Biochemistry of Thermal Injury
Pathophysiology
The body responds to a burn injury in two ways: local response and systemic response. Locally, there is tissue damage and systemically, organ systems are affected as a result of the burn (DeSanti, 2005).
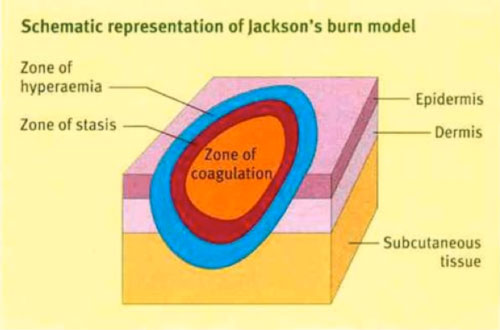
Local Response: Three Zones of a Burn
Figure: 3 Zones of a Burn
There are 3 zones of a burn, as described by Jackson’s Thermal Wound Theory.
- Zone of Coagulation: This is the most central location of the burn, where the damage is maximum and irreversible. This occurs due to coagulation of constituent proteins.
- Zone of Stasis: In this area there is decreased tissue perfusion (flow of blood). The tissue here can potentially be salvaged if it is not subject to additional damage such as an infection.
- Zone of Hyperemia: This is the peripheral area of the burn where there is an increased flow of blood and decreased cell injury. This area generally recovers unless there is additional damage such as an infection. (Hettiaratchy 2004).
Systemic Responses
Cardiovascular Response
There are 2 stages of cardiovascular response following a burn injury: acute/resuscitative phase, which lasts about 48 hours and a hypermetabolic phase. During the acute phase, there is decreased blood flow to tissues and organs due to the direct effect of heat. In this phase, there is an increase in capillary permeability, which further induces fluid and protein loss. During the hypermetabolic phase, there in an increase in internal temperatures and blood flow to tissues and organs. In this phase, there is formation of an edema as well as increased water permeability. This can lead to cardiac instability, hypotension and decrease in myocardial contractility. It may dispose an individual to myocardial infarction (Cakir 2004) (Hettiaratchy 2004).
Pulmonary Response
Within the first couple hours of a burn injury, lung inflammation and lipid peroxidation occurs, which increases oxygen radicals. This response persists for a minimum of 5 days following the burn. Mortality can occur among burn victims if there are respiratory difficulties from inhaling smoke. Inhalation injury after burn trauma includes bronchial obstruction, airway resistance and altered capillary permeability. In severe burns, adult respiratory distress syndrome can occur (Hiettiaratchy 2004). Renal Response
The renal system of an individual responds by decreasing renal blood flow and glomerular filtration rate after a burn injury. Levels of stress hormones, such as catecholamine, angiotensin, aldosterone and vasopressin increase. These renal responses can result in acute renal failure, which can further result in mortality (Cakir 2004).
Gastrointestinal Response
The renal system of an individual responds by decreasing renal blood flow and glomerular filtration rate after a burn injury. Levels of stress hormones, such as catecholamine, angiotensin, aldosterone and vasopressin increase. These renal responses can result in acute renal failure, which can further result in mortality (Cakir 2004).
Immune Response
Thermal injury results in an immunosuppressed state. Following a burn, the body releases pro-inflammatory factors but there is a depression in the lines of defense. When the skin layers are damages, there can be microbial invasion and growth in the damaged skin. Neutrophil accumulation increases in tissues, phagocytic activity is inhibited, macrophage hyperactivity increases and T-cells cannot function properly. This results in an increase in reactive nitrogen intermediated which cause immune dysfunction. Due to this, there is an increased susceptibility to sepsis, the presence of bacteria and toxins in tissues, and this can result in multiple organ failure. Burn toxins and oxygen radicals are also produced, which further lead to peroxidation. Comprised immune function is a leading cause of morbidity and mortality in burn patients (Cakir, 2004) (Hettiaratchy, 2004).
Types of Burns
Thermal Burns
Thermal burns occur due to heat sources coming in contact with the skin and raising the temperature. They can be caused by exposure to hot charring liquids, flames, steam, hot metals etc. This can result in tissue cell death as well as charring.
Electrical Burns
Electrical burns occur through electrocutions, when an electric current travels through the body.
Chemical Burns
Chemical burns occur when the skin or eyes come in contact with chemical products that are corrosive agents. Alkalis, acids, detergents or solvents can cause this type of burn.
Radiation Burns
Radiation burns occur when the skin is exposed to sources of radiation, such as UV from the sun or X-rays, for a long time (John Hopkins Medicine 2007).
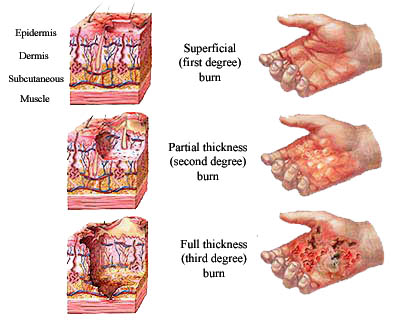
Classifications of Burns
Figure: Burn Classifications
First Degree (Superficial)
First-degree burns directly affect the outer layer of the skin (epidermis). The burn site appears to be dry and red. An example of a first-degree burn is a sunburn.
Second Degree (Partial Thickness)
Second-degree burns affect the epidermis and dermis layers of the skin. The burn site appears to be red, blistered and swollen. An example of a first-degree burn is a burn from scalding hot water.
Third Degree (Full Thickness)
Third-degree burns fully penetrate the epidermis and dermis layers. The burn site appears to be white or charred but there are no sensations of pain since the nerves are destroyed in these areas. An example of a third-degree burn is a flame burn from a fire.
Fourth Degree
Fourth-degree burns occurs when bones, muscles and tendons are burned in addition to the epidermis and dermis layers. They can occur from prolonged exposure to flame or an electrical injury from high voltage. (John Hopkins Medicine 2007).