This is an old revision of the document!
Table of Contents
Male Infertility
Presentation Slides
What is male infertility?
The inability to impregnate a fertile female due to abnormalities in the quantity and quality of sperm (Andrology Australia).
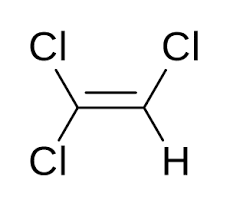
How is sperm normally produced?
The system of tubes in the testicles (seminiferous tubules) contain germ cells that are converted into sperm by hormones, including testosterone. During this process, the germ cells divide until they resemble tadpoles with a head and short tail.
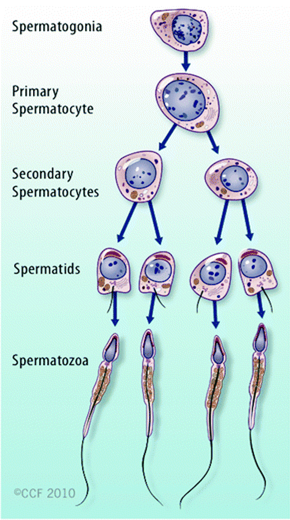
Figure 1. The Process of Spermatogenesis.
The tails push the sperm into a tube behind testes called epididymis. For around 5 weeks, the sperm travels through the epididymis to complete their development. The sperm then moves to the vas deferens. When a man is stimulated or sexual activity, the sperm mixes with seminal fluid (whitish liquid produced by seminal vesicle and prostate gland, to form semen. Due to stimulation, the semen which contains up to 500 million sperm is pushed out of the penis through the urethra (Frothingham, n.d.).
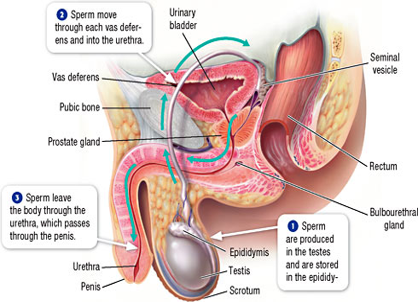
Figure 2. The Movement of Sperm in the Male Reproductive Tract.
Symptoms
The main indicator of male infertility is the inability to conceive a child. In some cases, underlying problem such as an inherited disorder, a hormonal imbalance, dilated veins around the testicle or a condition that blocks the passage of sperm causes signs and symptoms to surface. The symptoms include:
- Issues with sexual function — difficulty with ejaculation, reduced sexual desire, or erectile dysfunction, which are linked to testosterone levels
- Pain, swelling or a lump in the testicle area
- Recurrent respiratory infections
- Abnormal breast growth (gynecomastia)
- Decreased facial or body hair
- Small, firm testicles
- Lower than normal sperm count
(Mayo Clinic, n.d.).
Medical Causes
Sperm Disorders
Most problems associated with infertility are caused by sperm that:
- Do not fully grow
- Irregular shape
- Produced in low numbers
- Not produced at all
(Mayo Clinic, n.d.)
Varicoceles
Varicoceles is when the scrotum has swollen veins. The sperm is blocked from proper growth because the blood is not able to be drained. This may be due to the blood flowing backwards from your belly into your scrotum. Since the testicles are too warm at that point, the sperm cannot be produced and results in low sperm count. Varicoceles is found in 16% of the male population.
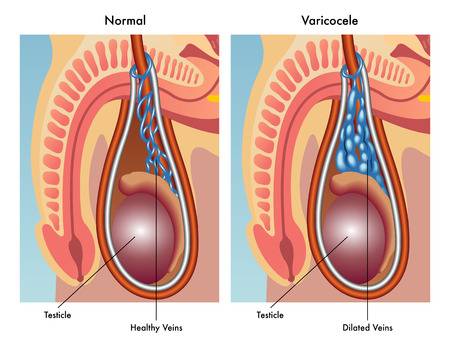
Figure 3. The difference between normal and dilated veins.
Retrograde Ejaculation
Retrograde ejaculation occurs when the nerves and muscles in your bladder don’t properly close during an orgasm. Instead of the semen coming out of the penis, it goes backwards into your bladder. Although the semen has normal sperm, it is not able to reach the vagina.
