Table of Contents
INTRODUCTION
Marijuana comes from the hemp plant known as Cannabis Sativa (Deem, 2013). It is made up of a concoction of the dried, shredded leaves and flowers from this particular plant (Deem, 2013). Cannabis Sativa plants were initially native to Central and Southern Asia (Deem, 2013). However, today majority of its best-known varieties are grown in Colombia, Mexico, Brazil, and Africa (Deem, 2013). The dominant psychoactive chemical in marijuana, which is responsible for majority of the intoxicating, mind-altering effects that people experience, is delta-9-tetrahydrocannabinol (THC), seen in figure 1 (Deem, 2013). This chemical is found in its most abundant concentrations in resin, which is the byproduct of smoking marijuana. Resin can be smoked as well, however, it is considered to be the unhealthiest aspect of smoking marijuana due to its high concentrations of tar and carbon (Deem, 2013). Additionally, the plant contains over 500 other chemicals, including compounds chemically similar to THC, referred to as cannabinoids (Deem, 2013).
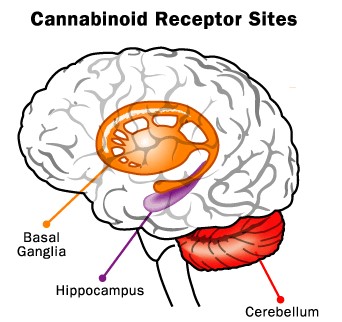
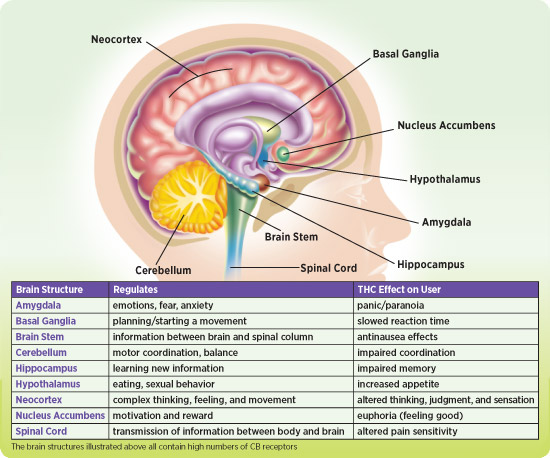
When marijuana is smoked, THC, along with the other chemicals contained within marijuana, pass from the lungs and enter the bloodstream. Once in the bloodstream these chemicals are rapidly carried throughout the body to the brain. The parts of the brain most affected by THC are the hippocampus and cerebellum, as these contain high levels of cannabinoid 1 receptors (which is what THC binds to) (Bonsor & Gerbis, 2001). Once these chemicals reach the brain the effects of the drug are felt. People’s experiences vary from a sense of relaxation, laughter, and increased appetite, to anxiety, fear, or panic. But the latter effects are most common when an individual is inexperienced with the drug or intakes a high amount (Bonsor & Gerbis, 2001). Detectable amounts of THC can remain in the body for days after use, however, noticeable effects from inhaled marijuana generally last between one to three hours (Bonsor & Gerbis, 2001). Once these effects ware off a person will generally return to their typical sober state. The reason why marijuana is considered dangerous is because the ingested THC binds to cannabinoid receptors found in the brain which leads to neural changes, affecting diverse cognitive processes. However, there is currently a lot of debate around how much of these changes are permanent (Bonsor & Gerbis, 2001).
—-
CANNABIS CONSUMPTION
Marijuana can be consumed in various ways ranging from liquid tinctures to dermal patches and oral sprays. Firstly, liquid tinctures are extracts taken from the marijuana plant that are taken orally; as well as oral sprays which could also be administered orally (Cohen & Rudick, 2007). Dermal patches are effective due to the lipophilic property of marijuana, which allows it to be readily dissolved in a fat-soluble substance and penetrate the cell membrane (Rosenthal & Newhart, 2002). The most common way of consuming marijuana is through smoking, vaporizing and eating edibles. Marijuana is often consumed by packing the dried buds into rolling paper, cigars, pipes, or bongs. Also, many prefer to eat marijuana edibles such as, weed brownies and cookies. Other less common methods of consumption include, capsules and lozenges (Rosenthal & Newhart, 2002).
