Table of Contents
Migraines
A migraine is a primary headache disorder that is characterized by recurrent throbbing head pain. It should be noted that individuals who do experience migraines have characteristic differences in comparison to a typical headache. These differences include increased severity, length, localization of pain to one side of the head and other associated symptoms (such as vomiting, nausea, sensitivity to light and smell). Individuals with migraines may or may not experience an aura, which is the phenomenon of experiencing flashing lights, an orb of light, olfactory or auditory sensations prior, or during a migraine (Ferrari, Klever, Terwindt, Ayata, & van den Maagdenberg, 2015). Migraines are included in the broad class of neurovascular disorders, as they mainly result from cortical spreading and the activation of trigeminovascular system (Hargreaves & Shepheard, 1999). The underlying mechanism of migraines is relatively unknown, but it is associated with a single nucleotide polymorphism on chromosome 8 or a frameshift mutation in the KCNK18 gene (Watson, 2011). Migraines are typically diagnosed by symptoms, past family history and through examinations. There are many different forms of treatment, focusing mainly on acute pain as well as preventative measures (Mayoclinic.org, 2017).
Epidemiology
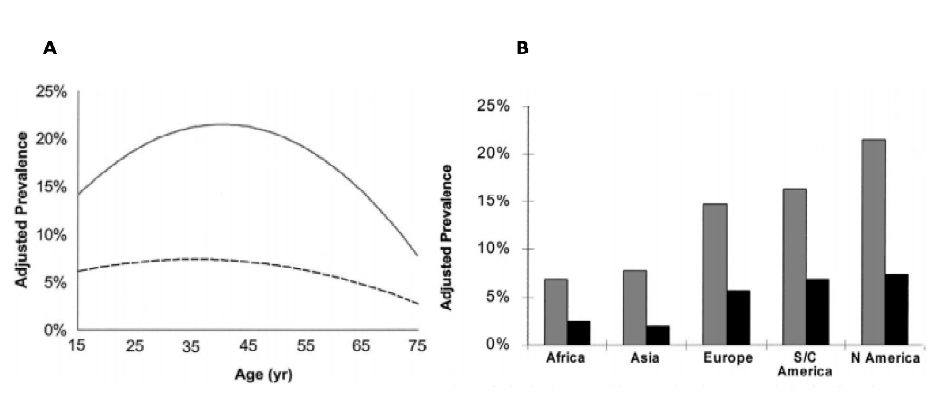
Migraines affect 8.3% of Canadians, which accounts for 2.7 million individuals. Worldwide, it is estimated to affect 14% of the entire population (Ramage-Morin & Gilmour, 2014). It should be noted that these estimates may fall short of the actual prevalence of migraines, as not many individuals actively seek medical assistance when affected (Ramage-Morin & Gilmour, 2014). Migraine prevalence is correlated with age, sex, race, geographic distribution, and socioeconomic factors. It has been found that migraines with auras occur earlier in males and females compared to migraines without. However, males tend to have migraines earlier on in life regardless of the presence of auras. Following puberty, females report migraines more frequently than males. Both sexes report having migraines within the age range of 25 to 55, followed by a decline as seen in Figure 1a (Ramage-Morin & Gilmour, 2014). Overall, it is found that females report migraines more frequently than males. In an American study, it was discovered that Caucasians tend to have the highest prevalence of migraines, while Asian Americans have the lowest. Geographically, data tends to support this finding as North and South Americans were observed to report migraines the most, while individuals in Asia reported migraines the least, as seen in Figure 1b. Typically, socioeconomic status is inversely proportional to the prevalence of migraines in a population (Lipton & Bigal, 2005).
Figure 1a: The prevalence of migraines globally by age. On average, both males and females experience the migraines between the ages of 25-55, but females tend to have migraines more often than do males (Ramage-Morin & Gilmour, 2014). Figure 1b: The prevalence of migraines by geographic location. Both males (grey) and females (black) in North America report migraines the most, while females in Asia report migraines the least (Lipton & Bigal, 2005).
Etiology
Potential causes that trigger migraine onset is currently not completely understood. However, variables such as external and biological factors have shown to play a significant role in multiple academic studies.
Stress and Mood
A major culprit to migraine onset in those predisposed to migraine attacks (migraineurs) are stress and critical changes in mood which is the most common self-reported factor ranging as much as 62% in patients (Robbins, 1994). For instance, in a study conducted by Wacogne and colleagues (2003), 141 migraineurs were compared with a control group of 109 non-migraineurs for the intensity of stress, anxiety and depression. Using the Perceived Stress Questionnaire, stress was measured, while anxiety and depression were measured via the Hospital Anxiety and Depression Scale. By the end of the investigation, researchers observed that the migraine group had significantly higher levels of stress and anxiety than the control group (Wacogne et al., 2003). A key finding was that “stress was a primordial factor in the triggering and perpetuation of migraine attacks” (Wacogne et al., 2003). In addition, impatience, unusual fatigue, intrusive thoughts, and irritability were also shown to be constant key indicators towards migraine onset based on the questionnaires used in the study (Wacogne et al., 2003).
