Introduction:
Crohn disease is an idiopathic, chronic inflammatory process of the gastrointestinal (GI) tract which affects any parts of the tract ranging from the mouth to the anus. It is believed to be the result of an imbalance between pro-inflammatory and anti-inflammatory mediators. Some factors which encourages this imbalance are genetic susceptibility and environmental triggers. Hence, there is no real single factor that induces this intestinal inflammation.
Signs and symptoms include abdominal pain, diarrhea, fever, and weight loss. Usually, these symptoms induce complications by intestinal fistulization and obstruction. Additionally, individuals diagnosed with this risk are at a greater risk of developing bowel cancer.
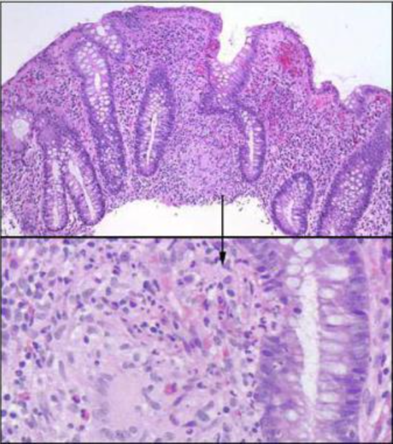
Figure 1: Inflammation of the Gastrointestinal (GI) Tract
Epidemiology:
According to a National Survey analysis that was done on a geographically diverse health insurance claims database, it estimated that the prevalence of Crohns disease among US children and adults between 2003-2004 to be 201 cases per 100,000 persons among adults and 43 per 100,000 among children.
Urban areas are estimated to have a higher prevalence of IBD than rural areas do. Moreover, upper socioeconomic classes are predicted to have a higher prevalence than lower socioeconomic classes due to the difference in the access to health care between the two groups.
In general, the frequency of this disease is similar in males and females, with some studies that shows a very slight female predominance. The rate of Crohn disease is deemed to be 1.1 – 1.8 times higher in women than in men. Moreover, Crohn disease is reported to be more common in white patients than black patients, and very rare in Asian and Hispanic individuals. On average, approximately 20% of all Crohn disease patients are of black descent.
Pathophysiology:
The pathophysiology of Crohn’s disease stems from a chronic inflammation from T-cell activation leading to tissue injury in the gastrointestinal tract. After the antigen activates an immune response, type 1 T-helper (Th1) cells predominate and stimulate an inflammatory response with other Th1 cytokines. Th1 cytokines include interleukin (IL)-12 and TNF-alpha that stimulate this inflammatory response. Inflammatory cells recruited by these cytokines release metabolites, proteases, and free radicals that all result in direct injury to the intestine.
According to a study conducted in 2012, researchers suggest that genetic factors for Crohns Disease leads to an abnormal observation in epithelial barrier integrity, deficits in autophagy, deficiencies in innate pattern recognition receptors, and problems with lymphocyte differentiation (Ghazi, 2016).
On a microscopic level, the initial lesion starts from an ulceration of the superficial mucosa. The inflammatory cells such as granulomas then invade the deep mucosal layers and start extending through all layers of the intestinal walls and into the regional lymph nodes. Although granuloma formation is the primary pathophysiologic factor of Crohn disease, its absence does not exclude the diagnosis.
Figure 2: Invasion of granulosa cells inducing inflammation in GI tract
References:
1 Kornbluth A, Sachar DB, Salomon P. Crohn's disease. Feldman M, Scharschmidt BF, Sleisenger MH, eds. Sleisenger & Fordtran's Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, and Management. 6th ed. Philadelphia, Pa: WB Saunders Co; 1998. Vol 2: 1708-34.
2 Gahzi, Leyla (2016) Pathophysiology of Crohn Disease. Retrieved from: http://emedicine.medscape.com/article/172940-overview#a3