Immunologic Infertility
During an injury on infection, the body produces antibodies which can attack sperm. These attacks impair the sperm’s mobility and function. Although the mechanism of how this happens is unknown, it prevents sperm from moving to the fallopian tube and fertilizing the egg.
Obstruction
The sperm can be blocked from any part of the male reproductive tract. A blockage is usually caused by numerous infections, surgeries, inflammation and genetic defects. Due to these blockages, sperm can’t leave the testicles during an ejaculation.
Hormones
Hormones in the pituitary gland signal the testicles to make sperm. However, if the hormone levels are low, there is little to no sperm production.
Chromosomes
If there are alterations to a chromosome’s structure or number, it can have negative implications on a sperm. For example, if the Y chromosome from a male is missing parts of the structure.
Medication
Specific medications can alter sperm production, function and mobility. The medications are usually given to people to treat illnesses such as:
- Depression
- Digestive problems
- Infections
- High blood pressure
- Cancer
- Arthritis
(Mayo Clinic, n.d.), (Eunice Kennedy Shriver National Institute of Child Health and Human Development, 2017)
Environmental Causes
Industrial Chemicals and Heavy Metals
Low sperm counts can result from extended exposure to chemicals such as benzenes, toluene, pesticides, herbicides, organic solvents, painting materials and heavy metals such as lead (Mayo Clinic, n.d.). For example, male mechanics exposed to trichloroethylene (TCE), a chemical used as a degreasing agent, were found to have TCE and its by-products in their semen. A study conducted on mice found that TCE exposure led to reproductive tissue damage, suggesting that TCE is metabolized in the human reproductive tract and can adversely affect the normal development of sperm (Xu et al., 2004).
Radiation or X-rays
Sperm production may be reduced as a result of exposure to radiation. With low doses, sperm counts are able to eventually return back to normal. However, high doses of radiation may lead to permanent sperm production reduction (Mayo Clinic, n.d.).
Overheating the Testicles
Sperm production and function will be become impaired at elevated temperatures. Sitting, wearing tight clothing, and using a laptop for long periods of time may contribute to the increased temperature in the scrotum and thus have the ability to reduce sperm production (Mayo Clinic, n.d.)
Lifestyle Causes
Drug Use
Anabolic-androgenic steroids are one of the most common substances known to contribute to male infertility. They are also known as performance-enhancing drugs and are typically taken by athletes to increase muscle mass and strength. This type of drug can result in a shrinkage of testicles and a decrease in sperm production (Mayo Clinic, n.d.).
Alcohol Use
Alcohol has the ability to disturb the feedback mechanisms of the hypothalamus-pituitary-gonadal (HPG) axis. This can result in reduced or impaired production of hormones involved in sperm production such as luteinizing hormone (LH) and follicle-stimulating hormone (FSH). Alcohol consumption can also lower testosterone levels (Gude, 2012). All these factors contribute to decreased sperm production in addition to erectile dysfunction (Mayo Clinic, n.d.).
Smoking
It is suggested that the nicotine found in cigarette smoke contributes to significant decreases in sperm motility and sperm count. These effects can be reversed with cessation of smoking (Kovac et al., 2015). Secondhand smoking will contribute to male infertility as well (Mayo Clinic, n.d.).
Emotional/Psychological Stress
Severe or prolonged psychological stress such as depression, lack of self-esteem, stigma, grief, and isolation could reduce sperm count, libido, contribute to erectile dysfunction, and delayed or inhibited ejaculation (Basu, 2014). In addition, stress can interfere with certain hormones needed to produce sperm. Kirby et al. found that stress induced in rats led to hypothalamic suppression of reproductive function (2009).
Weight
Obesity can reduce fertility in males through hormonal and physical factors (Cabler et al., 2010).
Hormonal Factors: Obese men have high levels of white adipose tissue which exhibit high levels of aromatase activity. Aromatase is an enzyme that helps convert androgens, such as testosterone into estrogen. Therefore, the reduction of testosterone levels via aromatase activity can contribute to male infertility.
