Table of Contents
Concussion
Introduction
Concussions, also known as mild traumatic brain injury (TBI), are head injuries that occur after a blunt force to the head resulting in the brain moving back and forth. Interestingly, the word concussion comes from the Latin word conutere, which means “to shake violently” (Bhandari, 2019). Concussions are commonly caused by events such as car accidents, falls, sports injuries, and assaults. The impact on brain injury varies depending on the severity of the hit. The most commonly observed signs and symptoms of concussions are headaches, dizziness, nausea or vomiting, and slow reaction to stimuli (Healthline, 2017). People who experience a concussion usually recover quickly, but in some extreme cases, symptoms can last for days or weeks. Though one concussion is unlikely to do brain damage, repeated hits to the head can have severe impacts on the brain and affect brain functioning. It is estimated that athletes in the U.S. experience about 300,000 concussions each year (“11 Facts About Concussions,” n.d.). It is important to seek medical attention after experiencing a concussion. If a second concussion is experienced before the first concussion has time to recover, serious complications can arise.
Cause
Cerebrospinal fluid (CSF) is a colorless and transparent fluid inside the skull that encompasses and preserves the central nervous system consisting of the brain and spinal cord. Cerebrospinal fluid cushions the brain and spinal cord, assisting in preventing any abrupt movements, brain damages, and jolts and bumps. Any violent hit to the head, neck and thus to the central nervous system can lead the brain to slide backwards and forwards forcibly against the inner walls of the skull, thus rupturing blood vessels and injuring the nerve tissues which in turn cause the accumulation of blood. Concussions are most frequently caused by events, including car accidents, sports injuries, cycling accidents, falls, playground coincidences in children, assaults and other traumatic events causing brain injuries. These mentioned causal events and injuries may affect regular brain functioning, leading to the signs and symptoms of concussion.
Signs & Symptoms
Signs and symptoms of a concussion vary and mainly depends on both the individual being injured and the severity of the damage as well. Therefore, it is significantly crucial and highly recommended to recognize the signs and symptoms that one can experience from concussions. The most common physical signs of a concussion may include headache, hearing ringing noises in the ear, nausea, vomiting, blurry vision, dizziness, slurred speech, and tiredness. It is worth mentioning that in some cases, the signs and symptoms may not begin immediately after a concussion and thus starts developing hours, days, weeks, or months after the injury. The common non-immediate symptoms may include amnesia, which is a partial or total loss of memory, depression, irritability, lack of concentration, disturbed sleep, and sensitivity to light. Furthermore, in the case of experiencing any of the symptoms, including prolonged headache, persistent dizziness, constant memory loss, and loss of sense of smell or taste, immediate medical care would be required. Concussion signs are known to be more challenging to encounter in young children as they may not be able to describe their feelings and symptoms, including altered appetite, walking or standing unsteadily, irritability, and altered sleep patterns. Children experiencing some severe signs and symptoms including loss of consciousness, bleeding from nose or ears, seizure, prolonged dizziness and headache, confusion, blurred vision need emergency medical care.
Diagnosis
As there is no biomarker for concussion, the current basis of concussion diagnosis is using a symptom scale. Symptoms are self-reported after an individual has experienced a hit to the head or whiplash. Relying on the individual’s self-report of symptoms is complicated as the individual may underreport (Anderson et al., 2013). Using various evaluation tools, such as symptom scales, neurological assessments, and cognitive testing, may increase the specificity of concussion diagnosis. The neurological assessment evaluates the individual’s vision, hearing, strength, balance, coordination, and refluxes. Cognitive testing evaluates serval factors including memory, concentration, and ability to recall information (Mayo Clinic, 2020).
To diagnose more severe head and brain injuries, neuroimaging techniques such as computed technology (CT) and magnetic resonance imaging (MRI) are used. Neuroimaging can also determine whether the injury has caused bleeding or swelling in the skull.