CANNABIS USAGE
MEDICINAL
Marijuana has three prominent usages, medicinal, spiritual and recreational. It is often quite difficult for scientists to study potential medicinal marijuana uses since it is difficult to obtain permission for human medical trials (Richard & Paul, nd). Furthermore, marijuana is currently classified as a schedule 2 substance by the federal government, making it even tougher to obtain permission (Hoffmann & Weber, 2010). In addition, far more studies regarding the potential harmful effects of marijuana have been conducted and only very minimal (6%) have been conducted studying its potential benefits (Gupta, 2013). Many studies focusing on the medicinal use of marijuana have shown varying results and despite little research on marijuana per se, it is important to note this does not imply that marijuana has no medicinal purposes.
However, few case studies and research has led to promising results for potential medicinal uses of marijuana. Firstly, marijuana can be considered during chemotherapy to alleviate common side effects such as vomiting and nausea (Murnion, 2015). Individuals with HIV/AIDS may also use marijuana for similar reasons along with improving their appetite. Marijuana has also been somewhat effective in treating chronic pain and muscle spasms, including pain from neuropathy that may be caused due to fibromyalgia and rheumatoid arthritis (Murnion, 2015). Marijuana has also shown limited evidence in treating neurological problems such as, multiple sclerosis and epilepsy. In epilepsy specifically, Δ9-tetrahydrocannabinol (THC) and cannabidiol (CBD) have shown to give patients relief from cases of spasticity (Murnion, 2015). In addition, some studies have shown marijuana has significantly improved tics in patients suffering from Tourette syndrome. Marijuana can also act as a supplementary means of treatment in individuals suffering from anorexia, arthritis, glaucoma and migraines (Richard & Paul, nd).
Although minimal research has been conducted on cannabinoids and its use in treatment of cancer, cannabinoids have displayed anti-cancer effects in various laboratory experiments. There is ongoing research being conducted to explore different medicinal properties of marijuana. There has been extensive focus on marijuana’s effect on dementia, diabetes, epilepsy, glaucoma, and Tourette syndrome. Cannabinoids have been hypothesized to relieve some of the symptoms associated with Alzheimer’s Disease and may assist in slowing cell damage in diabetes mellitus type 1 (Caulkins, Kilmer, & Kleiman, 2016) .
SPIRITUAL
Marijuana has had a long history of spiritual use and both historically and presently has been viewed as an entheogenic. To elaborate, marijuana has been used to reach a stage of enlightenment, connection, and nirvana. Despite its rich historical use, many religions have opposing stances on marijuana, but those in support have associated the psychoactive effects that marijuana may produce with an intense spiritual experience (Bello, 2007).
RECREATIONAL
The use of a psychoactive drug to alter one’s mind state, modify emotions, cognitions, and perceptions is often described as recreational usage. Marijuana has been long used as a recreational drug due its psychoactive effects (Bello, 2007). Today, people use marijuana for several activities and occasions, including but not limited to (Osborne & Fogel, 2008) :
- Relaxing and Concentrating
- Making everyday activities more enjoyable
- Eating
- Listening to music
- Socializing
- Watching movies
- Playing sports
- Having Sex
EPIDEMIOLOGY
In 2012, 43% of Canadians reported that they had used marijuana at some time in their lives, and 12% reported using it in the past year (Statistics Canada, 2013). Marijuana use was more common among males than females (Statistics Canada, 2013). People aged 18 to 24 had the highest prevalence of past-year marijuana use, and tended to use it more frequently than did people of other ages (Statistics Canada, 2013).
In Canada, as in many other countries, marijuana is the most commonly used illicit drug (Statistics Canada, 2013).