Physical Factors: Obese men are found to have increased scrotal fat, which may lead to increased testicular temperature.
Diagnosis
Male infertility is difficult to diagnose. Therefore, it may require numerous steps.
History and Physical Exam
The initial step towards a diagnosis is a history and physical exam. For the history portion, you would provide the healthcare provider with details surrounding issues of your reproductive system, hormone levels, illnesses, accidents and surgeries. The healthcare provider will also ask about your current health which includes medications and lifestyle choices such as drinking and tobacco use. The healthcare provider will also consider your exposure to heavy metals and your sexual health. The physical exam will examine issues in your penis, vas deferens, and testicles.
Semen Analysis
A semen analysis is usually conducted twice and is a lab test to determine male infertility. First, semen is collected by an individual masturbating into a specimen cup. The semen is studied for factors that will contribute to fertility or infertility. The factors that a healthcare provider will study are sperm volume, count, concentration, motility and structure. From these factors, a healthcare provider can determine the source of the issue. If the semen analysis shows a low sperm count, this may indicate issues with sperm growth and delivery.
Transrectal Ultrasound
The point of a transrectal ultrasound is to look at the structure of the reproductive system. I probe is placed in the recum. The ultrasound will provide insight into the structures of the ejaculatory duct or seminal vesicles.
Testicular Biopsy
This test is usually done in the case that the semen analysis indicates a low sperm count or no sperm at all. The biopsy involves a small cut to the scrotum where a small sample of tissue is taken from each testicle to be studied. The biopsy helps to determine the cause of infertility and collect sperm for assisted reproduction purposes.
Hormonal Profile
To rule out of major health concerns, a hormonal profile can be conducted. This purpose of this test is to determine how effective your testicles are at making sperm. This involves looking at hormones such as follicle-stimulating hormone.
Prevalence
The actual rates of male infertility are unknown and are shown based on self-report as well as rates calculated from current literature (Kumar & Singh, 2015). Global male infertility rates are different amongst races simply due to the fact that some developing countries underreport their male infertility. This is the case especially in African countries because if a man is unable to reproduce they are seen as inferior. It is believed that to compensate for this, polygamy is practiced in order to increase their likelihood of impregnating a woman (Agarwal et al., 2015). In North America its estimated that 4.5-6% of males are infertile; of all infertility cases, approximately 40-50% are due to male infertility (Kumar & Singh, 2015). This can be attributed to low sperm concentration, poor sperm motility or abnormal sperm or even a combination of these deficiencies (Agarwal et al., 2015).
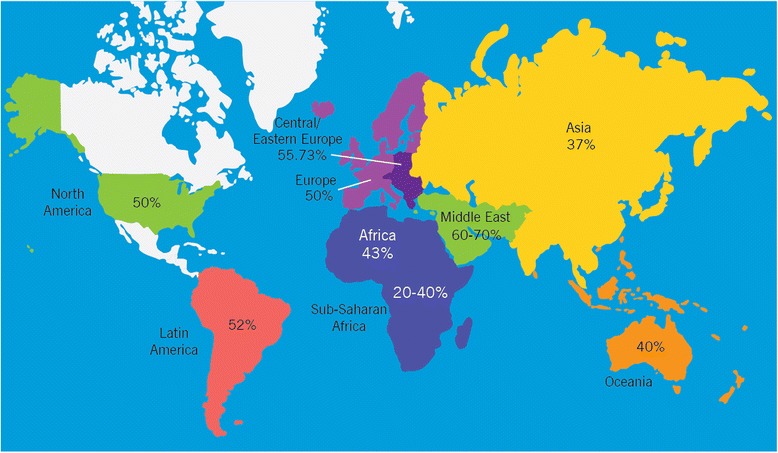
Figure 5. Out of the total infertility cases, estimated percentages due to males are reported.
Treatments
Surgical Therapy for Male Infertility
Varicocele Treatment
Varicocelectomy fixes swollen veins, which helps sperm movement, numbers, and structure (Urology Care Foundation, n.d.).