A CT scan uses a series of X-rays to obtain cross-sectional images of the skull and brain. Since CT scans tend to be more accessible in emergency rooms, it is the most common imaging technique used to clinically assess head trauma (Belanger et al., 2007).
MRI uses powerful magnets and radio waves to build up detailed images of the brain; and is also used to detect structural changes in the brain (Mayo Clinic, 2020).
fMRI (functional magnetic resonance imaging) recognizes functional changes in the brain while the individual is asked to engage in cognitive tasks (Cognitivefx, 2018).
Pathogenesis
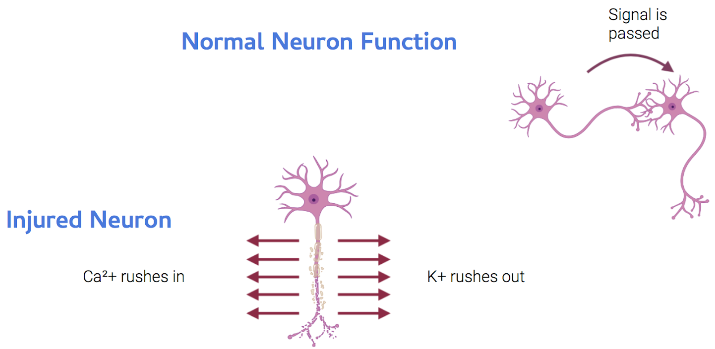 Figure 3: During injury, neurons release potassium out of the cell body and calcium ions rush into the cell causing metabolic dysfunction.
Figure 3: During injury, neurons release potassium out of the cell body and calcium ions rush into the cell causing metabolic dysfunction.
Concussions occur with any type of external force to the head, these events cause the brain to accelerate and decelerate with either translational, rotational, and/or angular force. The injury can result through the initial movement of the skull, onto the frontal lobe being stuck inside of the skull (known as contusion). This then leads to the rebound injury to the occipital lobe which results in the stretching and tearing of neurons in the brain stem and throughout the brain. This is a form of deceleration injury in a linear manner. Rotational injury happens when the brain rotates on axis causing stretching and tearing of axons. This then results in the stretching and tearing of blood vessels which causes a hematoma. Lastly, as the brain strikes the skull it causes contusion. It is believed that this leads to a wave of energy that passes through the brain triggering neuronal dysfunction. This then results in the cascade of ionic, metabolic, physiologic and neurometabolic cascade of concussion. In normal neuron function, the components of a neuron are the dendrites, nerve cell body, axon, and synapse where the signal arrives at the neuron and travels down to another axon. Neurotransmitters are released accordingly in order to trigger the next cell with a specific coded message. During injury, the neuron releases Potassium which rushes out of the cell body and calcium ions rush into the cell which causes metabolic dysfunction.
Prognosis
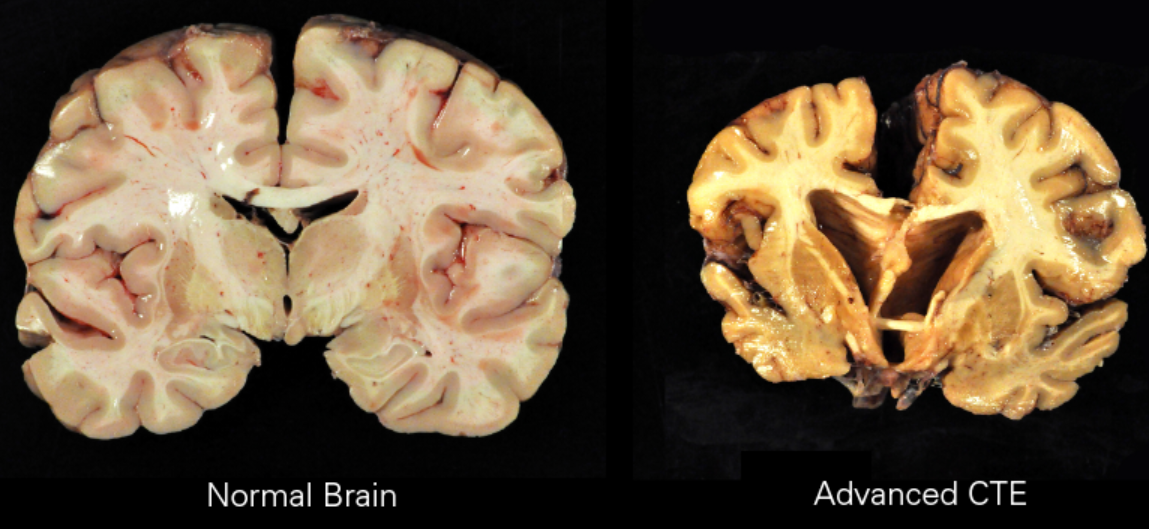
Chronic traumatic encephalopathy (CTE)