Similar findings were shown in another study conducted by Hashizume and colleagues (2008). Stress and significant shifts in mood were examined over 1-3 days before a suspected migraine. During this time, participants recorded – four times a day biweekly – for migraine severity, stressful event occurrence, domestic and non-domestic stress, daily burdens, and any anxiety or depressive episode experiences. Overall, final results concluded that there was an evident change in various modes of psychosocial stress in advance of a migraine attack on the days when migraines were recorded. (Hashizume et al., 2008). Such stress-related variables were thus confirmed to be correlated to migraines by a significant degree, thus playing an important role in migraine frequency and occurrence (Hashizume et al., 2008).
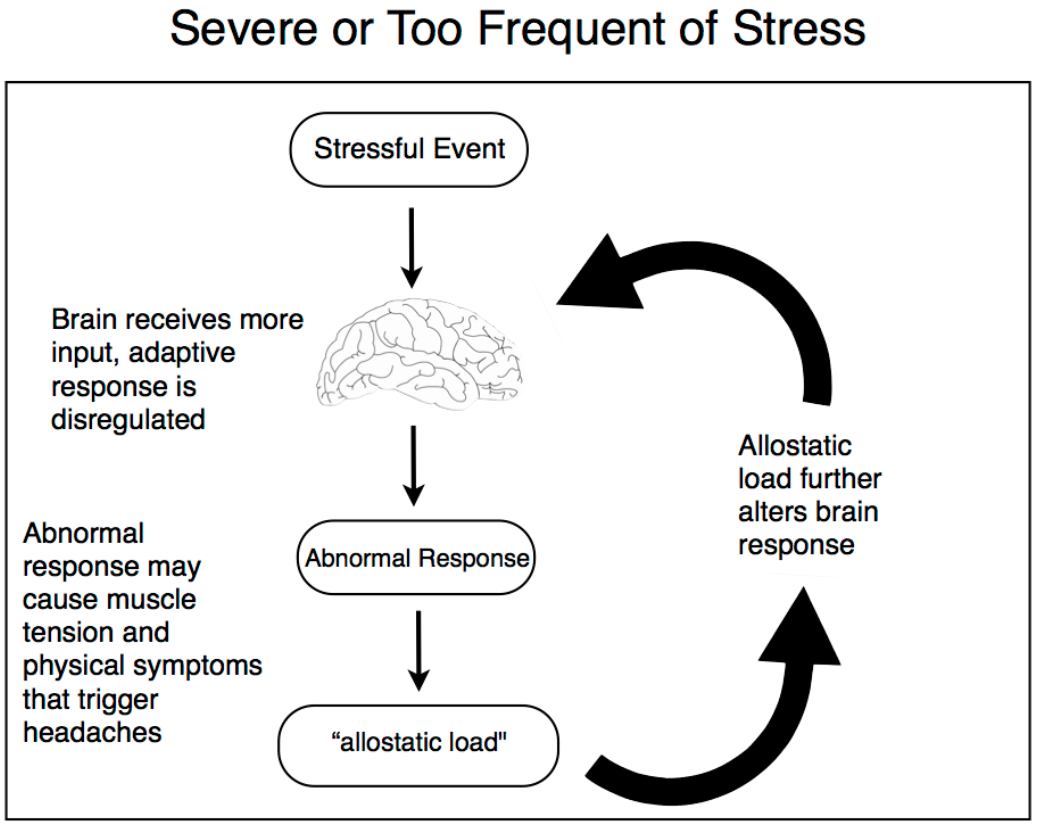
Significant evidence has also displayed the cyclic nature of migraines, particularly how migraines themselves act as a stressor leading to a positive feedback and increase of migraine severity and frequency, as seen in Figure 2 (Sauro & Becker, 2009). A noteworthy investigation lead by Holm and colleagues (1997), looked at the daily temporal relationship between migraines, appraisal, coping and stress in a group of migraineurs. From this group, it was observed that 50-70% of participants showed a significant and meaningful correlation between their recorded days of migraine attacks and days of major stress (Holm et al., 1997). In addition, migraine severity also showed to steadily increase over time, further supporting the hypothesis that migraines and stress are reciprocal and cyclically influence one another (Holm et al., 1997).
