This is an old revision of the document!
Table of Contents
Multiple Sclerosis
<style justify> Multiple Sclerosis (MS) is an autoimmune disease affecting the central nervous system. The disease specifically affects the myelin and as a result inflammation occurs and the myelin is damaged. Myelin performs the crucial role of nerve impulse through nerve fibers. If myelin is damaged then there will be a decrease in the transmission of nerve impulses. When the damage is significant then scar tissue will replace the myelin. The symptoms of MS vary for each individual, some include fatigue, pain, bladder problems, walking problems, cognitive difficulties and optic neuritis. Canada currently has the highest rate of MS with approximately 100,000 Canadians currently diagnosed (Multiple Sclerosis Society of Canada, 2016). </style>
<br> <br> <br>
Causes
There currently is no known cause for the affliction of MS; however the general consensus is that which follows both environmental as well as genetic factors contributing to the emergence of the disease (Dyment et al. 2004). There is a variance in the amount of environmental factors thought to influence the presence of MS. Many theories attempt to analyze different combinations of risk factors with hopes of coming to a conclusion which explains the emergence of MS; however none have been successful (Dyment et al. 2004).
Some of the most prominent environmental risk factors include an array of microbes (Ascherio & Munger, 2007). Microbes vary depending on geographic region and it is thought that a change in exposure to a set of microbes native to a specific location is what increases the risk of developing MS (Ascherio & Munger, 2007). A theory which further investigates this ideology is that of the hygiene hypothesis. It states that in early life contact with infections are beneficial to the individual, with later exposure to high risk microbes resulting in the development of MS further along in life (Compston & Coles, 2008). Therefore an individual who has recently moved to an area with high risk microbes is more likely to acquire MS due to its novelty to their immune system. In addition to microbes there is evidence in support of a virus as a candidate for causing MS (Ascherio & Munger, 2007). An example of this would be the human herpes virus (hhv), more specifically hhv-4, which is one of the 8 different known strains of hhv (Gildan, 2005). The majority of the human population has been exposed to at least one strain of the hhv, with one of the most common being the Varicella zoster virus which causes chickenpox or shingles (Gildan, 2005). Studies show that individuals who have not previously been infected with hhv-4, otherwise known as the Epstein-Barr virus are at less of a risk of acquiring MS compared to those who have previously contracted it (Gildan, 2005). Furthermore according to the hygiene hypothesis individuals exposed to the Epstein-Barr virus as youths have a reduced risk of being affected by MS as opposed to the higher risk experienced by adults since it is their first interaction with the causative virus in a relatively later stage in life which acts as a trigger (Gildan, 2005).
While believed by many, MS is not categorized as a hereditary disease (Dyment et al. 2004). Instead its connection with genetics lies within the chance of genetic variation leading to increase risk in developing the disease (Ascherio & Munger, 2007). Due to the similarity of genetic expression found among related individuals, the probability of developing MS is increased when comparing with an afflicted member of the family versus the general public (Ascherio & Munger, 2007). In addition, MS is more prevalent in certain ethnic groups than others due to the genetic expression variance (Ascherio & Munger, 2007). More specifically there are a few genes which when mutated are more likely to be linked with MS, they are found in the human leukocyte antigen (HLA) system (Ascherio & Munger, 2007). Mutations in this system have been shown to be susceptible to the progression of various autoimmune diseases including type-1 diabetes (Ascherio & Munger, 2007). In general research show that changes in the HLA system are responsible for between 20 to 60 percent of the genetic predisposition to MS (Ascherio & Munger, 2007).
<br>
Symptoms
MS symptoms vary from person to person (Multiple Sclerosis Clinical Presentation, 2016).