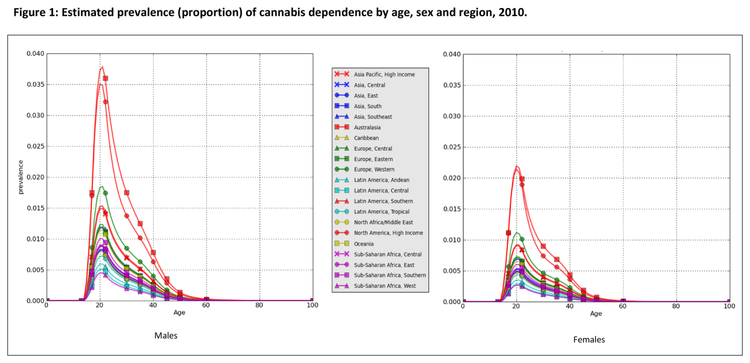
Throughout the world the prevalence was higher in males than females, resulting in an average male:female sex ratio of 1.8 (Degenhard et al, 2013). Prevalence peaks worldwide in the 20-24 years age group at between and then steadily decreasing after that age group thereafter (Degenhard et al, 2013).
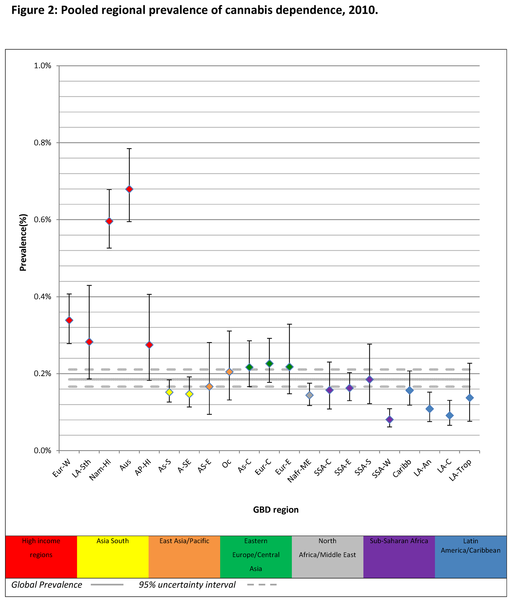
Figure 3: Pooled regional prevalence of cannabis dependence, 2010. Note. Prevalence estimates were standardised by population age and sex; AP-HI: Asia Pacific, High Income, As-C: Asia Central, AS-E: Asia East, AS-S: Asia South, A-SE: Asia Southeast, Aus: Australasia, Caribb: Caribbean, Eur-C: Europe Central, Eur-E: Europe Eastern, Eur-W: Europe Western, LA-An: Latin America, Andean, LA-C: Latin America, Central, LA-Sth: Latin America, Southern, LA-Trop: Latin America, Tropical, Nafr-ME: North Africa/Middle East, Nam-HI: North America, High Income, Oc: Oceania, SSA-C: Sub-Saharan Africa, Central, SSA-E: Sub-Saharan Africa, East, SSA-S: Sub-Saharan Africa Southern, SSA-W: Sub-Saharan Africa, West. (Degenhard et al, 2013)
Prevalence in high income regions was much higher than that in low to middle income regions and the global average (Degenhard et al, 2013). Cannabis dependence in Australasia is about 8 times higher than prevalence in Sub-Saharan Africa, West (Degenhard et al, 2013).
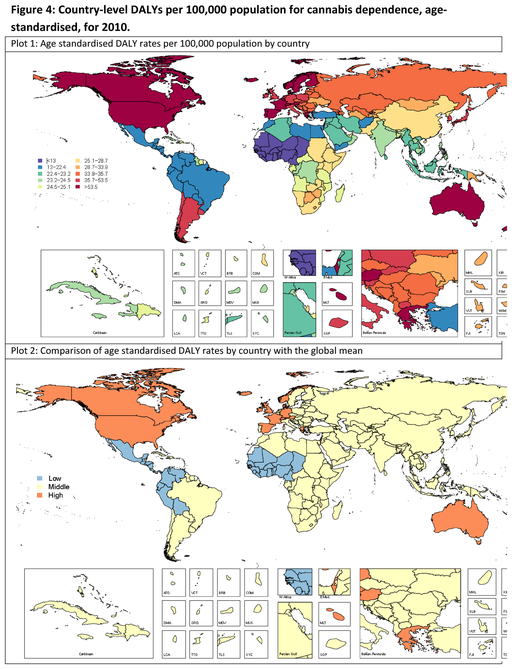
Figure 4: Country-level DALYs per 100,000 population for cannabis dependence, age-standardised, for 2010. Note. Low: shows countries with statistically lower DALY rates than global mean; Middle: Shows countries with DALY rates that are not statistically different to global mean; High: Shows countries with statistically higher DALY rates than global mean. (Degenhard et al, 2013)
Worldwide, DALYs are closely associated with high income countries having more effected years compared to those of low income countries (Degenhard et al, 2013). The statistical DALY rates are comparably higher than the global mean in higher income countries than lower income (Degenhard et al, 2013).