Like Alzheimer’s, CTE is a form of tauopathy, a class of neurodegenerative diseases involving the aggregation of tau proteins in the brain. The disease is caused by repeated injuries to the head. Although the exact amount of trauma required for the condition to occur is unknown it is believed to take many years to develop (Asken et al., 2017). Most documented cases have occurred in athletes involved in contact sports such as boxing, football, and hockey (Mckee et al., 2009). CTE is a progressive disease meaning the symptoms can worsen over time leading to problems like memory loss and suicidality. Those with CTE can experience a broad range of symptoms but generally they result in behavioural, mood, and cognitive problems (Asken et al., 2017).
Second impact syndrome
Second Impact Syndrome (SIS) occurs when the brain swells rapidly after a person suffers a second concussion before symptoms from an earlier one has subsided. This second blow may occur minutes, days or weeks after an initial concussion, and even the mildest concussion can lead to SIS. The condition is often fatal, and almost everyone who is not killed is severely disabled. The cause of SIS is uncertain, but it is thought that the brain's arterioles lose their ability to regulate their diameter, and therefore lose control over cerebral blood flow, causing massive cerebral edema (Cantu, 2011).
Post-concussion syndrome
In post-concussion syndrome, symptoms do not resolve for weeks, months, or years after a concussion, and may occasionally be permanent. The question of whether the syndrome is due to structural damage or other factors such as psychological ones, or a combination of these, has long been the subject of debate (Mittenberg & Strauman, 2000).
Cumulative effects
The severity of concussions and their symptoms may worsen with successive injuries, even if a subsequent injury occurs months or years after an initial one (Harmon, 1999). Cumulative effects may include psychiatric disorders and loss of long-term memory. For example, the risk of developing clinical depression has been found to be significantly greater for retired football players with a history of three or more concussions than for those with no concussion history. Three or more concussions is also associated with a fivefold greater chance of developing Alzheimer's disease and a threefold greater chance of developing memory deficits (Cantu, 2007).
Statistics
The word concussion comes from the Latin word conutere, which means “to shake violently” (Bhandari, 2019).
Youth are more at risk for concussion as their brain is still developing (CDC, 2019).
One can get a concussion from whiplash, not just direct contact (CDC, 2019).
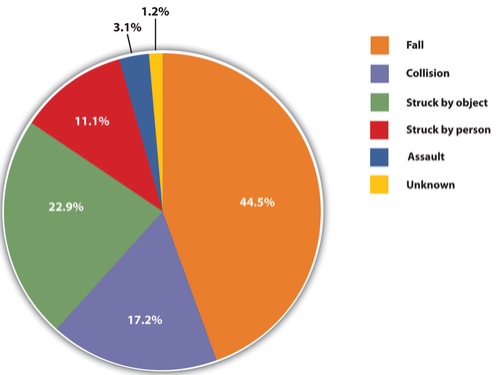
In 2014, falls were the leading cause of a traumatic brain injury (TBI). Falls accounted for almost half (48%) of all TBI-related emergency department visits and affected children (age 17 or younger) and older adults (age 65 and older) (CDC, 2019).
