived from https://brighterworld.mcmaster.ca/articles/coronavirus-explanations-from-an-expert/.
Hajjar, S. A., Memish, Z. A., & Mcintosh, K. (2013). Middle East Respiratory Syndromw Coronavirus (MERS-CoV): A Perpetual Challenge. Annals of Saudi Medicine, 33(5), 427–436. doi: 10.5144/0256-4947.2013.427
Kim, K., Tandi, T., Choi, J., Moon, J., & Kim, M. (2017). Middle East respiratory syndrome coronavirus (MERS-CoV) outbreak in South Korea, 2015: epidemiology, characteristics and public health implications. Journal of Hospital Infection, 95(2), 207–213. doi: 10.1016/j.jhin.2016.10.008
Middle East respiratory syndrome coronavirus (MERS-CoV). (n.d.). Retrieved February 24, 2020, from https://www.who.int/en/news-room/fact-sheets/detail/middle-east-respiratory-syndrome-c oronavirus-(mers-cov)
Memish, Z., & Al-Tawfiq, J. (2014). Middle East respiratory syndrome coronavirus: epidemiology and disease control measures. Infection and Drug Resistance, 281. doi: 10.2147/idr.s51283
MERS Symptoms & Complications. (2019, August 2). Retrieved February 24, 2020, from https://www.cdc.gov/coronavirus/mers/about/symptoms.html
MERS Transmission. (2019, August 2). Retrieved from https://www.cdc.gov/coronavirus/mers/about/transmission.html
Otter, J., Donskey, C., Yezli, S., Douthwaite, S., Goldenberg, S., & Weber, D. (2016). Transmission of SARS and MERS coronaviruses and influenza virus in healthcare settings: the possible role of dry surface contamination. Journal of Hospital Infection, 92(3), 235–250. doi: 10.1016/j.jhin.2015.08.027
Radonovich, L. J., Simberkoff, M. S., Bessesen, M. T., Brown, A. C., Cummings, D. A. T., Gaydos, C. A., … Perl, T. M. (2019). N95 Respirators vs Medical Masks for Preventing Influenza Among Health Care Personnel. Jama, 322(9), 824. doi: 10.1001/jama.2019.11645
Wit, E. de, Feldmann, F., Cronin, J., Jordan, R., Okumura, A., Thomas, T., Scott, D., Cihlar, T., & Feldmann, H. (2020). Prophylactic and therapeutic remdesivir (GS-5734) treatment in the rhesus macaque model of MERS-CoV infection. Proceedings of the National Academy of Sciences. https://doi.org/10.1073/pnas.1922083117
WHO MERS-CoV Global Summary and Assessment of Risk (2018.). Retrieved from https://www.who.int/csr/disease/coronavirus_infections/archive_updates/en/
World Health Organization. (2020, February). Coronavirus. Retrieved from https://www.who.int/health-topics/coronavirus
Yang, S., Lee, G. W., Chen, C.-M., Wu, C.-C., & Yu, K.-P. (2007). The Size and Concentration of Droplets Generated by Coughing in Human Subjects. Journal of Aerosol Medicine, 20(4), 484–494. doi: 10.1089/jam.2007.0610
Zhu, S., Kato, S., & Yang, J.-H. (2006). Study on transport characteristics of saliva droplets produced by coughing in a calm indoor environment. Building and Environment, 41(12), 1691–1702. doi: 10.1016/j.buildenv.2005.06.024
Zumla, A., Hui, D. S., & Perlman, S. (2015). Middle East respiratory syndrome. The Lancet, 386(9997), 995–1007. doi: 10.1016/s0140-6736(15)60454-8