SHORT-TERM EFFECTS
The short-term effects of marijuana on the user can range from increasing relaxation and relieving disease related symptoms to more negative impacts, such as increased heart rate and increased risk of heart disease (Ameri, 1999).
Positive Effects:
Not all users of marijuana do it for the sole purpose of reaching the euphoric sensation of being “high.” Many use cannabis to experience increased relaxation, creativity and pain relief from symptoms associated with various diseases. Recreational users of marijuana enjoy the immediate effect of mild relaxation as well as the increased social enhancement that is involved with using the drug (Lee et al., 2007). Other users smoke cannabis to enhance their creativity, as marijuana is known to reduce inhibition. Whether the drug leads to actual increases in creativity or just an enhanced perception of one’s creativity is still up for debate, as studies show conflicting results (Jones et al., 2009). Yet, many other users of the drug do so in order to decrease chronic pain or the uncomfortable symptoms of different diseases. Cannabis in pharmacotherapy of diseases is still under extensive research, but much of it leans towards treating convulsions, depression, and asthma, among others abnormalities (Martin-Sanchez et al., 2009). Cannabinoids in the brain are associated with improvements in motor control in many patients suffering from Parkinson’s disease, showing its medical usage potential (Lotan et al., 2014). Additionally, marijuana is known as a stimulant to appetite, leading to increases in food consumption (Foltin et al., 1988). It enhances the user’s taste and smell sensitivity to food, as well as increases the number of snacking occasions throughout the day. This is especially beneficial to cancer patients, as it helps minimize nausea that results from chemotherapy (Voth et al., 1997, Martin-Sanchez et al., 2009).
Negative Effects:
Although marijuana may have some positive short-term impacts on the user, it may also bring about a range of harmful effects as well. The extent to which these effects are detrimental to the user depends on the age and tolerance of the person consuming the drug. Studies show that cannabis use, especially early onset use (before age 15), is associated with increased delinquent behaviour, future employment and financial issues, mental health problems and substance abuse (Fergusson et al., 1996). This may be due to a sensitive period of cognitive development at this age, during which the impact of cannabinoid receptors in the brain hinder normal development (Pope et al., 2003). Moreover, cannabis may be more toxic to the developing brain than it is to mature brains, causing a decrease in white matter in developing brains (see Figure 5) (Pope et al., 2003). These toxic changes occur when cannabinoid receptors interfere with normal functioning of neurotransmitters in different regions of the brain (Ameri, 1999). While many scientists may consider cannabis as a potential pharmacotherapy, research shows it may actually bring more harmful effects to the user than beneficial ones (Lotan et al., 2014). Some research even indicates that frequent marijuana use can lead to acute psychosis and manic episodes, especially in individuals with pre-existing psychotic disorders (Khan, 2009). This may be an explanation as to why some individuals experience lowered anxiety while others face anxiety-inducing effects post cannabis use. It is not uncommon for those facing heightened anxiety to hallucinate, feel paranoid, feel irrational panic or have a sudden fear of dying after smoking marijuana (Khan, 2009). In addition, frequent cannabis use can lead to even more negative consequences, including disruptions with short-term memory, lowered coordination, delayed reaction time, increased heart rate and sexual problems (Drug Free World, 2006). Thus, it is very important for an individual to do more research before making the decision to consume cannabis in any form.