Concussions occur in all sports with the highest incidence in football, hockey, rugby, soccer, and basketball (Harmon et al., 2013).
5 of 10 cases of concussions go unreported or undetected in the U.S (CDC, 2019).
Treatment
There are three main forms of treatment that are used to alleviate the side effects of concussions. The first being physical and mental rest, rest is appropriate in order for the brain to recover, both physically and mentally. Relative rest includes the limiting of activities that require thinking and mental concentration. This is heavily imposed especially the first two days after the concussion, although rest taken to extreme levels is counterproductive. This includes lying in a dark room avoiding all stimuli. It is advised in the first 48 hours that there should be a limit of activities that require high mental concentration such as watching TV, doing schoolwork, reading, and texting. In general physical activities that increase any symptoms and exertion are to be avoided to no longer provoke symptoms. After a period of relative rest, it is recommended that there is a gradual increase in daily activities such as screen time and light exercise has shown to lead to a quick recovery. Secondly, routine activity by gradually adding more activities that involve thinking such as doing schoolwork or assignments can improve the speed of recovery. Lastly, pain relief is used to manage side effects. It is safe to have Tylenol (Acetaminophen) instead of pain relievers such as Advil, Motrin IB and Aspirin as these increase the risk of bleeding (Mayo Clinic, 2020).
Case Study - Rowan Stringer
Rowan Stringer was a grade 12 student who had recently been accepted in the University of Ottawa’s nursing program for the Fall of 2013 with the hope of becoming a paediatric nurse. However, all of this changed in May 2013
Rowan's Final 10 Days
Friday, May 3rd, 2013
Rowan captained her high school rugby team during a three-game tournament. During the second game she was hit in the head. However, she later returned to the same game. Later in the evening she complained of a headache to her mom and asked for a painkiller.
Monday, May 6th, 2013
Rowan is once again hit in the head during a game and the headaches return.
Tuesday, May 7th, 2013
Rowan doesn’t feel right. Texts messages with her friend showed she was aware she probably had a concussion. In fact, one of her texts indicated she had Googled ‘concussion.’ However, when asked if she will play the game the next day her reply was “Yeah. Nothing can stop me! Unless I’m dead.” When asked if she will get checked about her symptoms the reply was “Nope. Just see if it gets worse.” And finally, when her friend suggested seeing a Doctor Rowan said “Meh. What’s some brain damage gonna hurt.” In other messages that night Rowan referred to her injuries as “warrior wounds” and wore them with pride.
Wednesday, May 8th, 2013
Rowan is tackled and hits her head on the ground. She lost consciousness and was rushed to the hospital.
Saturday, May 11th, 2013
With no possibility of recovery Rowan’s last wish was for her heart, lungs, liver, pancreas, kidneys and corneas to be donated.
Sunday, May 12th, 2013 – Mothers day
Rowan is removed from life support. Her official cause of death was Second impact syndrome. It’s believed she never told her parents or any adults about the headaches. She was 17.
Rowan’s Law
Ontario passed Rowan's Law. This new legislation is intended to protect amateur athletes by improving concussion safety on the field and at school (Hall, 2016).
Conclusion
Overall, experiencing a concussion is not to be taken lightly. Rowan Stringer’s case serves as a prime example of how concussions can be life-threatening if left untreated. Most concussion cases result from sports injuries and 5 out of 10 cases can go undetected in the U.S (CDC, 2019). Physical and mental rest is vital to recovering and avoiding further brain damage. Moreover, seeking medical attention is important after experiencing a concussion to be assessed and rule out any potential damage.
References
Anderson, B.L.,W. J. Pomerantz, J. K. Mann, and M. A. Gittelman. (2013). “I Can't Miss the Big Game”: High School (HS) Football Players' Knowledge and Attitudes about Concussions. Presented at the Pediatric Academic Societies Annual Meeting, Washington,DC, May 6. AP(Associated Press).
