This is an old revision of the document!
Table of Contents
Obesity
Introduction
 Obesity is a progressive illness which is usually defined by an abnormal and excessive accumulation of body fat that can have a negative impact on one’s health (Mokdad et al., 2003).
Obesity is a progressive illness which is usually defined by an abnormal and excessive accumulation of body fat that can have a negative impact on one’s health (Mokdad et al., 2003).
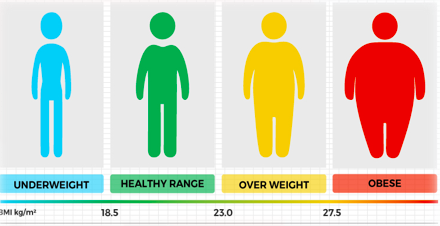
Population health studies estimate the prevalence of obesity by categorizing individuals based on a Body Mass Index (BMI) (Katzmarzyk & Mason, 2006). Generally, individuals with a body mass index greater than 30 kg/m2 are considered to be obese. However, a body mass index alone is not enough to diagnose someone with obesity. A qualified health care professional will make the diagnosis based on additional clinical tests and measures (Katzmarzyk & Mason, 2006).
Studies show that the prevalence of obesity has increased significantly in the last 30 years (“Obesity in Canada,” n.d.). According to the 2014 and 2015 Canadian Community Health Surveys, over 5 million adults have obesity and 30% of adults in Canada have obesity and these individuals may require medical support to manage their condition. Organizations such as Obesity Canada, the American Medical Association and the World Health Organization now consider obesity to be a chronic disease. Furthermore, obesity is the main cause of of type 2 diabetes, high blood pressure, heart disease, stroke, arthritis and cancer. In fact, 1 in 10 premature deaths among Canadian adults from ages 20 to 64 is thought to occur directly due to obesity related complications (“Obesity in Canada,” n.d.).
In 2001, a US study conducted a telephone survey of 195 005 adults aged 18 years or older residing from all states (Mokdad et al., 2003). They found the prevalence of obesity (BMI ≥30) to be 20.9% and had risen dramatically when compared to prevalence rates from the 1990’s. Overall, the study concludes that increases in obesity among US adults continue in both sexes, all ages, all races, all educational levels, and all smoking levels (Mokdad et al., 2003).
Aside from physiological impairments, obesity can also impact one’s overall psychological, social and economic well-being due to the social stigma associated with the disease. Obesity stigma can cause unequal access to employment, healthcare and education. This is because some individuals may view obese people as lazy, careless and apathetic.
Studies predict that the direct healthcare cost of obesity based on hospitalization and medication costs is approximately $7 billion (“Obesity in Canada,” n.d.). By 2021, the costs are expected to rise to $9 billion and continue to rise as the prevalence of obesity is expected to increase during the next two decades (“Obesity in Canada,” n.d.).
Ultimately, public, private and non-governmental initiatives covering the rises of obesity and treatment options are needed to control this global epidemic.
Diagnosis
Obesity diagnosis can be based on the individual’s physical exam, medical history, their body mass index, and their waist circumference (National Heart, Lung, and Blood Institute, 2019).
Body Mass Index
Dependent on if you are a child or adult, doctors use calculations to measure the BMI of the individual to diagnose obesity. The body mass index is a calculation that uses an individual’s weight and height. The formula is BMI = weight (kg) / height (m^2). The body mass index is used to determine whether the individual is underweight, healthy weight, overweight, or obese. Looking at the chart provided, children are considered underweight if their BMI is under the 5th percentile, and adults are considered underweight if their BMI is under 18.5 (National Heart, Lung, and Blood Institute, 2019). Children are considered obese if their BMI is the 95th percentile or above, and adults are considered overweight if their BMI is 30 or above (National Heart, Lung, and Blood Institute, 2019).
Physical and Medical Examination
Doctors tend to ask the individual about their family history and the individual’s physical and eating habits, which helps them to determine whether other conditions are causing obesity or if obesity is causing any other complications (National Heart, Lung, and Blood Institute, 2019). When the doctors are doing a physical exam, the doctor’s look at the abdomen examining the unhealthy fat it contains, which allows them to measure your waist circumference (National Heart, Lung, and Blood Institute, 2019).
Causes
One of the causes of obesity is an imbalance in energy (National Heart, Lung, and Blood Institute, 2019). This energy is calculated in calories and means that the energy going out does not equal the energy coming in. Energy going out is when the body uses the calories for breathing or physical activities. Energy going in is when the body gains the calories from drinks and food. When the body takes in more calories then it uses, that is when obesity develops (National Heart, Lung, and Blood Institute, 2019). The imbalance in energy leads to the body storing fat.
There are many medicines in the market that can lead to an individual gaining weight and becoming obese. Some of these medicines include antipsychotics and antidepressants (National Heart, Lung, and Blood Institute, 2019).
Hormones produced by the endocrine system help maintain a balance in energy in the body. When there is a disorder or tumor in the endocrine system, it can lead to the individual becoming obese (National Heart, Lung, and Blood Institute, 2019). An example of this is hypothyroidism (National Heart, Lung, and Blood Institute, 2019). Individuals that have this condition have a low amount of thyroid hormones. This is linked with reduced metabolism, leading to the individual gaining weight.