MS Symptoms include:
- Sensory loss
- Walking difficulty
- Spasticity
- Bladder, bowel, and sexual dysfunction
- Tremors
- Optic neuritis
- Heat intolerance
- Fatigue
- Pain
- Cognitive difficulties
- Constipation
<br>
Diagnosis
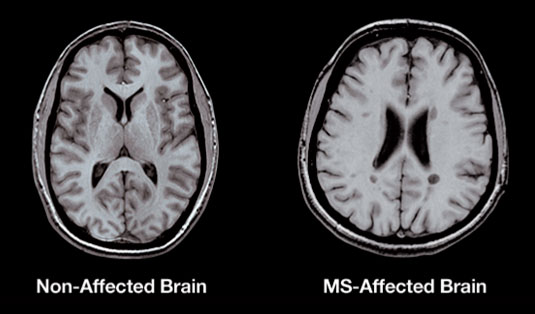
Figure 1: A T1-weighted MRI demonstrating permanent lesions in a MS patient. The dark spots
in the scan are the lesions. (Source: Spinms, 2016)
</style>
<style justify> The diagnosis of Multiple Sclerosis (MS) can be detected through MRI, lumbar puncture and electroencephalography. MS is difficult to diagnose due to the multiple symptoms associated with the disease, which can vary from person to person. Magnetic resonance imaging (MRI) can be used to reveal areas of lesions. However, MRI has disadvantages as it lacks specificity and many conditions have similar conditions of MS and as a result many false positives occur. It has been determined that 90% of MS patients will display an abnormal MRI scan and thus MRI should be the first diagnostic tool to be used. However, 5% of individuals show no sign of lesions in the brain while using MRI (Rolak, 2003).
When there are abnormalities in the cerebrospinal fluid, it can be used to diagnose MS. In the Cerebral spinal fluid (CSF), the white blood cell and spinal fluid proteins are slightly elevated. An elevated Immunoglobin G level in CSF is the most significant in detecting MS. The Immunoglobin G reflects an autoimmune activation and appears as oligoclonal bands on the electrophoresis performed on the CSF. Oligoclonal bands indicate the presence of immunoglobins, which indicate inflammation in the central nervous system. The oligoclonal bands vary from MS patient, but 90% of MS patients present these bands. A limitation to this method is other diseases produce these bands as well and can lead to misdiagnosis. To obtain the CSF it requires undergoing lumbar puncture, which many patients are unsure of doing (Rolak, 2003).
Another method that could be used is evoked potential, which is used to measure conduction rates in the CNS pathway though the recording of electroencephalographic response to sensory stimulation. Slow conduction rates indicate inflammation and demyelination, presenting an MS lesion (Rolak, 2003).
Prognosis and progression
There are four different patterns of MS,
- Clinically Isolated Syndrome (CIS)
- Relapsing and remitting (RRMS)
- Secondary progressive (SPMS)
- Primary progressive (PPMS)
Clinically Isolated Syndrome refers to a first episode where there is inflammatory demyelination in the CNS. It is not yet considered MS, but could become MS if further activity occurs. In the relapse and remitting stage this indicates good health followed by an immediate change in symptoms. Secondary progressive MS occurs after the relapse and remitting stage. At this point there are more symptoms that are progressively getting worse. Primary progressive MS is the steady development of symptoms that will eventually become worse as the diseases progresses. RRMS, SPMS, and PPMS can be active or not active depending on if there is evidence of relapse or disease activity present (Hedley, 2012). </style>
<br>
Pathophysiology