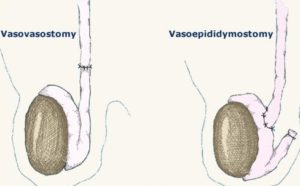
Microsurgical Vasovasostomy
A surgery to undo a vasectomy. This involves microsurgery to join the 2 cut parts of the vas deferens of each testicle (Urology Care Foundation, n.d.).
Vasoepididymostomy
This joins the upper end of the vas deferens to the epididymis. It's the most common microsurgical method to treat epididymal blocks (Urology Care Foundation, n.d.).
Transurethral Resection of the Ejaculatory Duct
Ejaculatory duct blockage can be treated surgically. A cystoscope is passed into the urethra and a small incision is made in the ejaculatory duct. This gets sperm into the semen in about 65 out of 100 men. But there can be problems. Blockages could come back. Incontinence and retrograde ejaculation from bladder damage are other possible but rare problems. Also, only 1 in 4 couples get pregnant naturally after this treatment (Urology Care Foundation, n.d.).
Treatment for Unknown Causes of Male Infertility
Because infertility problems are often due to hormones, empiric therapy might balance hormone levels. It's not easy to tell how well empiric treatments will work
Assisted Reproductive Techniques (ART):
Intrauterine Insemination (IUI)
For IUI, your health care provider places the sperm into the female partner's uterus through a tube. IUI is often good for low sperm count and movement problems, retrograde ejaculation, and other causes of infertility (Urology Care Foundation, n.d.).
In Vitro Fertilization (IVF)
IVF is when the egg of a female partner or donor is joined with sperm in a lab Petri dish. For IVF, the ovaries must be overstimulated. This is often done with drugs. It allows many mature eggs to be retrieved. After 3 to 5 days of growth, the fertilized egg (embryo) is put back into the uterus. IVF is used mostly for women with blocked fallopian tubes, but it's being used more and more in cases where the man has very severe and untreatable oligospermia (low sperm count) (Urology Care Foundation, n.d.).
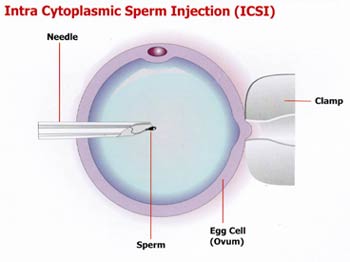
Intracytoplasmic Sperm Injection (ICSI)
ICSI is a variation of IVF. It has revolutionized treatment of severe male infertility. A single sperm is injected into the egg with a tiny needle. Once the egg is fertilized, it's put in the female partner's uterus. It is used if you have very poor semen quality, or if you have no sperm in the semen caused by a block or testicular failure that can't be fixed. Sperm may also be taken from the testicles or epididymis by surgery for this method (Urology Care Foundation, n.d.).
Sperm Retrieval for Assisted Reproductive Techniques
Testicular Sperm Extraction (TESE)
This is a common technique used to diagnose the cause of azoospermia. It also gets enough tissue for sperm extraction. The sperm taken from the testicle can be used fresh or frozen (“cryopreserved”). One or many small biopsies are done, often in the office (Urology Care Foundation, n.d.).
Testicular Fine Needle Aspiration (TFNA)
TFNA was first used to diagnose azoospermia. It is now sometimes used to collect sperm from the testicles. A needle and syringe puncture the scrotal skin to pull sperm from the testicle (Urology Care Foundation, n.d.).
Percutaneous Epididymal Sperm Aspiration (PESA)
PESA, like TFNA, can be done many times at low cost. There is no surgical cut. More urologists can do it because it doesn't call for a high-powered microscope. PESA is done under local or general anesthesia. The urologist sticks a needle attached to a syringe into the epididymis. Then he or she gently withdraws fluid. Sperm may not always be gotten this way. You may still need open surgery (Urology Care Foundation, n.d.).