LONG-TERM EFFECTS
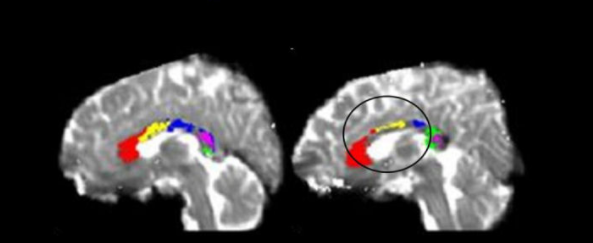
As a result of the chemical THC binding to cannabinoid 1 (CB1) receptors in the brain, observed long term morphological brain alterations connected to marijuana use are reported in CB1 receptor-enriched areas (Filbey et al, 2014). This includes regions such as the orbitofrontal cortex, amygdala, hippocampus, and cerebellum, a few of which are illustrated in figure # below (Filbey et al, 2014). Studies focusing on the physical brain effects from marijuana have found significant amounts of brain volume reductions in these CB1 enriched areas, particularly within the orbitofrontal cortex (Filbey et al, 2014). However, whether these reductions in brain volume lead to a cascade of downstream alterations in brain organization and function is still unknown. However, there is a high possibility that as a consequence of brain volume reductions, connectivity changes emerge as well (Filbey et al, 2014). These connectivity declines are currently a possible explanation for why someone who has used marijuana over long periods of time may appear cognitively slower.
A study done by Filbey et al used high-resolution MRI techniques to obtain brain images from a cohort of chronic cannabis users, in comparison to age- and sex-matched nonusing controls. Their obtained images revealed a significant decline in gray matter volume in the orbitofrontal cortex (OFC) in the marijuana users in comparison to the controls (Filbey et al, 2014). The OFC is the primary region in the reward network, and it is also enriched with CB1 receptors, which helps explain why it was mainly targeted in the chronic marijuana users. However, the cannabis group also showed higher levels of functional connectivity within the OFC compared with the control group, this can be seen in figure # below. These findings could help explain why marijuana users claim to experience feelings of creativity.
Additionally, the effects of cannabis may be beneficial to white matter by regulating mitochondrial activity and antioxidant processes, consequently protecting neurons on the molecular level (Filbey et al, 2014). These results suggest that OFC grey matter has higher vulnerability to the neurotoxic effects of cannabis use. In terms of cognition, marijuana use can cause functional impairment, however, the degree and/or duration of the impairment depends on the age when an individual initially began using and the duration of their use (Abuse, 2017). A large longitudinal study in New Zealand focused on the effects of marijuana as a result of age. Their findings revealed that persistent marijuana use beginning in adolescence was strongly associated with a loss of six to eight IQ points, as measured in mid-adulthood (Abuse, 2017). Significantly, those who partook in marijuana use heavily as teenagers but quit in adulthood, did not recover their lost IQ points (Abuse, 2017). Conversely, those who began using marijuana heavily in adulthood did not lose any IQ points (Abuse, 2017). These results suggest that marijuana has its strongest long-term impact on younger individuals, whose brains are still maturing and building new connections. Another study conducted by Zalesky et al expanded on the idea of cannabis use in adolescence and revealed that THC is hazardous to white matter of developing brains. However, he also suggests that the level of harm it elicits on white matter diminishes with age.