Food and Drink
Another potential cause for migraines is certain dietary triggers. These food and drink-related triggers affect the release of neurotransmitters (serotonin and norepinephrine) that induce vasoconstriction, vasodilation and directly affect the brainstem, trigeminal ganglia and cortical neuronal pathways in the brain. Foods of noteworthy interest include items high in sodium, cheese, processed food, and preservatives (Millichap & Yee, 2003). Chocolate is also of high interest, based on the numerous studies focusing on its migraine-inducing effects. For instance, in a double-blind parallel study, migraineurs were either given regular chocolate or a placebo (Gibb et al., 1991). What was observed following ingestion was a migraine episode in 5 patients, out of a total of 12 who ate the regular chocolate. However, no patients out of the 8 in the placebo group had a migraine attack, showing significant evidence that chocolate had the capability to induce migraines in certain individuals (Gibb et al., 1991).
Another item of high interest is alcohol, specifically red wine, which showed to provoke migraines in individuals as well. In a study conducted by Littlewood and colleagues (1998), participants were either given red wine, vodka or a diluted alcohol mixture. Results from this study showed a similar effect, with red wine having the highest number of migraine attacks in a group, with 9 out of the 11 patients experiencing an attack (Littlewood et al., 1988). However, no patients out of the 8 with vodka experienced a migraine, showing significance towards red wine being a potential trigger to migraine onset (Littlewood et al., 1988).
Lack of food and drink has also been seen to provoke migraine onset as well, as much as 40% in patients in one study (Robbins, 1994). Hunger has been observed to have biological effects with decreased levels of serotonin, elevated prostaglandin levels, as well as elevated blood lipids and free fatty acids levels which then lead to an increase in blood platelet aggregability (Bic et al., 1998). These changes in the body related to biochemical imbalance has thus shown to affect similar vasodilatation activity that precedes a migraine attack (Bic et al., 1998).
Change in Weather
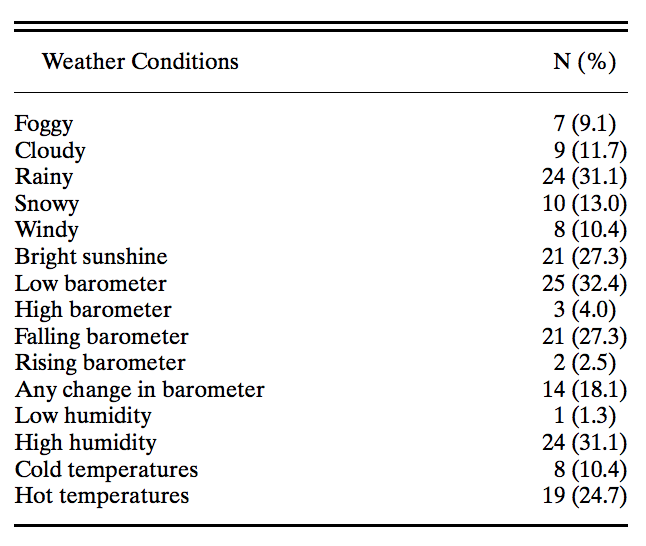
Sudden changes in weather and certain weather conditions have also been highly self-reported in migraineurs, as much as 43% of patients in one study (Robbins, 1994). In another study by Prince and colleagues (2004), 77 migraineurs provided a calendar (from 2 to 24 months) where it was seen that influences of certain weather variables had a significant impact on migraine onset, making them more susceptible. As seen in Figure 3, weather conditions that had the highest influence included low air pressure, high humidity, sudden air pressure change, and bright sunshine - each ranking highest to lowest impact respectively (Prince et al., 2004). In another study by Hoffmann and colleagues (2011), journals were written by participants in which similar results were seen. Onset of attacks with high migraine intensity was associated with lower temperature and higher humidity. This was also seen when measuring weather components such as temperature, air pressure, and relative humidity over a year.
Menustration and Female Hormones
Approximately 20 million American women suffer from migraines, and nearly 12 million have experienced increased migraine intensity during their menstrual cycle (Lay & Mascellino, 2001). This phenomenon has been correlated to the heightened estrogen levels during this time, which can play a role. This can be evidently seen in the rate of migraine onset being highest in women in their 20’s, with prevalence peaking around age 40. Afterwards, this prevalence significantly declines after menopause, where the menstrual cycle ceases in women between the ages of 40 and above (Lay & Mascellino, 2001). In a prospective study, similar observations were seen with 32% of menstruating patients reported migraine attacks, whereas only 19% were reported in the control group (Wöber et al., 2006).