Risk
Obesity has many risk factors that can be changed and many risk factors that cannot be changed. The factors that can be changed are environments and unhealthy lifestyle habits (National Heart, Lung, and Blood Institute, 2019). The factors that cannot be changed are age, sex, genetics, family history, and ethnicity (National Heart, Lung, and Blood Institute, 2019). Changing your unhealthy lifestyle habit into a healthy lifestyle can decrease the risk of becoming obese.
Evolutionary Basis of Obesity
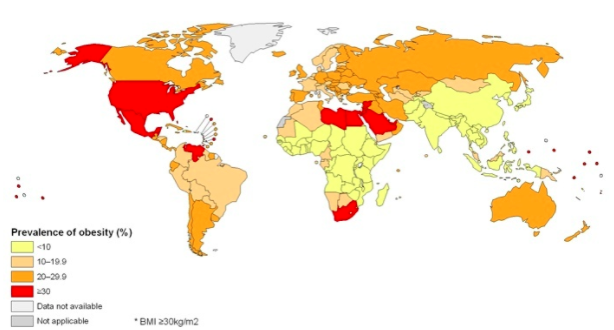
Figure 3: This map displays a country-by-country look at adult obesity prevalence in 2008. https://www.hsph.harvard.edu/obesity-prevention-source/map-of-global-obesity-trends/
Obesity and Gender
Pathophysiology
In the past decade, a bulk of research regarding obesity has looked into its regulation since it is tied with molecular regulation of appetite, ultimately affecting energy homeostasis. With that said, during nutrient deprived states, like starvation, a plethora of stored fat is necessary in order for the individual’s survival. On the other hand, during prolonged abundance of food in the body, there is excessive storage of fats that result in obesity, due to the body’s extremely efficiency fat storage system (Spiegelman & Flier, 2001). The excessive storage of fat that creates obesity will stimulate an enhanced sympathetic state, which will eventually lead to release of excessive fatty acids from enhanced lipolysis. Subsequently, this excessive release of fatty acids are free in the body and can stimulate lipotoxicity because there is oxidative stress to the endoplasmic reticulum (ER) and mitochondria of cells that is created by the lipids and their metabolites. Not only does this phenomenon affect adipose tissues, but also non-adipose tissues as well, which is why obesity extends its pathophysiology to many organs like the kidneys, liver and pancreas as well as in metabolic syndrome (Evans, Barish, & Wang, 2004). In addition, fatty free acids that are secreted from excessively stored triglyceride also aid in the inhibition of lipogenesis which prevents proper clearance of serum triglyceride levels. As a result, the improper clearance of triglyceride contributes to hypertriglyceridemia which means there are a high levels of triglycerides on the blood serum. One consequence of hypertriglyceridemia is the release of fatty acids by endothelial lipoprotein lipase within elevated beta lipoproteins. With that said, there is insulin-receptor dysfunction due to this elevation and this dysfunctional state creates hyperglycemia and increased glucose production in the liver. Furthermore, one other effect from the lipotoxicity caused by excessive fatty acids is a decrease in the secretion of insulin from the pancreas, resulting in beta-cell exhaustion (Redinger, 2007).
Linked Diseases
diabetes–add from word doc
cancer –add from word doc
cardiac problems – add from word doc
Treatments
Conclusion
Obesity is a problem that is impacting many individuals around the world specifically in western countries. This disease can be inherited by environmental or genetic factors. With the consumption of many fats, and high caloric meals the individual can develop obesity. It is critical that the individual burns more calories than they consume. Although, this may not always be the reason but, research has shown that if a person has low to none exercise levels, he or she has a high possibility to develop obesity. Medicines such as insulin and thiazolidinediones (TZDs) can also result in excessive weight gain (OAC, n.d.). Using the body mass index, we can determine whether the person is obese or not. If the child is 95th percentile or over they are considered to be obese and if the adult is 30 or above he/she is obese. To prevent obesity from happening it is critical that to maintain a healthy lifestyle and ask doctors about what medication can result in weight gain.
References
Evans, R. M., Barish, G. D., & Wang, Y.-X. (2004). PPARs and the complex journey to obesity. Nature Medicine, 10(4), 355–361. https://doi.org/10.1038/nm1025
1. National Heart, Lung, and Blood Institute. (2019). Overweight and Obesity. [online] Available at: https://www.nhlbi.nih.gov/health-topics/overweight-and-obesity [Accessed 31 Mar. 2019].
2. Mokdad, A. H., Ford, E. S., Bowman, B. A., Dietz, W. H., Vinicor, F., Bales, V. S., & Marks, J. S. (2003). Prevalence of Obesity, Diabetes, and Obesity-Related Health Risk Factors, 2001. JAMA, 289(1), 76–79. https://doi.org/10.1001/jama.289.1.76
3. Katzmarzyk, P. T., & Mason, C. (2006). Prevalence of class I, II and III obesity in Canada. CMAJ : Canadian Medical Association Journal = Journal de l’Association Medicale Canadienne, 174(2), 156–7. https://doi.org/10.1503/cmaj.050806
4. Obesity in Canada - Obesity Canada. (n.d.). Retrieved April 1, 2019, from https://obesitycanada.ca/obesity-in-canada/
Redinger, R. N. (2007). The Pathophysiology of Obesity and Its Clinical Manifestations. Gastroenterology & Hepatology, 3(11), 856–863. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3104148/
Spiegelman, B. M., & Flier, J. S. (2001). Obesity and the regulation of energy balance. Cell, 104(4), 531–543.