This is an old revision of the document!
Table of Contents
Osteoporosis
Introduction
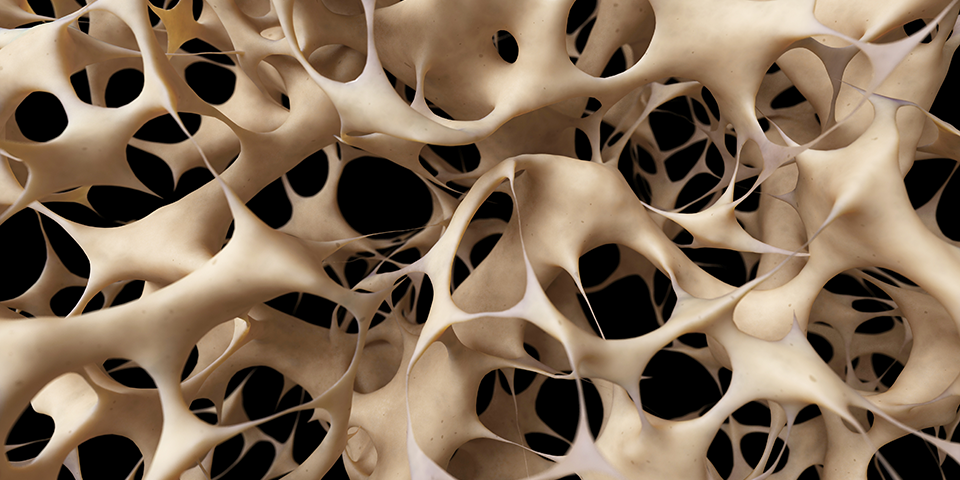
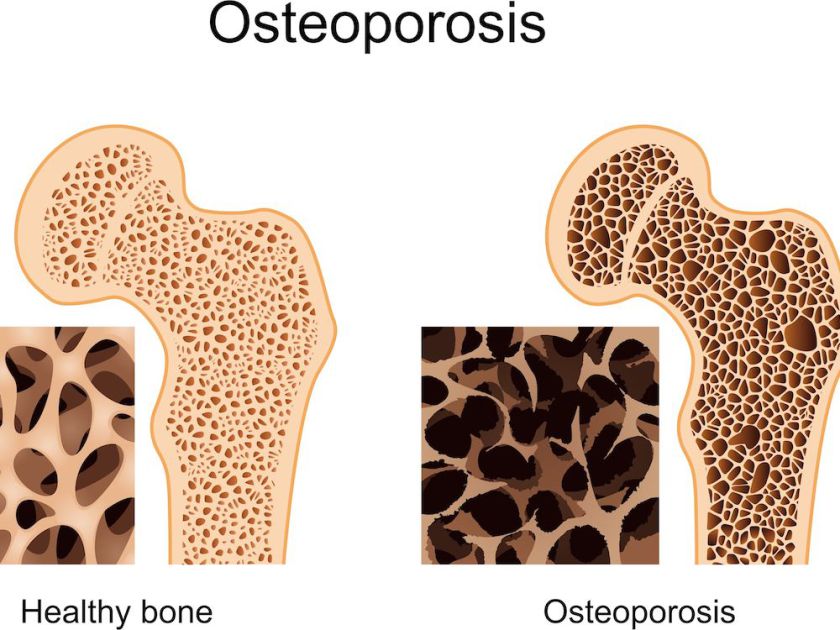
Osteoporosis is a bone disease characterized by a deterioration of bone tissue and low bone density which results in the weakening of bones. This systematic impairment of bone mass, strength and microarchitecture leads to an increasing prevalence of breaks and fractures (Rachner et al., 2011). The term osteoporosis is derived from “porous bones”, from the Greek: οστούν/ostoun meaning “bone” and πόρος/poros meaning “pore”.
The human skeleton is composed of 206 bones. Bones are composed of tissue, proteins, minerals and vitamins. The formation, modelling and breakdown of bone is regulated by bone cells such as osteoblasts, and osteoclasts (International Osteoporosis Foundation, 2017). Osteoblasts are the cells responsible for producing and secreting bone matrix proteins for bone synthesis and remodelling, while osteoclasts are responsible for bone breakdown through the reabsorption. When the activity of osteoclasts surpasses the bone formation by osteoblasts, the bones become brittle and porous leaving them susceptible to fractures(International Osteoporosis Foundation, 2017). As the population ages, osteoporosis poses an increasing social and medical demand on individuals, caregivers and healthcare providers. Currently, prevention, detection and management are instrumental in managing this condition (Cosman et al., 2014).