Microsurgical Epididymal Sperm Aspiration (MESA)
With MESA, sperm are also retrieved from the epididymal tubes. This method uses a surgical microscope. MESA yields high amounts of motile sperm. They can be frozen and thawed later for IVF treatments. This method limits harm to the epididymis. It keeps blood out of the fluid. Even though MESA calls for general anesthesia and microsurgical skill, it has a lower problem rate. It's also able to collect larger numbers of sperm with better motility for banking (Urology Care Foundation, n.d.).
Management, Support and Resources
- American Urological Association (http://www.auafoundation.org)
- Society for the Study of Male Reproduction (www.ssmr.org)
- Resolve National Infertility Association (http://www.resolve.org)
- Men's Health Network (http://www.menshealthnetwork.org)
- American Pregnancy Association (http://americanpregnancy.org/infertility/male-infertility)
- Fertility Matters Canada (www.fertilitymatter.ca)
Myths
- A man's age doesn't affect his ability to father a child: The quality and quantity of a man's sperm begin to decline after age 40
- Wearing boxers is better than briefs: The theory is that wearing tight pants or briefs causes increasing temperature of the scrotum, therefore affecting sperm. There is no conclusive evidence of this
- Smoking doesn't affect male fertility: Cigarette smoking is associated with reduced sperm quality (lower total sperm count combined with increased abnormal morphology).
- Diet doesn't affect male fertility: Men that consume high-fat diets have been found to have a decreased sperm count
Case study
Jimmy Fallon and his wife tried to have a baby for 5 years to no avail. As a celebrity and a male one at that it was a very difficult time for him. He expressed in an interview that he tried to sleep upside down and drink certain teas, anything to help and they finally decided on a surrogate. What to learn from this case study: check your semen analysis, lifestyle adjustments can improve sperm quality, this may serve as an indicator for other health problems, no sperm doesn't mean you can’t have kids.

Figure 8. Jimmy Fallon on his show.
References
Agarwal, A., Mulgund, A., Hamada, A., & Chyatte, M. R. (2015). A unique view on male infertility around the globe. Reproductive biology and endocrinology : RB&E, 13, 37. doi:10.1186/s12958-015-0032-1
Andrology Australia. (n.d.). Male Infertility. Retrieved November 14, 2018, from https://andrologyaustralia.org/your-health/male-infertility/
Basu, S. C. (2014). Psychological Stress and Male Infertility. In Male Infertility (pp. 141-159). Springer, New York, NY.
Cabler, S., Agarwal, A., Flint, M., & Du Plessis, S. S. (2010). Obesity: modern man's fertility nemesis. Asian journal of andrology, 12(4), 480.
Eunice Kennedy Shriver National Institute of Child Health and Human Development. (2017). What are some possible causes of male infertility? Retrieved December 1, 2018, from http://www.nichd.nih.gov/health/topics/infertility/conditioninfo/causes/causes-male
Gude, D. (2012). Alcohol and fertility. Journal of human reproductive sciences, 5(2), 226.
Kirby, E. D., Geraghty, A. C., Ubuka, T., Bentley, G. E., & Kaufer, D. (2009). Stress increases putative gonadotropin inhibitory hormone and decreases luteinizing hormone in male rats. Proceedings of the National Academy of Sciences.
Kumar, N., & Singh, A. K. (2015). Trends of male factor infertility, an important cause of infertility: A review of literature. Journal of human reproductive sciences, 8(4), 191-6.
Kovac, J. R., Khanna, A., & Lipshultz, L. I. (2015). The effects of cigarette smoking on male fertility. Postgraduate medicine, 127(3), 338-341.
Mayo Clinic Staff. (n.d.). Male Infertility. Retrieved November 14, 2018, from https://www.mayoclinic.org/diseases-conditions/male-infertility/symptoms-causes/syc-20374773?p=1
Urology Care Foundation. (n.d.). How is male infertility treated. Retrieved November 14, 2018, from https://www.urologyhealth.org/urologic-conditions/male-infertility/treatment
Xu, H., Tanphaichitr, N., Forkert, P. G., Anupriwan, A., Weerachatyanukul, W., Vincent, R., … & Wade, M. G. (2004). Exposure to trichloroethylene and its metabolites causes impairment of sperm fertilizing ability in mice. Toxicological sciences, 82(2), 590-597.