Other Extraneous Factors
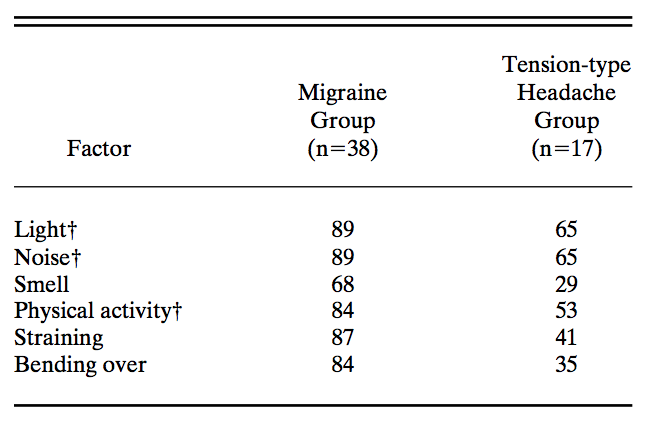
As much as 38% of patients have described that bright light, either sunlight or artificial, as well as excessive noise, were associated with their migraine pain, as seen in Figure 4 (Robbins, 1994). Another study showed that lack of sleep, and even oversleeping, was also reported as a major precipitating factor for migraine onset (Spierings, 2001).
Pathophysiology
Migraines are thought to be a neurovascular disorder, which is the result of a dysfunction in the central nervous system. There are two primary phenomena that take place when investigating migraines (Hargreaves & Shepheard, 1999). The first phenomenon is related to the activation of the trigeminovascular system which causes the pain associated with migraines. The second phenomenon is referred to as cortical spreading depression, which aims to explain the aura that is often accompanied by migraines (Hargreaves & Shepheard, 1999).
Cortical Spreading Depression
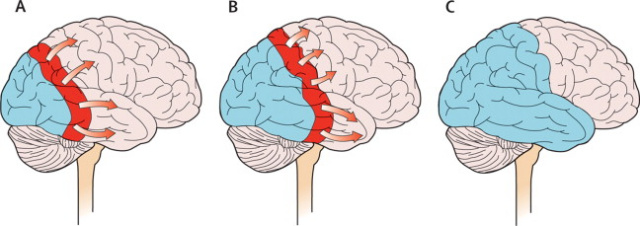
The process of Cortical Spreading Depression (CSD) explains the mechanism behind migraines with aura. Current understanding indicates that a wave of neuronal excitation found in the cortical gray matter spreads across the cerebral cortex as seen in Figure 5 (Chawla, 2018). As these neurons begin to depolarize it is thought that the aura phase is triggered. The activation of the aura phase then excites the trigeminal fibres, which causes the headache phase of a migraine (Chawla, 2018).
Pain Pathophysiology
The exact cause of the pain associated with migraines is unknown, but current theories indicate that the pain is the result of dysfunction within the central nervous system (CNS). This dysfunction causes changes in the shape of blood vessels found in the intracranial meningeal structures when triggered (Hargreaves & Shepheard, 1999). Specifically, the occuring vasodilation of these vessels, followed by the stimulation of the trigeminal sensory system causes pain. As the trigeminovascular system becomes activated, vasoactive sensory neuropeptides are released that increase the pain response (Hargreaves & Shepheard, 1999). The now activated trigeminal nerves send nociceptive information to central neurons in the brain stem, which sends these pain signals to higher brain structures where the headache pain is then perceived. As the migraine attack persists, it has been suggested that these central neurons become sensitized (Hargreaves & Shepheard, 1999).
Structures Associated with the Trigeminovascular System
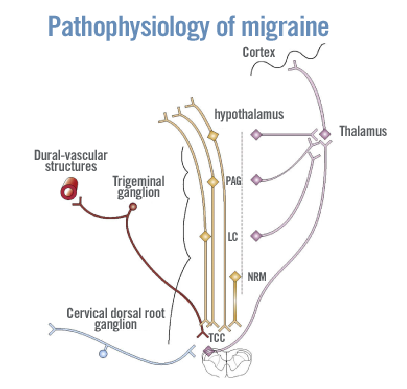
The pathway associated with migraines pain can be triggered by multiple factors such as stress, diet, weather and so forth. As seen in Figure 6 there are many major structures involved in the activation of the trigeminovascular system (Pathophysiology of Migraines, 2018). The dural vascular structures become activated from sensory neurons that are connected to the trigeminal ganglion and upper cervical dorsal roots. This input from the dural vascular structure then innervates the trigeminocervical complex (TCC) through second-order neurons (Pathophysiology of Migraines, 2018). The localization of pain is the result of nerve fibres, which ascend from the trigeminal nucleus caudalis to the thalamus, and then to the sensory cortex. The merging of projections from the trigeminal nerve at the trigeminal nucleus caudalis and upper cervical nerve roots are thought to be attributed to the perceived pain in the head and upper neck regions (Pathophysiology of Migraines, 2018).