<style justify> Three characteristics that may be present in Multiple Sclerosis are lesion/plaque formation, inflammation and destruction of myelin sheaths. The exact mechanism of T cells becoming autoreactive is widely unknown, however they have been able to propose molecular mimicry as a possible reason for the autoimmune process involved in MS (Wu and Alvarez, 2011). Molecular mimicry concept proposes that the Myelin Basic Protein (MBP) sequence from 85-99 resembles some pathogens or viruses antigens and could be involved in initiating autoimmunity. Some of these viruses can include the herpes virus family (EBV, herpes simplex, and cytomegalovirus), influenza viruses, and papillomaviruses (Wucherpfennig and Strominger, 1995). After the penetration of the Blood-brain barrier, the inflammatory process causes the demyelination of neurons and therefore leading to the formation of lesions. The disease process also consists of loss of myelin and disappearance of oligodendrocytes, which is known for the synthesis of myelin protein (Wu and Alvarez, 2011). </style>
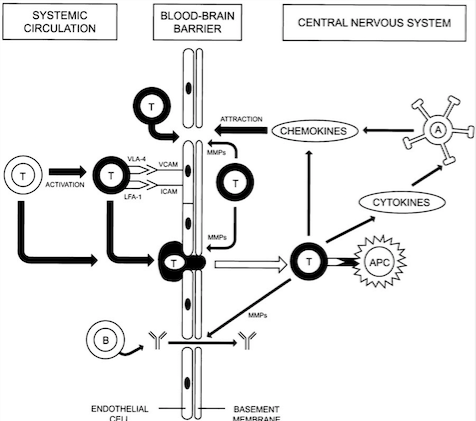
<style justify> Blood-brain barrier Penetration: Initially, for the T cells to cause lesion formation, they need to penetrate the Blood-brain barrier. The Blood-brain barrier consists of endothelial cells, tight junctions and basement membrane (Löscher and Potschka, 2005). The immune system cells travels through blood vessels which also contain endothelial cells. The Blood-brain barrier has selective permeability and prevents the immune system cells from entering the brain (Wingerchuk et al., 2001). However, when triggered by a virus such as Epstein Barr Virus (EBV), the Blood-brain barrier can be penetrated by T cells that can be autoreactive or be programmed to attack myelin protein present on the axons of the neurons (Wu and Alvarez, 2011).
Inflammation in the area due to a virus or foreign substances causes more T cells and macrophages to be recruited into the Blood-brain barrier due to the help of increased expression of adhesion molecules (Wingerchuk et al., 2001). Then, activated and non-activated T cells can secrete Matrix metalloproteinases (MMPs) which cause the degradation of the extracellular matrix, therefore weakening the Blood-brain barrier and allowing for other leukocytes and macrophages to enter (Wingerchuk et al., 2001). Inside the Central Nervous System, T cells can be activated by Antigen Presenting Cells and antibodies, therefore releasing an increased amount of chemokines and cytokines, which can recruit a much larger inflammatory response and lead to initiation of lesion formation (Wingerchuk et al., 2001).[X]. </style>
Figure X: Illustrates the mechanism used by T cells to penetrate the Blood-brain
Barrier (Source: Wingerchuk et al., 2001).
</style>
<style justify> Lesions: In Multiple Sclerosis, lesions will be formed in the white matter of the brain due to demyelination of neurons in the Central Nervous System. Demyelination or lesion formation can occur in any area, but most often occurs in the periventricular regions, optic nerves, brainstem, cerebellum and spinal cord (Wingerchuk et al., 2001). Demyelination usually occurs due to an autoimmune response by T cells towards myelin protein and oligodendrocytes, which are responsible for synthesizing myelin protein (Wu and Alvarez, 2011). [X].
Different type of lesions: (Wu and Alvarez, 2011) There are four different types of patterns of lesions and each one of them varies in composition. (Most common forms are III and IV).