History
The discovery of the correlation between age-related deterioration in bone mass and density and the resulting risk in fractures can be dated back to the writings of 18th century British surgeon, Astley Cooper, who observed the “thin and spongy texture” of the bones of older patients (Grob, 2014). Furthermore, skeletal remains that have been studied by anthropologists have shown decreased bone density associated with chronic malnutrition, which is an identified risk factor of the bone disease (Grob, 2014).
Epidemiology
1 in 3 women and 1 in 5 men in Canada suffers from osteoporosis 2 million Canadians Osteoporosis usually begin in mid-30s Responsible for more than 1.5 million fractures annually, including 300,000 hip fractures, approximately 700,000 vertebral fractures, 250,000 wrist fractures, and more than 300,000 fractures at other sites.
Risk Factors
Chronological disease Canada Younger adults (age < 50 years):
Fragility fracture (breaking a bone as a result of a minor accident) Long term use of glucocorticoids such as prednisone Hypogonadism or premature menopause (age < 45 years) Having other disorders strongly associated with rapid bone loss and/or fracture such as rheumatoid arthritis, malabsorption syndrome, and primary hyperparathyroidism Older adults (age > 50 years):
Being 65 years or older Clinical risk factors for fracture (menopausal women, men age 50 to 64 years): Fragility fracture (breaking a bone as a result of a minor accident) Long term use of glucocorticoids such as prednisone Having a parent who had a hip fracture Having a spine fracture or low bone mass identified on x-ray Being a smoker High alcohol intake (greater than or equal to 3 units per day on a consistent basis) Low body weight (less than 60 kg or 132 lbs) or major weight loss(present weight is more than 10% below your weight at age 25) Having other disorders strongly associated with rapid bone loss and/or fracture as mentioned above
Osteoporosis Canada Men are more likely than women to suffer from hip fractures ( 37% to 28%) Age, sex, vertebral compression fracture, fragility fracture after age 40, either parent has had a hip fracture, >3 months use of glucocorticoid drugs, medical conditions that inhibit absorption of nutrients and other medical conditions or medications that contribute to bone loss.
Signs and Symptoms
Individuals may not realize that they have osteoporosis until a fracture of the bone occurs. As the most common areas for fractures include the wrist, spine, shoulder, and hip, symptoms can include:
- Stooped posture overtime
- Bone pain or tenderness
- Rounding of the back called kyphosis
- Height loss overtime
(Canadian Cancer Society, 2018)
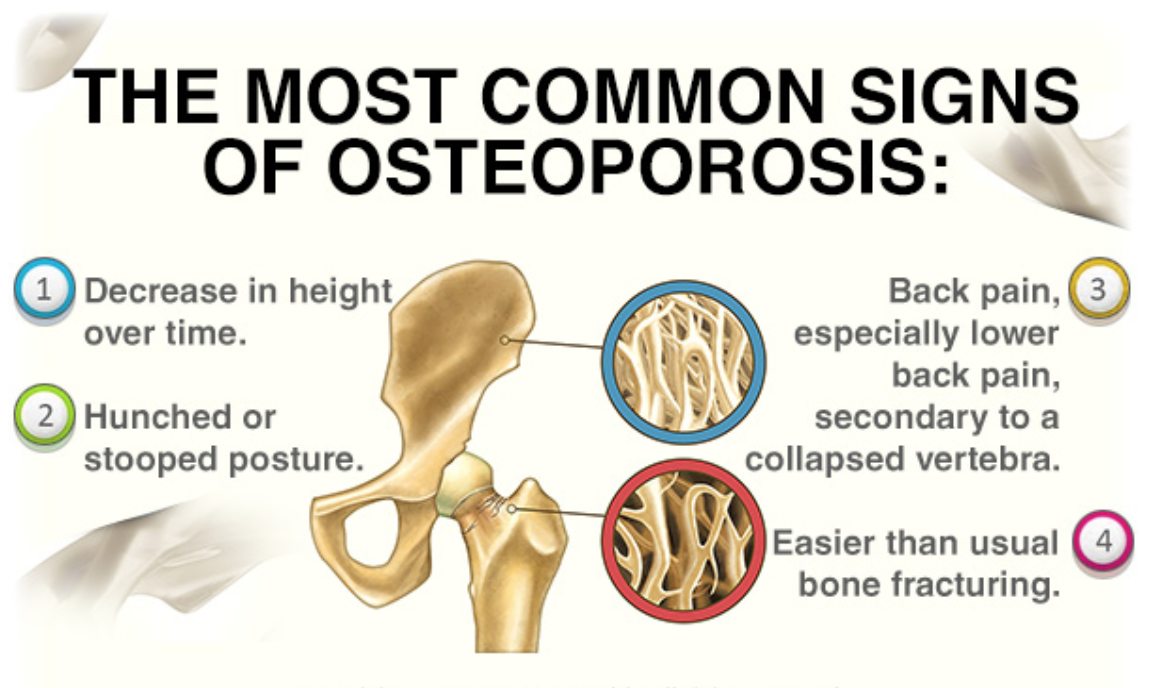 Figure _: Four common signs of osteoporosis that is prevalent such as decrease in height overtime, hunched or stooped posture, back pain, and easier than usual bone fracturing.