Mechanisms
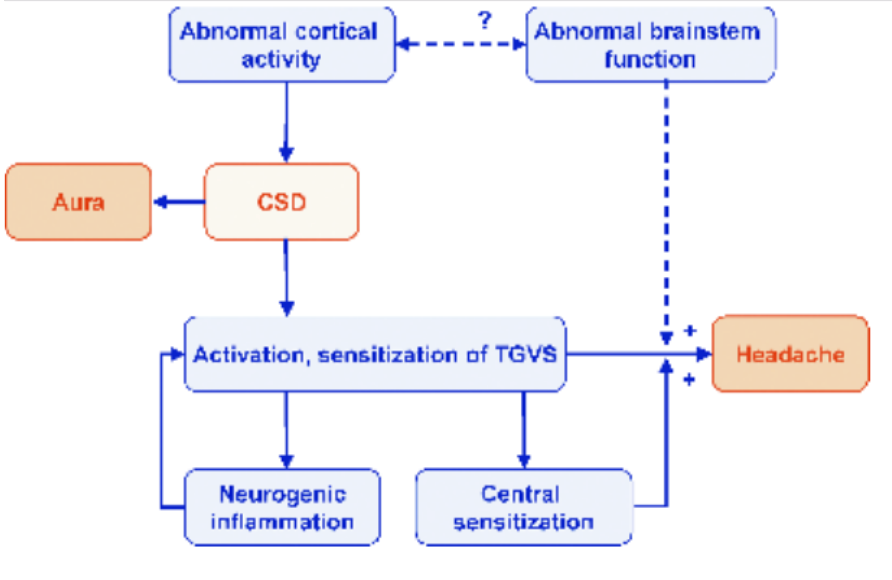
The mechanisms underlying the trigeminovascular system remain largely unknown as shown in Figure 7, such as the relationship between abnormal cortical activity and brainstem function and the relationship between dysfunctional brainstem function and the activation of trigeminal hyperexcitability (Pietrobon, 2005). One hypothesis suggests the possibility that CSD also occurs in MO (a migraine without aura) patients but the associated aura symptoms do not show because it takes place in a clinically silent area of the cerebral cortex and thus causes headache pain (Pietrobon, 2005). Another view illustrates migraine aura and headache as parallel and not sequential. Therefore, this demonstrates that the cause of a migraine is a dysfunction in the brainstem nuclei (Pietrobon, 2005). However, both these proposed hypotheses lack evidence and therefore, cannot be claimed as scientific fact.
A study that looked at 2731 migraine cases, found that 95% of individuals with migraines had a single nucleotide polymorphism in the minor allele of rs1835740 on chromosome 8q22.1 (Watson, 2011). This single nucleotide polymorphism is located between the genes encoding astrocyte elevated gene 1 (AEG-1) and plasma glutamate carboxypeptidase (PGCP), which plays a role in glutamate signalling (Watson, 2011). AEG-1 is shown to downregulate SLCA2 that is the major glutamate transporter in the brain and causes an increase in glutamate in the synaptic cleft (Watson, 2011). This results in hyperexcitability and increases the chance of migraines. Whereas, migraines with aura is characterized by a frameshift mutation in the gene, KCNK18, rather than a single nucleotide polymorphism (Watson, 2011). KCNK18 was shown to relate to the migraine trait and encodes TRESK, a TWIK-related spinal cord potassium channel, expressed in trigeminal ganglion that is activated during migraines (Watson, 2011). A mutation in this, results in the complete loss of function of the ion channel, leading to the migraine pathology.
Familial Hemiplegic Migraine
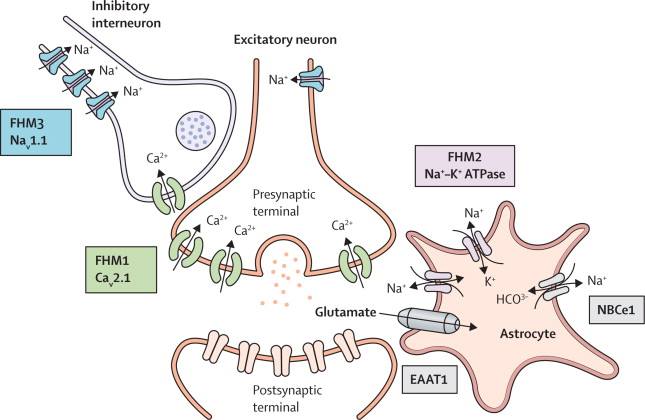
Genes associated with the cause of migraines have yet to be definitive, except for in familial hemiplegic migraine (FHM) cases, as visualized in Figure 8. FHM is a type of migraine characterized by aura symptoms mostly in the temporal order (visual, sensory, motor, aphasic) and can co-occur within families (Pietrobon, 2005). These attacks are similar to migraines with aura attacks, however, tend to last longer and may have severe attacks that include impairment of consciousness or seizures (Pietrobon, 2005). There are 3 different types of Familial Hemiplegic Migraines, which will be further explored below.