MECHANISM OF ACTION
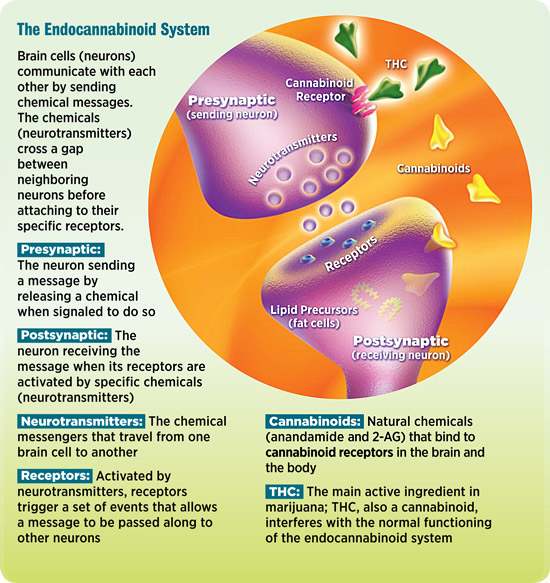
Marijuana’s active ingredient, delta-9-tetrahydrocannabinol (THC) targets the endocannabinoid system, which is one the communication systems within the brain and body. This system is part of the CNS and is highly integrated with the full function of the body. There are 2 main parts of the endocannabinoid system, the cannabinoid (CB) receptors and the cannabinoids which act on these receptors (neurotransmitters). The human body produces natural cannabinoids called anandamide and 2-AG (arachidonoyl glycerol). THC is an agonist of these neurotransmitters and competes with the natural cannabinoids produced by the body (Scholastic, 2011).
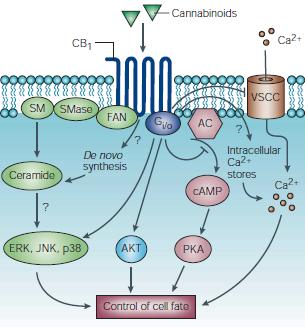
Specifically there are 2 main CB receptors, CB1 receptors, which are abundant in the CNS and many parts of the brain, and the CB2 receptors whicher are found in tissues associated with immune function such as the spleen, leukocytes, and bone marrow. Particularly, CB1 receptors are the focus of the effects of marijuana on the brain (Scholastic, 2011).
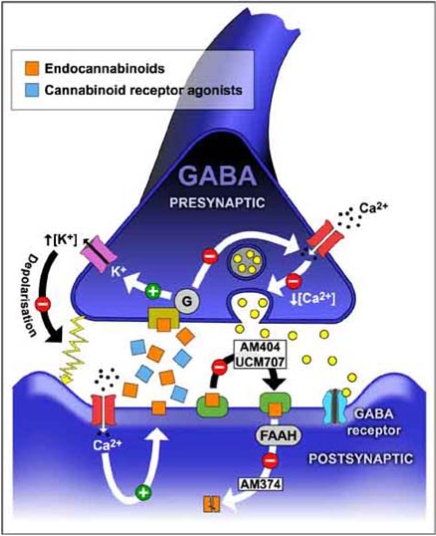
Most nervous communication systems, neurotransmitter pathways start from vesicles inside the presynaptic cleft, exiting the presynaptic cleft and binding to receptors on the postsynaptic cleft. In contrast, specifically CB1 receptors are located on the presynaptic cleft, while anandamide and 2-AG are produced at the postsynaptic site, further released to bind to the CB1 receptors located on the pre-synaptic cleft. This reverse mechanism gives rise to its ultimate function, controlling all physiological changes induced by the neurotransmitters that create synapses from presynaptic to postsynaptic neurons (Iverson, L., 2003). Cannabinoids alter neurotransmitter trafficking and concentrations by controlling the mechanisms occurring in the presynaptic cleft, having to do with the release of many transmitters. In essence, cannabinoids are known as “dimmer switches” particularly due to how they modulate the prolonged or transient reduction of neurotransmitters. Specific physiological changes observed are the reduction of calcium uptake of pre-synaptic neurons, which are the main triggers of releasing neurotransmitter filled vesicles, as well as an increase of potassium which minimizes depolarization, dampening synapse activation (Iverson, L., 2003).
When marijuana is smoked, or administered into the body in other ways, THC, being an agonist of these natural cannabinoids, has a great concentration and is able to bind to these CB1 receptors in the brain (Scholastic, 2011). They override the natural system and takeover completely, having various effects such as slowing down reaction time, decrease function of short-term memory, affected judgment or cause of anxiety. In addition, THC triggers areas of the brain that make you feel good, known as the “high” (Scholastic, 2011).