Figure _: Four common signs of osteoporosis that is prevalent such as decrease in height overtime, hunched or stooped posture, back pain, and easier than usual bone fracturing.
Areas of Fractures
The most common area of fracture that occurs is the fracture of the spine. The range of pain can vary from mild to extreme as this fracture can occur from coughing, sneezing, or more serious situations such as a fall (Gardner, Demetrakopoulos, Shindle, Griffih, and Lane 2006). It is indicated that two-thirds of broken bones in the spine occur without any pain and can be indicated if the healthcare provider believes that height is loss within an individual (Osteoporosis Canada, 2018). Kyphosis occurs within the loss of height when there is an excessive outward curve with the upper back. Some people may experience constant pain since the ligaments and tendons are strained. It can also lead to reduced space in the internal organs making it more difficult for some individuals to breathe or eat (National Osteoporosis Foundation, 2018).
Another common area of fracture occurs in hip fractures are considered the most common fracture that occurs during osteoporosis (Gardner, Demetrakopoulos, Shindle, Griffih, and Lane 2006). This commonly occurs within individuals in their late 70s or 80s and those who experience a hip fracture are at high risk to develop fractures in other areas (Osteoporosis Canada, 2018). It also causes the highest cost associated and most often a hip replacement is needed in order to allow the individual to regain function (Gardner, Demetrakopoulos, Shindle, Griffih, and Lane 2006). Hip fractures occur due to the femoral head being supported by a thin structure which is called the femoral neck. The femoral neck is prone for fracture in those who have bone disorders including osteoporosis (Metcalfe, 2008).
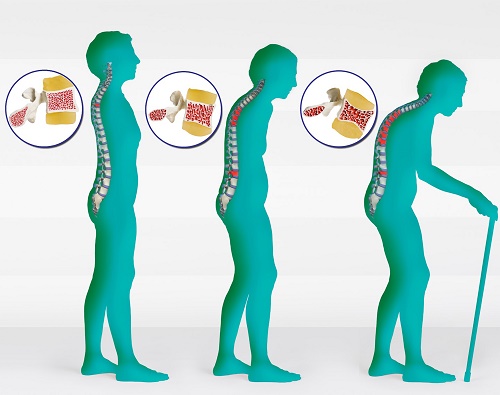 Figure 1: An image showing the effects of having one or more fractures in osteoporosis .
Figure 1: An image showing the effects of having one or more fractures in osteoporosis .