- FHM1: This is the most common type of FHM at around 50% of the cases. This migraine is characterized by mutations in CACNA1A that encodes for a pore-forming alpha1 subunit of neuronal Cav2.1 channels (located in the presynaptic terminals and somatodendritic membranes, places that have been implicated with migraines) that has 4 domains each containing 6 transmembrane regions with a voltage sensor and pore loop (Russell, 2011). These channels play a role in neurotransmitter release and have been expressed in many brain structures involving migraines such as cerebral cortex, trigeminal ganglia and brainstem nuclei. The effect of the mutation involves an influx of Ca2+ due to lower voltages of the channel activation. A study by Pietrobon (2005) demonstrates that there is also an excessive release of glutamate in relation to the Ca2+, which starts a positive feedback cycle leading to CSD (Pietrobon, 2005) This gene is related to other conditions, such as nystagmus (involuntary movement of the eyeballs) and ataxia (unsteadiness and the loss of muscle coordination).
- FHM2: This type of migraine is characterized by mutations in ATP1A2 gene encoding alpha 2 subunit or Na+, K+ and ATPase (Pietrobon, 2005). It consists of an alpha subunit (binding site) and a regulatory beta subunit. Driven by Na+ and K+ gradients, this ATPase uses energy to transport Na+ and K+ ions into cells and to clear glutamate. Mutations in the ATPase causes the exogenous pumps and endogenous pumps to act without distinction or complete malfunction of the pumps (Pietrobon, 2005). As a result, surrounding neurons begin to depolarize which causes a local build-up of K+ and enhanced glutamate concentration in the synaptic cleft. This surplus of K+ and glutamate enhances one’s susceptibility to CSD (Pietrobon, 2005). This gene has also been connected to seizures, fever, and other mental illness.
- FHM3: This type of FHM mutation is extremely rare and has minimal information regarding the mechanism. Currently, it is understood that the FHM3 is characterized by a mutation in the gene SCN1A, leading to the impairment of Nav1.1 voltage-gated Na+ channel (Russell, 2011). A few cases from a study by Russel (2011) suggests that the mutation leads to a malfunction in a glutamate transporter EAAT1 affecting glutamate uptake. Due to the lack of knowledge regarding this mutation, no information currently exists about how this mutation impacts the migraine pathways.
Diagnosis
A family physician may diagnose migraines based on medical history, family history, symptoms, physical test or they may recommend you to a neurologist to receive a neurological examination.
There are several examinations that can be done to diagnose migraines. One examination is blood tests examining problems with blood vessels, infections in the spinal cord or the brain, or other toxins in the system (Mayoclinic.org, 2017). Magnetic Resonance Imaging provides detailed images of the brain and blood vessels and helps to diagnose any tumours, strokes, bleeding in the brain, infections and other neurological conditions. A CT scan creates detailed cross-sectional images of the brain which also helps to diagnose medical problems that may be causing migraines. A spinal tap is also another examination conducted after an infection is suspected (Mayoclinic.org, 2017).
Treatment
To date, there is no actual cure for Migraines however, there are drugs that help stop symptoms and prevent future attacks. These treatments depend on the frequency, severity and the degree of disability that the migraines cause. Medication for migraines falls under two categories(Mayoclinic.org, 2017).
Pain Relievers
Pain relieving medication also known as acute treatments are taken during migraine attacks and designed to stop symptoms. For mild migraines, aspirin or ibuprofen such as Advil or Tylenol may be used to help relieve mild migraines however they are not effective alone for severe migraines (Mayoclinic.org, 2017).Pain relievers work by travelling through the body and being absorbed into the bloodstream. Once they enter the bloodstream, the blood carries the medicine to different parts of the body looking for the pain.
- Triptans:These are often used in treating migraines by stimulating serotonin causing blood vessels to constrict and block the pain pathways in the brain. This relieves pain and other symptoms, ultimately stopping the migraine (Mayoclinic.org, 2).
- Ergots: Ergots are noted to be the most effective in individuals who experience pain that lasts more than 48 hours (Mayoclinic.org, 2017). These class of drugs are effective when they are taken soon after migraine symptoms initiate as they also cause blood vessels in the body to constrict (Ramsey, 2018).
- Anti-nausea Medications: This class of medication is usually combined with other medications but used to treat nausea, one of the main symptom associated with migraines (Mayoclinic.org, 2017).
- Opioid Medications: When patients are unable to take triptans or ergots, they are often prescribed opioids to treat migraine pain as a replacement (Mayoclinic.org, 2017).
- Glucocorticoids: Glucocorticoids may be used with other medications to improve pain relief from migraines(Mayoclinic.org, 2017).