- Pattern I: Contains T cells and macrophages
- Pattern II: Contains T cell and macrophages, as well as immunoglobulin and myelin degradation products
- Pattern III: Loss of Oligodendrocytes and myelin glycoprotein
- Pattern IV: Oligodendrocytes dystrophy and absence of remyelination
[X]. </style>
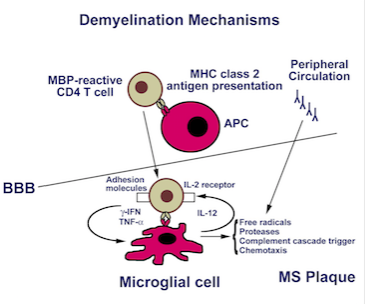
Figure X: Illustrates the inflammatory response towards myelin
protein, thus causing formation of lesions (Source: Luzzio, (n.d.)). </style>
<style justify> Lesion Formation Mechanism: (Brosnan) One of the proposed mechanisms of lesion formation was further examined by Brosnan and Raine (1996). They proposed that CD4 T cells were activated outside the Blood-brain barrier by Antigen presenting cells to either myelin protein or oligodendrocytes. The CD4 T cells would enter the Blood-brain barrier and the activated CD4 T cells would recognize antigens presented by microglial cells, which are the macrophages in the Blood-brain barrier or B cells antibodies (Brosnan and Raine, 1996). Once the MHC class 2 receptor recognition and costimulation occur, the CD4 T cells can now release cytokines such as TNF-alpha, gamma-IFN and IL-17. Then the activated microglial cell releases free radicals, nitric oxide, proteases which can cause destruction of tissue in Central Nervous System and recruit more of an inflammation response. This can ultimately cause irreversible tissue and axonal damage and therefore leading to the formation of lesions (Brosnan and Raine, 1996).[X] [Figure X]. </style>
Figure X: Demonstrates the location and as well as the immune cells involved
in the production of IL-17 (Source: Tzartos et al., 2008). </style>
<style justify> Inflammation: The attacks by the T-cells on myelin cause inflammatory processes, triggering other immune cells, cytokines and antibodies. The Blood-brain barrier starts to swell as well as macrophages are activated along with cytokines and other destructive proteins (Wu and Alvarez, 2011). [X] </style>
Effect of Demyelination: After demyelination, the nerve tissue is damaged and the axons are not able to conduct action potentials effectively due to loss of myelin, which ultimately acts as an insulator. This prevents the body to communicate with the Central Nervous System effectively, therefore causing numbness in certain areas of the body (Smith and McDonald, 1999). [X]
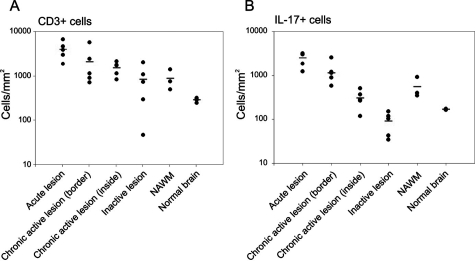
Figure X: Illustrates the expression
of CD3 T cells and as well as the
activity of the CD3 T cells based on
IL-17 production in patients with
different stages of MS.
(Source: Tzartos et al., 2008) </style>
<style justify> Evidence Supporting Immune-mediated Pathophysiology: In an experiment conducted by Tzartos et al. (2008), they wanted to explore specifically which immune system factors and cells were involved in demyelination as well as the role of Interleukin-17 in demyelination (Tzartos et al., 2008). Initially, they wanted to determine whether T cells, astrocytes, microglia/macrophages, oligodendrocytes were able to produce IL-17, since there were earlier reports that IL-17 is present in higher concentrations in MS tissues. They used in situ hybridization and immunofluorescent-labelled IL-17 mRNA (Tzartos et al., 2008). In addition, they also labelled the interested cells and used an overlap imaging technique to show where IL-17 was present and therefore indicating its production . Astrocytes, T cells, oligodendrocytes all overlapped with IL-17 expression while microglia/macrophages did not (Tzartos et al., 2008). ( Fig X- T cells showed the largest expression, while astrocytes and oligodendrocytes showed small amount). In another experiment, they then wanted to see whether there was an increase of activity of CD3 T cell involved ( Th17 cells) in lesions/plaques and compare this to normal nerve tissue. They also looked at IL-17 to assess the activity of the activated Th17 cells (Tzartos et al., 2008). Using tissue samples from the perivascular areas of acute lesions, active borders of chronic active lesions, inactive lesions, inactive areas of chronic active lesions and as well as NAWM in MS patients(normal appearing white matter), they observed that there was increased amount of IL-17 cytokine and CD3 T cells in MS patient tissues samples compared to the non MS brain (control variable) . This indicated that IL-17 is largely involved in the inflammatory response in MS (Tzartos et al., 2008). In addition, they looked at alternative method to quantify the presence of IL-17 in MS patient brain sample. They compared the densities and were able to conclude the similar results as previously reported. Therefore, demonstrating that IL-17 and CD3 T cells were involved in carrying out an inflammatory response leading to demyelination of neurons (Tzartos et al., 2008). Fig [X] </style>