Diagnosis
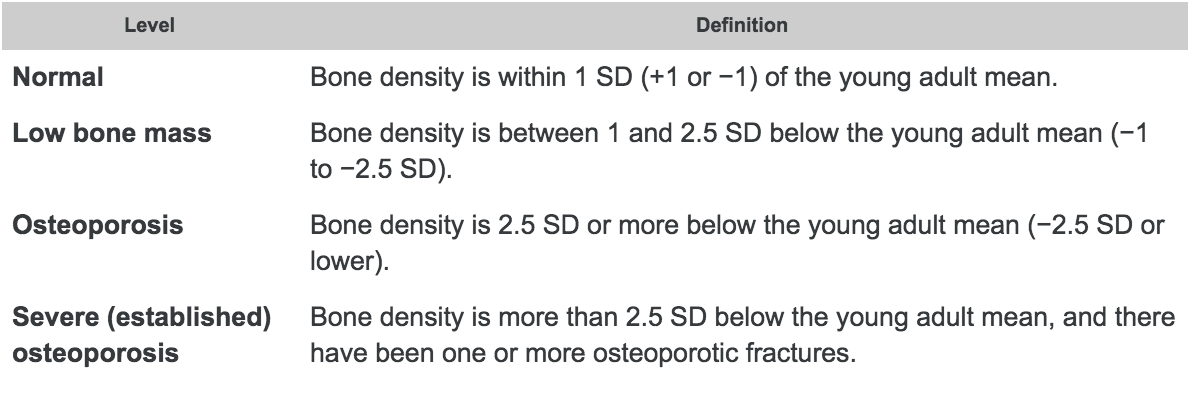
The bone mass density, also known as BMD, is the primary test that can be used to determine the bone strength using a dual X-ray absorptiometry. The scanned bone from either the hip or spine from an individual can determine the bone density to determine the diagnosis as well as any future fracture risks (Sozen, Ozisik, and Calik 2017). The World Health Organization (WHO) presents that osteoporosis is determined when an individual has 2.5 standard deviation below the average using a T-score. This can be performed from knowing the difference between the patient’s BMD and the average to compare with the severity of the diagnosis (Sozen, Ozisik,and Calik 2017). The results are usually compared to a healthy 30-year old adult’s bone mineral density. Therefore, a lower BMD number will indicate a higher risk of a fracture (National Resource Center, 2015).
Figure __: A table demonstrating the comparison of standard deviations created by the World Health Organization (WHO).
Screening & Measuring Tools
Dual-energy x-ray absorptiometry (DEXA) is a method that can be performed on different areas to determine osteoporosis with a low radiation dose. This method consists of two energies where the x-ray goes across the desired area. Areas often included are the lumbar spine and proximal femur. However, if these areas are unavailable, the forearm can also be used to scan for BMD measurement (Ramos et al., 2011).
Another method used to determine osteoporosis is determined using blood tests or bone biopsies. Blood tests are able to indicate certain proteins such as alkaline phosphatase. An individual with a higher amount of alkaline phosphatase has a higher indication with certain bone diseases. Calcium levels in the blood can also indicate if an individual has enough calcium intake (Institute for Quality and Efficiency in Health Care, 2017).
Pathophysiology
Osteoporosis is known defined as having a low bone mass and the deterioration of bone tissue which leads to a high incidence of bone fracture for individuals. The likelihood of obtaining osteoporosis usually increases with age. The mechanism and rate for which older individuals lose bone, positively correlates with calcium deficiency.
There are two main types of osteoporosis; primary and secondary. Primary osteoporosis is caused by an age-related bone loss, typically occurring to men that are above the age of 70. Secondary osteoporosis is when bone mass is lost due to onset of certain diseases, bad lifestyle, etc. Some common causes of secondary osteoporosis include cigarette smoking, alcoholism, and low testosterone levels in men.
This calcium deficiency leads to secondary hyperparathyroidism; elevated PTH levels in the blood. This stimulates osteoclast activity within the bone resulting in more bone resorption than normal.
The reason for why osteoporosis is usually seen in older individuals is due to a couple of factors. Aging skin along with decreased sun exposure, reduces the conversion of a precursor of vitamin D (7-dehydrocholesterol) to Vitamin D3. Ultimately, this causes Vitamin D insufficiency which reduces the amount of calcium being absorbed.
In females, menopause usually leads to the loss of bone mass. When menopause occurs, the hormone progesterone is deficient. Some supporting data from 1990 suggests that progesterone plays the role of being a bone formation-stimulating hormone. Although supported, nothing is concrete as this hormone regulated by estrogen, thereby including multiple confounding variables.
In males studies have been done linking bone mineral densities to testosterone levels. When comparing the estrogen level of males, the group of males with the highest levels had the highest bone mineral density, while the group of males with the lowest estrogen levels had the highest risk of a hip fracture. In contrast, when measuring levels of testosterone, there was no significant difference in hip fracture risk when looking at hypogonadal men versus eugonadal men. This supports the fact that the hormone estrogen plays more of a role in bone health in comparison to testosterone.