Preventive Medications (Proactive)
Preventative Medications differ as they are only prescribed if the patients experience four or more devastating attacks a month that lasts more than 12 hours, pain relieving medications are not helping and migraine signs and symptoms include a prolonged aura or any numbness and weakness. These medications reduce the frequency, severity, length of the migraines and relieve the symptoms during migraine attacks. It usually takes several weeks to see improvements in symptoms but if these drugs show beneficial results and the migraines are well controlled, the doctor may recommend suspending the medication to determine if the migraines will return (Mayoclinic.org, 2017).
Common drugs that can be prescribed to reduce the frequency and severity of migraines are the following.
- Cardiovascular Drugs: Beta blockers are used to treat high blood pressure and coronary artery disease. They work by relaxing and opening up blood flow in blood vessels. They also block the effect of adrenaline which reduces blood pressure and slows the heartbeat (Mayoclinic.org, 2017).
- Antidepressants: Tricyclic antidepressants may reduce the frequency of migraines by affecting the level of serotonin and other brain chemicals (Mayoclinic.org, 2017).
- Anti-seizure Drugs: Some anti-seizure drugs also have been noticed to reduce the frequency of migraines (Mayoclinic.org, 2017).
- OnabotulinumtoxinA (Botox): OnabotulinumtoxinA has been shown to be helpful in treating chronic migraines in adults. During this procedure, the botox is injected into the muscles of the forehead and neck. Botox enters the nerve endings and blocks the release of chemicals involved in pain transmission, ultimately preventing the activation of pain in the brain. If this treatment is effective for the patient, it is usually repeated every 12 weeks (Mayoclinic.org, 2017).
Alternative Medicine
Some forms of alternative medicine are believed to relieve symptoms as well. These include Acupuncture, Biofeedback, Massage therapy, Cognitive Behavioral Therapy, Herbs, Vitamins such as Riboflavin (vitamin B-2) and Minerals (Mayoclinic.org, 2017).
Conclusion
Overall, migraines are a primary headache disorder, characterized by recurrent throbbing, heightened severity, length, localization of pain to one side of the head, amongst other symptoms (vomiting, nausea, sensitivity to light and smell). These symptoms are observed at a high prevalence rate globally by age, with females experiencing more migraines than males overall. In addition, although the causes and triggers to migraine onset remains unclear, multiple studies have observed patients being most susceptible to stress, certain foods and drink, as well as other associated environmental and biological factors (light, weather, menstruation, hunger, etc.). What can be understood currently about this phenomenon is how migraines are a neurovascular disorders, mainly due to cortical spreading and the activation of trigeminovascular system seen in the brain and central nervous system. Beyond this scope however, the rest is relatively unclear, specifically concerning the mechanisms at play. It has been theorized that migraines are associated to a single nucleotide polymorphism on chromosome 8 or a frameshift mutation in the KCNK18 gene. With this current understanding about migraines, diagnosis can be completed quickly and treatment can be implemented at any migraine stage via acute or proactive methods. Yet, despite the efforts in providing a myriad of pharmaceutical and alternative treatments to the public, more has to be done to further learn how migraines occur and how to effectively lessen their severity for individuals.
Presentation
Click presentation_1_migraines.pdf for a research seminar presentation on migraines.
Copyright © Miguel Cardoso, Shara Chowdhury, Sabrina Musto, Harpreet Pabla, & Ojan Yarkhani
References
Bic, Z., Blix, G. G., Hopp, H. P., & Leslie, F. M. (1998). In search of the ideal treatment for migraine headache. Medical hypotheses, 50(1), 1-7.
Business Insider. Retrieved 2 February 2018, from http://www.businessinsider.com/how-pain-relievers-tylenol-ibuprofen-work-2016-10
Chawla, J. (2018). Migraine Headache: Practice Essentials, Background, Pathophysiology. Emed
Ferrari, M. D., Klever, R. R., Terwindt, G. M., Ayata, C., & van den Maagdenberg, A. M. J. M. (2015). Migraine pathophysiology: lessons from mouse models and human genetics. The Lancet Neurology, 14(1), 65–80. https://doi.org/10.1016/S1474-4422(14)70220-0
Gibb, C. M., Davies, P. T. G., Glover, V., Steiner, T. J., Rose, F. C., & Sandler, M. (1991). Chocolate is a migraine-provoking agent. Cephalalgia, 11(2), 93-95.
Hargreaves, R., & Shepheard, S. (1999). Pathophysiology of Migraine — New Insights. Canadian Journal Of Neurological Sciences / Journal Canadien Des Sciences Neurologiques, 26(03),12-19. http://dx.doi.org/10.1017/s0317167100000147
Hashizume, M., Yamada, U., Sato, A., Hayashi, K., Amano, Y., Makino, M., … & Tsuboi, K. (2008). Stress and psychological factors before a migraine attack: A time-based analysis. BioPsychoSocial medicine, 2(1), 14.