Figure X: Illustrates the observed expression as a density for both CD3 T cells and
IL-17 based on the different stages of MS (Source: Tzartos et al., 2008). </style>
<style justify> Non-immunological Roles of Demyelination: The immune-mediated destruction of myelin protein on neurons is not the only to cause demyelination. Other known non-immunological causes of demyelination can be soluble substances such as perforin, calpain (Calcium activated proteases involved in myelin protein degradation) and also reactive oxygen and nitrogen species such as nitric oxide (Brosnan and Raine, 1996).</style>
<br> <br> <br> <br> <br> <br> <br> <br> <br> <br> <br> <br> <br> <br>
Treatment and Management
<style justify>
Currently, there is no cure for multiple sclerosis as there are still many unclear aspects to the disease. (Hedley, 2012) There are several treatments available to aid with prolonging the remission period, to manage relapse, and to manage symptoms of the disease. Different treatments are recommended for different patterns of MS. For RRMS, SPMS, disease modifying drugs (DMDs) may be prescribed, whereas with PPMS, symptomatic treatment is the main approach as there has yet to be a proven disease modifying treatment. (Hedley, 2012) There are also complementary therapies available for MS.
<br>
Maintaining Remission
There are treatments available to modify the disease course by helping to maintain remission and delay relapse in MS. For RRMS, SPMS, disease modifying drugs (DMDs) may be prescribed. There are many DMDs available for MS. Interferon beta and glatiramer acetate are the current front-line therapies for maintaining remission. These make up the ABC-R therapy of MS, which consists of Avonex (interferon b-1a), Betaseron (interferon b-1b), Copaxone (glatiramer acetate), and Rebif (interferon b-1a). (Hillman, 2014)
Interferon Beta
Interferon beta is in the family of cytokines, which possess antiviral and immunoregulatory activities. The mechanisms of interferon beta in MS, however, are not clearly understood. (Hedley, 2012) There are two types of interferon beta (interferon beta-1a and interferon beta-1b) that have no difference in effectiveness. They are only different in the way they are manufactured. Interferon beta use in MS patients reduces the number and severity of relapses, and improves MRI measures. (Hillman, 2014) Studies show that MS patients using interferon beta therapy showed 75% fewer brain lesions on a brain MRI compared with a placebo. (Hedley, 2012) The effect of the treatment on long-term progression is not clear. There are some serious side effects of interferon beta. These include flu-like symptoms such as myalgia, fever, chills, asthenia, headache, and nausea, as well as psychological symptoms such as depression. Interferon beta may also lead to the development of neutralizing antibodies that may lead to a decrease in the effectiveness of therapy. (Hillman, 2014)
Glatiramer Acetate
Glatiramer acetate is thought to alter the immune processes believed to be responsible for the pathogenesis of MS, however its mechanism is not fully known. (Hedley, 2012) Studies have shown that there is delay of progression from CIS to “clinically definite MS” in MS patients for up to three years with use of glatiramer acetate. (Hedley, 2012) This treatment reduces the number and severity of relapses, and the formation of new lesions on a brain MRI, however its effects on long-term progression are not clear. (Hedley, 2012) Adverse effects of glatiramer acetate minor and mainly consist of injection site reactions, seen in 70% of patients. (Hedley, 2012) Other less common side effects include lipoatrophy, flushing, shortness of breath, chest tightness, and palpitations. (Hillman, 2014)
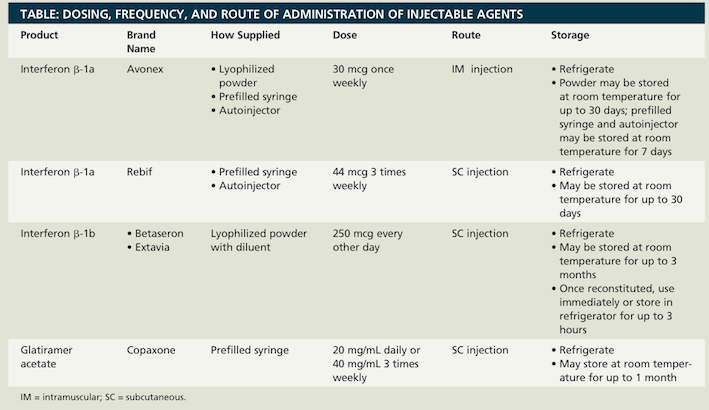
Deciding on which treatment to use (interferon beta or glatiramer acetate) depends on patient preference in type and frequency of injection. (See Figure X)
</style>
<style float-right>
Figure X: The dosing, frequency, and route of administration for the ACB-R therapies. (Source: Hillman & Khorassani, 2014)
</style>
<style justify>
There are several other treatments available aside from the front-line ABC-R therapies.