Treatments - Prevention & Management
There are no true cures for osteoporosis, so the goal of treatments of the disease is the prevention of bone fractures, minimizing bone loss, or increasing bone strength. It is very difficult to rebuild bone that is affected by the disease, and so prevention is just as important as treatments. There are 3 main ways to treat and prevent osteoporosis; lifestyle changes, drugs that minimize bone loss and increase bone strength, and drugs that increase bone formation (Kling et al., 2014).
Lifestyle
Many lifestyle changes can be put into effect in order prevent and manage osteoporosis. Exercise is an example of a lifestyle change that can be very beneficial. The benefit does not significantly increase bone density, but rather decreases the chance of falls and related injuries, most likely due to improved balance and muscle strength. Researchers have not determined the most effective types of exercise and so recommendations include weight bearing exercise such as walking. Smoking is another lifestyle choice that can worsen the effects of osteoporosis(Sözen et al., 2017).
It has been found that one pack of cigarettes per day can lead to a loss of 5-10% of bone mass. They also decrease estrogen levels and can lead to early bone loss in women before menopause, along with an earlier onset of menopause. Postmenopausal smoking is also linked with increased risk of osteoporosis (Kling et al., 2014).
Supplements can be useful for treatment of osteoporosis. Building strong bones requires a certain amount of calcium intake in both males and females. The amount of calcium intake recommended does increase with age, and is highest for postmenopausal women. Vitamin D is another important molecule that is needed for healthy bone density and strength. Similar to calcium, vitamin D alone is not enough for osteoporosis treatment, and should be used alongside other treatments(Kling et al., 2014).
In postmenopausal women specifically, estrogen hormone therapy has been effective at preventing bone loss, preventing fractures, and increasing bone strength. Estrogen used for treatment can be administered orally, or even as a skin patch (Jr, n.d).
Drugs and Medication
As of now, the most effective drugs for osteoporosis are antiresorptive agents, meaning they decrease the amount of calcium removed from bones. Since bones are dynamic and constantly being remodelled, and osteoporosis results when bone resorption is higher than bone rebuilding, these medications inhibit the removal of bone so bone rebuilding is favoured. Many antiresorptive agents are available including alendronate, risedronate, raloxifene and others (Lewiecki, 2004).
Bisphosphonates are a class of antiresorptive drugs that are used to decreases risks of fractures of hip, wrist, and spine. These class of drugs are all administered orally to reduce adverse side effects, and to enhance the absorption of the medicine. They are taken in the morning and are taken with water to increase absorption. They can also be administered intravenous to avoid possible stomach problems(Lewiecki, 2004).
Alendronate (Fosamax) is an example of a bisphosphonate drug. It is effective treatment for postmenopausal osteoporosis as well as with glucocorticoid induced osteoporosis. This drug, similar to other bisphosphonates increases bone density and reduces various possible fractures. It is taken orally once a week for postmenopausal osteoporosis and is also the first drug used for increasing bone density in males with osteoporosis. This drug as all others does have a few side effects. This includes irritation of the esophagus or even inflammation of the esophagus. Differences in the chemical makeups of the other bisphosphonate drugs is what allows for certain side effects to be avoided(Gronholz, 2008).
Zoledronate (Reclast) is an intravenous administered bisphosphonate that is given once a year. It is able to effectively strengthen bones along with preventing both spinal and non-spinal fractures. As with all medications, side effects of this drug may result in muscle and joint aches, and so mild pain killers are given following treatment. This drug is used mainly to prevent postmenopausal osteoporosis and to increase bone mass in males suffering the disease(Gronholz, 2008).
Conclusion
Osteoporosis is set to become a major health concern with an ageing population. Scientists have identified human stem cells that develop into the bone, cartilage, and other tissues that make up the body’s skeleton This will one day help doctors repair or replace joint cartilage, heal broken bones more quickly, and build up bone in osteoporosis patients. Additionally, a new genetic screen may predict a person’s future risk of osteoporosis and bone fracture and may allow for more preventative measures.
References
Bone Mass Measurement: What the Numbers Mean (2018). | NIH Osteoporosis and Related Bone Diseases National Resource Center. Cosman, F., De Beur, S. J., LeBoff, M. S., Lewiecki, E. M., Tanner, B., Randall, S., & Lindsay, R. (2014). Clinician’s guide to prevention and treatment of osteoporosis. Osteoporosis international, 25(10), 2359-2381.
Gardner, M., Demetrakopoulos, D., Shindle, M., Griffith, M. and Lane, J. (2006). Osteoporosis and Skeletal Fractures. HSS Journal, 2(1), pp.62-69.
