This is an old revision of the document!
Table of Contents
Causes of Sleep Deprivation
Alcohol/Drug Dependence
Research conducted by Irwin, Bjurstrom and Olmstead (2016) aimed to study the relationship between sleep and cocaine and alcohol use.8 In this study, the participants were individuals who has previously been dependent on these substances but were now in the early stages of abstinence.8 Polysomnographic sleep measures were recorded to determine sleep continuity, Stage 3 sleep and rapid eye movement (REM) sleep.8 In this study, sleep continuity included the total sleep time, sleep latency, which is the time required to transition from full wakefulness to sleep, sleep efficiency and wake sleep onset.8 Moreover, Stage 3 sleep was characterized by slow wave sleep (SWS), which consists of very slow delta waves in combination with smaller, faster waves in the brain.8 These measurements were then compared to the controls, which were patients that had no medical history of any mental illnesses or disorders.8 Although the results of the study indicated sleep continuity is not impacted by drug or alcohol use, the study did show that there was a decrease in Stage 3 sleep among both alcohol and cocaine-dependent patients.8 The results also indicate that loss of Stage 3 sleep occurs at an earlier age among the cocaine-dependent patients, in comparison to the alcohol-dependent patients.8 In addition, the amount of REM sleep increased among both groups of participants in comparison to the controls.8 Therefore, this study demonstrates that alcohol and cocaine have an impact on sleep disturbances.
Mental Disorders
Patients with schizophrenia often experience difficulty sleeping due to the fact that disturbances in sleep are characteristic of the first phase of a psychotic episode, known as the prodormal phase.9 More specifically, these patients either cannot fall asleep or cannot maintain sleep, waking up in at night or early in the morning.9 In addition, the severity of the illness is negatively correlated to the amount of rapid eye movement (REM) sleep patients with schizophrenia get.9 Therefore, depending on the severity of the disease, 30-80% of patients with schizophrenia suffer from sleep deprivation.9
Neurodegenerative Disease
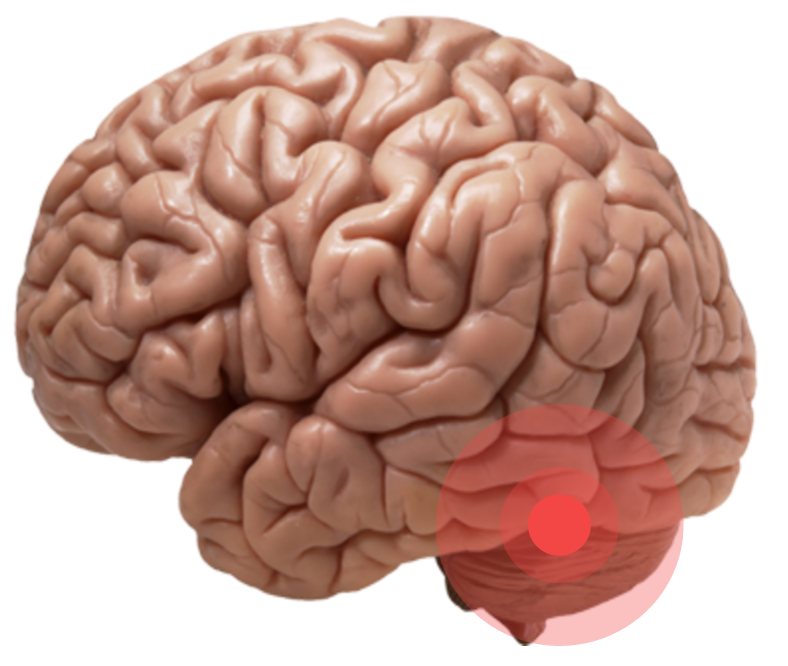
Parkinson’s Disease (PD) is the second most common neurodegenerative disease in the world.10 The pathology of PD affects all parts of the brain and recently, it has been noted that this neurodegenerative disease results in changes in sleep.10 Research conducted by Christensen et al. (2016) has demonstrated that REM sleep is less stable in patients with PD. 10 Since sleep is regulated by mechanisms that include neurons located in the basal brain regions, this research suggests that PD affects these mechanisms and, thus, leads to disturbances in sleep.10 Furthermore, the lower stability of REM sleep in patients with PD can also be attributed to the neurodegenerative nature of this disease.10 More specially, neurodegeneration affects the pre-thalamic fibres in the brain stem, which in turn may impact the neuronal mechanisms of REM sleep.10
Sleeping Disorders
Obstructive Sleep Apnea
Obstructive sleep apnea is a sleeping disorder which is characterized by a complete stop or reduction of air flow during sleep.11 This can be attributed to the complete or partial collapse of the airway.11 Obstructive sleep apnea can significantly decrease the amount and quality of sleep an individual gets due to loud snoring and interruptions in breathing patterns.11 In addition, individuals may awake from their sleep as a result of gasping or choking due to a lack of air.11 These obstructive respiratory events can occur five times during every hour of sleep and therefore, can lead to characteristics of sleep deprivation such as increased daytime sleepiness.11
Insomnia
Insomnia is another sleeping disorder which can cause sleep deprivation since individuals who experience insomnia have difficulties falling asleep or maintaining a state of being asleep.12 Importantly, insomnia leads to effects that are commonly associated with sleep deprivation, such as daytime sleepiness and an inability to focus.12 In addition, insomnia may also lead to an increased risk of worsening mental disorders, such as depression and anxiety.12 Moreover, there are two types of insomnia which can be associated with sleep deprivation. Primary insomnia is associated with difficulty, falling asleep, awakening during the night and difficulty falling back asleep after awakening.12 Secondary insomnia, however, is associated with comorbidities, such as heart disease or other sleeping disorders.12 Insomnia can, therefore, lead to sleep deprivation, decreasing one’s quality of life and functionality.12
References
8. Irwin, M. R., Bjurstrom, M. F., & Olmstead, R. (2016). Polysomnographic Measures of Sleep in Cocaine Dependence and Alcohol Dependence: Implications for Age‐Related Loss of Slow Wave, Stage 3 Sleep. Addiction.
9. Cohrs, S. (2008) Sleep disturbances in patients with schizophrenia: impact and effect of antipsychotics. CNS Drugs, 22, 939–962.
10. Christensen, J. A. E., Jennum, P., Koch, H., Frandsen, R., Zoetmulder, M., Arvastson, L., … & Sorensen, H. B. D. (2016). Sleep stability and transitions in patients with idiopathic REM sleep behavior disorder and patients with Parkinson’s disease. Clinical Neurophysiology, 127(1), 537-543.
11. Epstein, L. J., Kristo, D., Strollo Jr, P. J., Friedman, N., Malhotra, A., Patil, S. P., … & Weinstein, M. D. (2009). Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. Journal of Clinical Sleep Medicine, 5(3), 263-276.
12. Lee-Iannotti, J. K., & Parish, J. M. (2016). Suvorexant: a promising, novel treatment for insomnia. Neuropsychiatric Disease and Treatment, 12, 491–495.