The binding of THC initiates a signal transduction which essentially has 4 targets: adenylate cyclase, calcium channels, potassium channels, kinases and ceramides (Vathi, S., 2013). Adenyl cyclase modulation leads to an increase or decrease in cAMP, in this a decrease, further causing a decrease in calcium from intracellular stores located in the pre-synaptic cleft. For potassium channels, cannabinoids act on the Kir and Ka channels, which allows greater influx of potassium in the presynaptic cleft, causing hyperpolarization, in other words, a decrease in depolarization occurs (Vathi, S., 2013). We also see these CB1 receptors associated with enzymes that hydrolyze shingomyelin to ceramide and phosphocholine. These act as second messengers with activate pathways such as Raf1 and ERK. We also see proliferation and differentiation activated such as the JNK and p38 MAPK pathways (Vathi, S., 2013).
EFFECTS OF MARIJUANA ON THE BRAIN VIDEOS
EFFECTS OF MARIJUANA ON THE BRAIN POWERPOINT
References
Abuse, N.I. (2017). What are marijuana’s long-term effects on the brain? Retrieved April 01, 2017, from http://www.drugabuse.gov/publications/marijuana/what-are-marijuanas-long-term-effects-brain
Abush, H., & Akirav, I. (2012). Short-and long-term cognitive effects of chronic cannabinoids administration in late-adolescence rats. PLoS One, 7(2), e31731.
Ameri, Angela. “The Effects Of Cannabinoids On The Brain”. Progress in Neurobiology 58.4 (1999): 315-348. Web.
Arnone, D., Barrick, T. R., Chengappa, S., Mackay, C. E., Clark, C. A., & Abou-Saleh, M. T. (2008). Corpus callosum damage in heavy marijuana use: preliminary evidence from diffusion tensor tractography and tract-based spatial statistics. Neuroimage, 41(3), 1067-1074.
Bello, J. (2007). The Benefits of Marijuana: Physical, Psychological and Spiritual. Lifeservices Press.
Block, R. I., O'leary, D. S., Ehrhardt, J. C., Augustinack, J. C., Ghoneim, M. M., Arndt, S., & Hall, J. A. (2000). Effects of frequent marijuana use on brain tissue volume and composition. Neuroreport, 11(3), 491-496.
Block, R. I., O'leary, D. S., Ehrhardt, J. C., Augustinack, J. C., Ghoneim, M. M., Arndt, S., & Hall, J. A. (2000). Effects of frequent marijuana use on brain tissue volume and composition. Neuroreport, 11(3), 491-496.
Bolla, K. I., Brown, K., Eldreth, D., Tate, K., & Cadet, J. L. (2002). Dose-related neurocognitive effects of marijuana use. Neurology, 59(9), 1337-1343.
Bonsor, K., & Gerbis, N. (2001). How Marijuana Works. Retrieved April 02, 2017, from http://science.howstuffworks.com/marijuana3.htm
Borgelt, L. M., Franson, K. L., Nussbaum, A. M., & Wang, G. S. (2013). The pharmacologic and clinical effects of medical cannabis. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy, 33(2), 195-209.
Brock, Tom. “CANNABINOID SIGNALING: THE ORIGINAL RETROGRADE SIGNALING PATHWAY”. Caymanchem.com. N.p., 2008. Web. 2 Apr. 2017.
Caulkins, J. P., Kilmer, B., & Kleiman, M. A. (2016). Marijuana Legalization: What Everyone Needs to Know?. Oxford University Press.
Cohen, J. A., & Rudick, R. A. (Eds.). (2007). Multiple sclerosis therapeutics. CRC Press.
Deem, R. (2013). The Medical “Benefits” of Smoking Marijuana (Cannabis): a Review of the Current Scientific Literatureby Rich Deem. Retrieved April 01, 2017, from http://www.godandscience.org/doctrine/medical_marijuana_review.html
Degenhardt, Louisa, Alize J. Ferrari, Bianca Calabria, Wayne D. Hall, Rosana E. Norman, John Mcgrath, Abraham D. Flaxman, Rebecca E. Engell, Greg D. Freedman, Harvey A. Whiteford, and Theo Vos. “The Global Epidemiology and Contribution of Cannabis Use and Dependence to the Global Burden of Disease: Results from the GBD 2010 Study.” PLoS ONE 8.10 (2013): n. pag. Web.