Government of Canada. (2016, September 16). Osteoporosis Awareness Month – Exposing The Bone Thief. Retrieved from https://infobase.phac-aspc.gc.ca/datalab/osteo-blog-en.html?=undefined&wbdisable=true
Grob, G. N. (2014). Aging Bones: A Short History of Osteoporosis. JHU Press.
Gronholz, M. J. (2008). Prevention, diagnosis, and management of osteoporosis-related fracture: a multifactoral osteopathic approach. The Journal of the American Osteopathic Association, 108(10), 575-585.
Hip Fractures. (n.d.). Retrieved from https://osteoporosis.ca/bone-health-osteoporosis/living-with-the-disease/after-the-fracture/what-to-expect-from-some-specific-types-of-fracture/hip-fractures/
Jr, W. C. (n.d.). Osteoporosis Causes, Symptoms, Treatment & Diet. Retrieved from https://www.medicinenet.com/osteoporosis/article.htm#what_is_the_treatment_for_osteoporosis_and_can_osteoporosis_be_prevented
Kenny, A. M., & Prestwood, K. M. (2000). Osteoporosis: pathogenesis, diagnosis, and treatment in older adults. Rheumatic Disease Clinics of North America, 26(3), 569-591.
Kling, J. M., Clarke, B. L., & Sandhu, N. P. (2014). Osteoporosis prevention, screening, and treatment: a review. Journal of women's health, 23(7), 563-572.
Lewiecki, E. M. (2004). Management of osteoporosis. Clinical and Molecular Allergy, 2(1), 9.
Lorente-Ramos, R., Azpeitia-Armán, J., Muñoz-Hernández, A., García-Gómez, J., Díez-Martínez, P. and Grande-Bárez, M. (2011). Dual-Energy X-Ray Absorptiometry in the Diagnosis of Osteoporosis: A Practical Guide. American Journal of Roentgenology, 196(4), pp.897-904. Metcalfe, D. (2008). The pathophysiology of osteoporotic hip fracture. McGill Journal of Medicine : MJM, 11(1), 51–57.
National Osteoporosis Foundation. (2018). Osteoporosis and Your Spine - National Osteoporosis Foundation. [online] Available at: https://www.nof.org/patients/fracturesfall-prevention/exercisesafe- Osteoporosis - Canadian Cancer Society. [online] Available at: http://www.cancer.ca/en/cancer-information/diagnosis-and-treatment/managing-side-effects/osteoporosis/?region=on#ixzz5QdWol1aw [Accessed 24 Sep. 2018]. movement/osteoporosis-and-your-spine/ [Accessed 24 Sep. 2018]. Osteoporosis Canada. (2018, September). KNOW YOUR RISK. Retrieved from https://osteoporosis.ca/
Osteoporosis in Men. (n.d.). Retrieved from https://www.bones.nih.gov/health-info/bone/osteoporosis/men#b
Paul Lips, Tu Duong, Anna Oleksik, Dennis Black, Steven Cummings, David Cox, Thomas Nickelsen; A Global Study of Vitamin D Status and Parathyroid Function in Postmenopausal Women with Osteoporosis: Baseline Data from the Multiple Outcomes of Raloxifene Evaluation Clinical Trial, The Journal of Clinical Endocrinology & Metabolism, Volume 86, Issue 3, 1 March 2001, Pages 1212–1221, https://doi.org/10.1210/jcem.86.3.7327
PubMed Health. (2018). Understanding tests used to detect bone problems. [online] Available at: https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0072597/ [Accessed 16 Sep. 2018]
Rachner, T. D., Khosla, S., & Hofbauer, L. C. (2011). Osteoporosis: now and the future. The Lancet, 377(9773), 1276-1287.
Spine Fractures. (n.d.). Retrieved from https://osteoporosis.ca/bone-health-osteoporosis/living-with-the-disease/after-the-fracture/what-to-expect-from-some-specific-types-of-fracture/spine-fractures/
Sozen, T., Ozisik, L. and Calik Basaran, N. (2017). An overview and management of osteoporosis. European Journal of Rheumatology, 4(1), pp.46-56.
Wark, J. D. (1993). 8 Osteoporosis: pathogenesis, diagnosis, prevention and management. Baillière's clinical endocrinology and metabolism, 7(1), 151-181.