Hoffmann, J., Lo, H., Neeb, L., Martus, P., & Reuter, U. (2011). Weather sensitivity in migraineurs. Journal of neurology, 258(4), 596-602.
Holm, J. E., Lokken, C., & Myers, T. C. (1997). Migraine and stress: a daily examination of temporal relationships in women migraineurs. Headache: The journal of head and face pain, 37(9), 553-558.
Lay, C. L., & Mascellino, A. M. (2001). Menstrual migraine: diagnosis and treatment. Current pain and headache reports, 5(2), 195-199.
Lipton, R. B., & Bigal, M. E. (2005). The epidemiology of migraine. The American Journal of Medicine Supplements, 118(1), 3–10. https://doi.org/10.1016/J.AMJMED.2005.01.014
Littlewood, J., Glover, V., Davies, P. T. G., Gibb, C., Sandler, M., & Rose, F. C. (1988). Red wine as a cause of migraine. The Lancet, 331(8585), 558-559.
Mayoclinic.org. (2017). Migraine - Diagnosis and treatment - Mayo Clinic. [online] Available at: https://www.mayoclinic.org/diseases-conditions/migraine-headache/diagnosis-treatment/drc-20360207
Millichap, J. G., & Yee, M. M. (2003). The diet factor in pediatric and adolescent migraine. Pediatric neurology, 28(1), 9-15.
Nall, R. (2017). What’s the Difference Between Migraines and Headaches? Retrieved January 21, 2018, from https://www.healthline.com/health/migraine/migraine-vs-headache
Pathophysiology of Migraine. (2018). Migraine.com. Retrieved 25 January 2018, from https://migraine.com/pro/pathophysiology-of-migraine
Pietrobon, D. (2005). Migraine: New Molecular Mechanisms. The Neuroscientist,11(4), 373-386. doi:10.1177/1073858405275554
Prince, P. B., Rapoport, A. M., Sheftell, F. D., Tepper, S. J., & Bigal, M. E. (2004). The effect of weather on headache. Headache: The Journal of Head and Face Pain, 44(6), 596-602.
Pietrobon, D. (2005). Migraine: New Molecular Mechanisms. The Neuroscientist,11(4), 373-386. doi:10.1177/1073858405275554
Prince, P. B., Rapoport, A. M., Sheftell, F. D., Tepper, S. J., & Bigal, M. E. (2004). The effect of weather on headache. Headache: The Journal of Head and Face Pain, 44(6), 596-602.
Ramage-Morin, P. L., & Gilmour, H. (2014). Prevalence of migraine in the Canadian household population.
Robbins, L. (1994). Precipitating factors in migraine: a retrospective review of 494 patients. Headache: The Journal of Head and Face Pain, 34(4), 214-216.
Ramsey, L. (2018). Here's how common pain relievers actually work in your body and brain.
Robbins, L. (1994). Precipitating factors in migraine: a retrospective review of 494 patients. Headache: The Journal of Head and Face Pain, 34(4), 214-216.
Russell, M. B., & Ducros, A. (2011). Sporadic and familial hemiplegic migraine: pathophysiological mechanisms, clinical characteristics, diagnosis, and management. The Lancet Neurology,10(5), 457-470. doi:10.1016/s1474-4422(11)70048-5
Sandler, M., Li, N. Y., Jarrett, N., & Glover, V. (1995). Dietary migraine: recent progress in the red (and white) wine story. Cephalalgia, 15(2), 101-103.
Sauro, K. M., & Becker, W. J. (2009). The stress and migraine interaction. Headache: The journal of head and face pain, 49(9), 1378-1386.
Stress Response. (2012). Migraine Relief Chiropractic Center. [online] Available at: http://migrainechiro.blogspot.ca/2012/04/stress-response-diagram.html
Spierings, E. L., Ranke, A. H., & Honkoop, P. C. (2001). Precipitating and aggravating factors of migraine versus tension‐type headache. Headache: The journal of head and face pain, 41(6), 554-558.
Wacogne, C., Lacoste, J. P., Guillibert, E., Hugues, F. C., & Le Jeunne, C. (2003). Stress, anxiety, depression and migraine. Cephalalgia, 23(6), 451-455.
Watson, K. D. (2011). The Molecular Mechanism of Migraine. 7-8. Retrieved from https://scholarsarchive.byu.edu/cgi/viewcontent.cgi?article=4047&context=etd.
Wöber, C., Holzhammer, J., Zeitlhofer, J., Wessely, P., & Wöber-Bingöl, Ç. (2006). Trigger factors of migraine and tension-type headache: experience and knowledge of the patients. The journal of headache and pain, 7(4), 188-195.