Asken, B. M., Sullan, M. J., Dekosky, S. T., Jaffee, M. S., & Bauer, R. M. (2017). Research Gaps and Controversies in Chronic Traumatic Encephalopathy. JAMA Neurology, 74(10), 1255. doi: 10.1001/jamaneurol.2017.2396
Belanger, H. G., Vanderploeg, R. D., Curtiss, G., & Warden, D. L. (2007). Recent Neuroimaging Techniques in Mild Traumatic Brain Injury. The Journal of Neuropsychiatry and Clinical Neurosciences, 19(1), 5–20. doi: 10.1176/jnp.2007.19.1.5
Bhandari, S. (2019, August 28). Concussion: Symptoms, Causes, Diagnosis, Treatments, & Recovery. Retrieved from https://www.webmd.com/brain/concussion-traumatic-brain-injury-symptoms-causes-treatments#1
Cantu, R. C. (2007). Chronic Traumatic Encephalopathy In The National Football League. Neurosurgery, 61(2), 223–225. doi:10.1227/01.neu.0000255514.73967.90
Cantu, R. (2011). Second Impact Syndrome: Concussion and Second Injury Brain Complications. Yearbook of Sports Medicine, 2011, 26–28. doi: 10.1016/j.yspm.2011.03.046
Centers for Disease Control and Prevention (2019). Surveillance Report of Traumatic Brain Injury-related Emergency Department Visits, Hospitalizations, and Deaths—United States, 2014. Centers for Disease Control and Prevention, U.S. Department of Health and Human Services.
Concussion. (2020, February 22). Retrieved from https://www.mayoclinic.org/diseases-conditions/concussion/diagnosis-treatment/drc-20355600
Gioia, G. A., Collins, M., & Isquith, P. K. (2008). Improving identification and diagnosis of mild traumatic brain injury with evidence: psychometric support for the acute concussion evaluation. The Journal of head trauma rehabilitation, 23(4), 230-242.
FX, C. (2018). Diagnosing Concussion with functional NeuroCognitive Imaging. Retrieved from https://www.cognitivefxusa.com/blog/diagnosing-concussion-with-functional-neurocognitive-imaging
Hall, V. (2016). Rowan's Law: How the death of one teen is serving as a wake-up call for Canada on handling youth concussions. Retrieved from https://nationalpost.com/features/rowans-law
Harmon, K. G. (1999). Assessment and management of concussion in sports. Am Fam Physician 60, 887–892, 894.
Harmon, K. G., Drezner, J., Gammons, M., Guskiewicz, K., Halstead, M., Herring, S.,… Roberts, W. (2013). American Medical Society for Sports Medicine Position Statement. Clinical Journal of Sport Medicine, 23(1), 1–18. doi: 10.1097/jsm.0b013e31827f5f93
Healthline. (2017) Concussion. Retrieved from https://www.healthline.com/health/concussion
Mckee A. C., et al. (2009). Chronic Traumatic Encephalopathy in Athletes: Progressive Tauopathy After Repetitive Head Injury. Journal of Neuropathology & Experimental Neurology, 68(7), 709–735. doi: 10.1097/nen.0b013e3181a9d503
Mittenberg, W., & Strauman, S. (2000). Diagnosis of Mild Head Injury and the Postconcussion Syndrome. Journal of Head Trauma Rehabilitation, 15(2), 783–791. doi: 10.1097/00001199-200004000-00003
Piland, Scott & Motl, Robert & Ferrara, Michael & Peterson, Connie. (2003). Evidence for the Factorial and Construct Validity of a Self-Report Concussion Symptoms Scale. Journal of athletic training. 38. 104-112.
What Is a Concussion? (2019, February 12). Retrieved from https://www.cdc.gov/headsup/basics/concussion_whatis.html
11 Facts About Concussions. (n.d.). Retrieved from https://www.dosomething.org/us/facts/11-facts-about-concussions