Natalizumab
Natalizumab is a monoclonal antibody that is currently the best treatment for preventing relapses. (Hedley, 2012) 67% of patients using Natalizumab are relapse free (compared to 41% of patients with a placebo) after two years of treatment. (Hedley, 2012) This treatment is recommended for patients with rapidly evolving severe RRMS. There are however, several side effects including infections, urticaria, and headaches to name a few. (Hedley, 2012) One side effect that could possibly escalate to something serious is an increased risk of progressive multifocal leukoencephalopathy (PML). With PML, there is a progressive inflammation of white matter in the brain. Due to the morality of up to 50% with PML, Natalizumab is not a first-line therapy. (Hedley, 2012)
Mitoxantrone
Mitoxantrone is not used as often since the development of natalizumab. It is a DNA-reactive agent of which the mechanism of action is not yet known, but is approved in the US to treat SPMS and RRMS. (Hedley, 2012) It is cytotoxic, thus has serious side effects such as life threatening reactions and cardiac toxicity. Mitoxantrone has a maximum lifetime dose and thus is not used long-term. (Hedley, 2012)
Azathioprine
Azathioprine is an immunosuppressant that is used to try to prevent relapse and to slow disease progression. It is not commonly used as side effects include gastrointestinal disturbances, bone marrow suppression, and hepatic toxicity. (Hedley, 2012)
Fingolimod
Fingolimod is a sphingosine-1-phosphate receptor modulator that retains lymphocytes in lymph nodes. This prevents lymphocytes from reaching the CNS and causing damage. (Hedley, 2012) In RRMS patients where interferon beta is unsuccessful, fingolimod is used. It is administered orally (one capsule daily). (Hedley, 2012) The development of oral agents are exciting as it is a easier method of administration than injections.
Maintaining Relapse
There are also treatments to manage relapse MS. Relapses in MS are caused by inflammation in the CNS, damaging the myelin of nerve fibers. Due to the varying lengths, severity, and nature of relapses, treatment is not always needed. (Hedley, 2012) Treatment is recommended for severe relapses when distress is experienced or when there is increased limitation of activities. Corticosteroids are the treatment of choice when there is demyelination. Methylprednisolone is a synthetic glucocorticoid that is a strong anti-inflammatory. (Hedley, 2012) It is unclear what it does exactly with MS, but it is thought to aid by immunosuppression or to reduce the accumulation of fluid around nerve damage. Studies have shown that steroids are effective in speeding up recovery from relapse, however there are no benefits to the long-term progression of disease. (Hedley, 2012) There are short-term and long-term treatments available, however long-term treatment should be avoided due to the side effects. Side effects of long-term treatment include weight gain, acne, cataracts, osteoporosis, deterioration of the head of the thigh bone, and diabetes. The side effects of short-term treatment are minor. (Hillman, 2014)
Maintaining Symptoms
Treatment for complications that are associated with MS are also available. Common symptoms of MS are fatigue, bladder and bowel problems, weakness, spasticity, and swallowing difficulties.