Fergusson, D. M., Lynskey, M. T., & Horwood, L. J. (1996). The short-term consequences of early onset cannabis use. Journal of abnormal child psychology, 24(4), 499-512.
Filbey, F. M., Aslan, S., Calhoun, V. D., Spence, J. S., Damaraju, E., Caprihan, A., & Segall, J. (2014). Long-term effects of marijuana use on the brain. Proceedings of the National Academy of Sciences, 111(47), 16913-16918.
Foltin, R. W., Fischman, M. W., & Byrne, M. F. (1988). Effects of smoked marijuana on food intake and body weight of humans living in a residential laboratory. Appetite, 11(1), 1-14.
Gupta, S. (2013). Why I changed my mind on weed. CNN. com, 9.
Hendershot, C. S., Magnan, R. E., & Bryan, A. D. (2010). Associations of marijuana use and sex-related marijuana expectancies with HIV/STD risk behavior in high-risk adolescents. Psychology of Addictive Behaviors, 24(3), 404.
Hoffmann, D. E., & Weber, E. (2010). Medical marijuana and the law. New England Journal of Medicine, 362(16), 1453-1457.
H. (2015, September 17). The Effects Of Weed On Your Health. Retrieved April 01, 2017, from http://herb.co/2015/09/17/the-effects-of-weed-on-your-health/ Iversen, L. “Cannabis And The Brain”. Brain 126.6 (2003): 1252-1270. Web.
Jones, K. A., Blagrove, M., & Parrott, A. C. (2009). Cannabis and Ecstasy/MDMA: empirical measures of creativity in recreational users. Journal of psychoactive drugs, 41(4), 323-329.
Khan, M. A., & Akella, S. (2009). Cannabis-induced bipolar disorder with psychotic features: a case report. Psychiatry (1550-5952), 6(12).
Lee, C. M., Neighbors, C., & Woods, B. A. (2007). Marijuana motives: Young adults' reasons for using marijuana. Addictive behaviors, 32(7), 1384-1394.
Lotan, I., Treves, T. A., Roditi, Y., & Djaldetti, R. (2014). Cannabis (Medical Marijuana) Treatment for Motor and Non–Motor Symptoms of Parkinson Disease: An Open-Label Observational Study. Clinical neuropharmacology, 37(2), 41-44.
Murnion, B. (2015). Medicinal cannabis. Australian prescriber, 38(6), 212.
Osborne, G. B., & Fogel, C. (2008). Understanding the motivations for recreational marijuana use among adult Canadians. Substance use & misuse, 43(3-4), 539-572.
Pope, H. G., Gruber, A. J., Hudson, J. I., Cohane, G., Huestis, M. A., & Yurgelun-Todd, D. (2003). Early-onset cannabis use and cognitive deficits: what is the nature of the association?. Drug and alcohol dependence, 69(3), 303-310.
“Prevalence and correlates of marijuana use in Canada, 2012.” Government of Canada, Statistics Canada. N.p., 27 Nov. 2015. Web. 02 Apr. 2017.
Short- & Long-Term Effects of Marijuana - Negative Side Effects of Weed - Drug-Free World. (n.d.). Retrieved April 01, 2017, from http://www.drugfreeworld.org/drugfacts/marijuana/short-and-long-term-effects.html
Richard, O. N., & Paul, O. B. Medical Marijuana: Basic Scientific View.
Rosenthal, E., & Newhart, S. (2002). Marijuana Gold: Trash to Stash. Ed Rosenthal.
“The Science Of Marijuana: How THC Affects The Brain”. Headsup.scholastic.com. N.p., 2011. Web. 2 Apr. 2017.
“The Science Of The Endocannabinoid System: How THC Affects The Brain And The Body”. Headsup.scholastic.com. N.p., 2011. Web. 2 Apr. 2017.
Vathi, Sonila. “Endocannabinoid System: Key Regulatory Enzymes And Physio-Pathological Implications”. Flipper.diff.org. N.p., 2014. Web. 2 Apr. 2017.