Fatigue
Up to 95% of MS patients experience fatigue, and more than half describe it as one of the most troubling symptoms of MS. (Amato & Portaccio, 2012) The pathophysiology of fatigue in MS is not well understood. There are both pharmacological and non-pharmacological therapeutic approaches to MS. The most studied pharmaceuticals are amantadine, modafinil, and aminopyridines. There are several non-pharmacological interventions. One is neuro-rehabilitation, which improves compensation, adaptation and reconditioning. Another is exercise, which has very promising results such as reduced fatigue, improve in mood and quality of life. (Amato & Portaccio, 2012) Finally there is behavioural therapy, which strives to educate patients and caregivers about how to make small behavioural changes to reduce fatigue. This may include education on planning rest, relaxation techniques, adapting daily living activities, making everyday tasks more energy efficient, and controlling external temperature. (Amato & Portaccio, 2012)
</style>
<style float-right>
Figure X: Body weight assisted treadmill training. There is physical assistance for each
leg due to impaired walking ability. (Source: http://agelessphysio.com)
</style>
<style justify>
Bladder
Another symptom of MS is an overactive bladder. To manage an overactive bladder, MS patients can reduce fluid intake and caffeine to reduce symptoms of urgency and frequency. However, a daily intake of 1-2 litres of water is recommended. (Fowler et al., 2009) Pharmacological interventions such as antimuscarinic medication is also available to reduce incontinence, frequency, and urgency in MS. (Fowler et al., 2009) Some physical interventions would include pelvic floor exercises to strengthen the pelvic floor and treat stress incontinence. This is effective in patients whose neural pathways to their pelvic floor muscles are intact. (Fowler et al., 2009) In MS patients with neurogenic bladder dysfunction, clean intermittent self-catheterization is used. (Fowler et al., 2009)
Walking Ability
A common symptom of MS is impaired walking ability. Dalfampridine (Fampyra or Ampyra) can be used to improve walking ability. Dalfampridine is a potassium channel blocker that enhances conduction along demyelinated nerve fibres. (Hillman, 2014) In phase 3 clinical trials, walking speed was increased by about 25% within weeks in MS patients. (Hedley, 2012) There are, however, side effects such as a greater risk of seizures, anxiety, insomnia, dizziness, and tremor. (Hedley, 2012) In terms of physical therapy, exercise through treadmill training has been shown to improve walking endurance and velocity. (Amato & Portaccio, 2012) (See Figure X)
Depression
Depression can be a psychological symptom of MS or from interferon beta therapy. For MS patients with severe depression, interferon is avoided. (Hillman, 2014)
Complementary Therapies
Finally, there are therapies available that can be used alongside MS treatment that may help with the general sense of wellbeing in MS patients and help them to feel and cope better with the disease and the treatment. Some complementary therapies include reflexology, massage, tai chi, magnetic field therapy, neural therapy, and fish oils. (Hedley, 2012) Also linoleic acid, found in sunflower, corn, soya, and safflower oils, may reduce the progression of MS. (Hedley, 2012)
Current Research
The majority of research being done on MS primarily involves targeting new medications which better combat relapsing-remitting MS, as well as improving symptomatic treatments. However there is current research being done which aims to promote myelin repair, thus acting as a protective agent against MS. A study done by de la Fuente et al. in 2015, looked at vitamin D as an agent to promote remyelination, which is the process which drives specialized cells to fix damaged myelin found in the CNS nerve fibres. This process happen naturally in a healthy individual, however those afflicted with MS experience a decrease in the function over time due to the continuous damage being done to their myelin (de la Fuente et al. 2015). Cells termed oligodendrocyte progenitor cells (OPC) are responsible for creating oligodendrocytes which manufacture the myelin sheath (de la Fuente et al. 2015). Vitamin D is important because it binds to a specific protein, retinoid X receptor-y (RXR-y), which aids in swiftly maturing OPC into oligodendrocytes. Thus increasing the rate at which the myelin repairing oligodendrocytes, this would be greatly beneficial in battling MS. The study looked at a MS like disease in rats, more specifically focusing on the vitamin D receptors. They found that the RXR-y protein interacts with the vitamin D receptor, which stays active during the remyelination stage. This led to improved remyelination. Furthermore when the vitamin D receptors were prevented from binding and functioning correctly, the OPCs did not develop properly into oligodendrocytes, therefore leading to malfunctioning remyelination in the rats. This type of study investigating the remyelination enhancement possibility from vitamin D is the trend in current research.
</style>
<br>
References
Amato, M. P. & Portaccio, E. (2012). Management options in multiple sclerosis-associated fatigue. Expert Opinion on Pharmacotherapy, 13(2), 207-216
Brosnan, C. F., & Raine, C. S. (1996). Mechanisms of immune injury in multiple sclerosis. Brain Pathology, 6(3), 243-257.
de la Fuente AG et al. Vitamin D receptor-retinoid X receptor heterodimer signaling regulates oligodendrocyte progenitor cell differentiation. J Cell Biol. 2015; 211(5):975-85. Multiple Sclerosis Clinical Presentation. (2016). Retrieved September 18, 2016, from http://emedicine.medscape.com/article/1146199-clinical
Fowler, C. J., Panicker, J. N., Drake, N., Harris, C., Harrison, S. C. W., Kirby, M., Lucas, M., Macleod, N., Mangnall, J., North, A., et al. (2009). A UK consensus on the management of the bladder in multiple sclerosis. Postgraduate Medical Journal. 85, 552-559.
Hedley, L. (2012). Multiple sclerosis treatment options. The Pharmaceutical Journal. 288, 247-250.
Hillman, A. & Khorassani, F. (2014). Multiple sclerosis management. Pharmacy Times. Retrieved from http://www.pharmacytimes.com/publications/health-system-edition/2014/march2014/multiple-sclerosis-management
Löscher, W., & Potschka, H. (2005). Blood-brain barrier active efflux transporters: ATP-binding cassette gene family. NeuroRx, 2(1), 86-98.
Multiple Sclerosis Clinical Presentation. (2016). Retrieved September 18, 2016, from http://emedicine.medscape.com/article/1146199-clinical
Multiple Sclerosis Society of Canada. (2016). Retrieved September 18, 2016, from https://mssociety.ca/about-ms/what-is-ms
Rolak, L. A. (2003). Multiple Sclerosis: It's Not The Disease You Thought It Was.Clinical Medicine & Research, 1(1), 57-60. doi:10.3121/cmr.1.1.57
Smith, K. J., & McDonald, W. I. (1999). The pathophysiology of multiple sclerosis⋮ the mechanisms underlying the production of symptoms and the natural history of the disease. Philosophical Transactions of the Royal Society of London B: Biological Sciences, 354(1390), 1649-1673.
Tzartos, J. S., Friese, M. A., Craner, M. J., Palace, J., Newcombe, J., Esiri, M. M., & Fugger, L. (2008). Interleukin-17 Production in Central Nervous System-Infiltrating T Cells and Glial Cells Is Associated with Active Disease in Multiple Sclerosis. The American Journal of Pathology, 172(1), 146–155.
Wingerchuk, D. M., Lucchinetti, C. F., & Noseworthy, J. H. (2001). Multiple sclerosis: current pathophysiological concepts. Laboratory investigation, 81(3), 263-281.
Wu, G. F., & Alvarez, E. (2011). The immuno-pathophysiology of multiple sclerosis. Neurologic Clinics, 29(2), 257–278.
Wucherpfennig, K. W., & Strominger, J. L. (1995). Molecular mimicry in T cell-mediated autoimmunity: viral peptides activate human T cell clones specific for myelin basic protein. Cell, 80(5), 695-705.