This is an old revision of the document!
Table of Contents
Tuberculosis
Presentation Slides
What is tuberculosis?
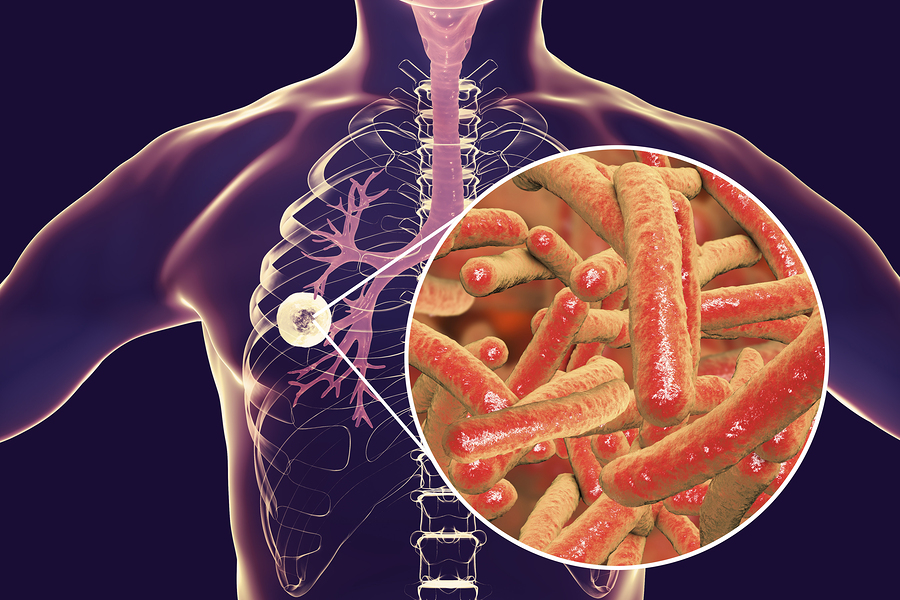
Tuberculosis (or TB) is a disease that is caused by the bacteria Myobacterium tuberculosis, which usually affects the lungs (World Health Organization, 2018). TB is a curable and preventable disease. It is spread through inhalation, so when someone with lung TB coughs or sneezes, they release the TB germs into the air where it can be inhaled by another person. Approximately 25% of the world's population has latent TB, meaning that they are infected by the bacteria but are not yet experiencing symptoms and cannot spread the disease. This is the reason why people who work in healthcare professions must be tested to see if they are carrying the bacteria. Of those infected with TB, there is a 5-15% risk of the disease becoming active. However, people with weakened immune systems, especially people with HIV, malnutrition or diabetes, are at a much higher risk of getting sick from it.
History of Tuberculosis
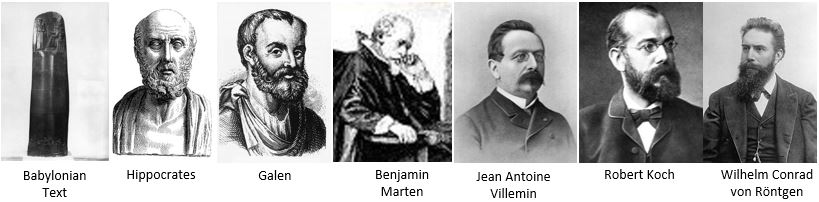
In 1948 BC, ancient text by the Babylonian monarch Hammurabi mentions a chronic lung disease that is likely TB (Herzog, 1998). Next, Famous Greek physician Hippocrates (460-370 BC), proposed the concept of pulmonary phthisis (tuberculosis) as a common disease that usually leads to death, however he believed that it was hereditary. Later, Galen (131-201) was the first person to suspect that phthisis was contagious, and warned against intimate contact with those who are sick.
In 1720, English physician Benjamin Marten proposed for the first time that the disease may be caused by small living creatures that entered the body, and proposed that the disease could perhaps be transmitted through contact by person to person (Herzog, 1998). In 1865, Jean Antoine Villemin single-handedly demonstrated that phthisis from humans and cattle could be transmitted to rabbits or guinea pigs. In 1882, Robert Koch produced irrefutable evidence that a specific microbe is the fundamental cause of tuberculosis. Equally as significant to this, in 1895, Wilhelm Conrad von Röntgen’s discovery of X-rays allowed for the accurate monitoring and studying of the development, course and severity of tuberculosis. Without Röntgen’s and Koch’s discoveries, the present day slow eradication of TB in developed countries wouldn’t be possible.
Signs and Symptoms
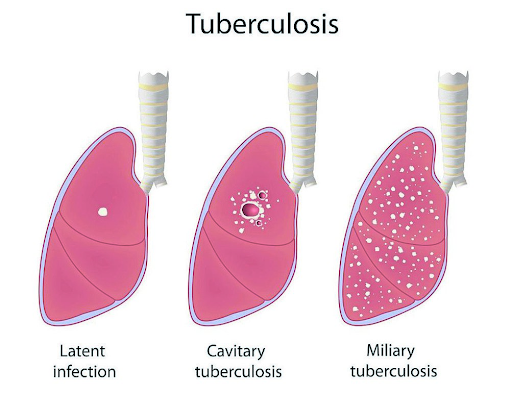
Latent TB
- While in this state, a person has the bacteria in their body but it is an inactive form which has no associated symptoms.
- This form of TB is also not contagious.
- Although this state is inactive, it can turn active if treatment is not provided.
- It is estimated that 2 billion people around the world have this form of TB.
- Usually tested with a TB skin test or blood test. Can be prevented.
Active TB
- This state of TB does show symptoms and is contagious.
- Bacteria is active and grows.
- It is possible for symptoms to show in the early weeks of infection or stay dormant and occur years later.
- Tested with sputum test and chest x-ray
- Can be treated
Signs and Symptoms
- Unintentional weight loss
- Fatigue
- Fever
- Night Sweats
- Chills
- Loss of appetite
- Coughing that lasts 3+ weeks
- Coughing up blood
- Chest pain or pain associated with breathing or coughing
People who have an increased risk of TB and should be screened for latent TB:
People living with HIV/AIDS IV drug users Those in contact or close proximity to infected individuals Health care works who treat people with a high chance of having TB
Diagnosis
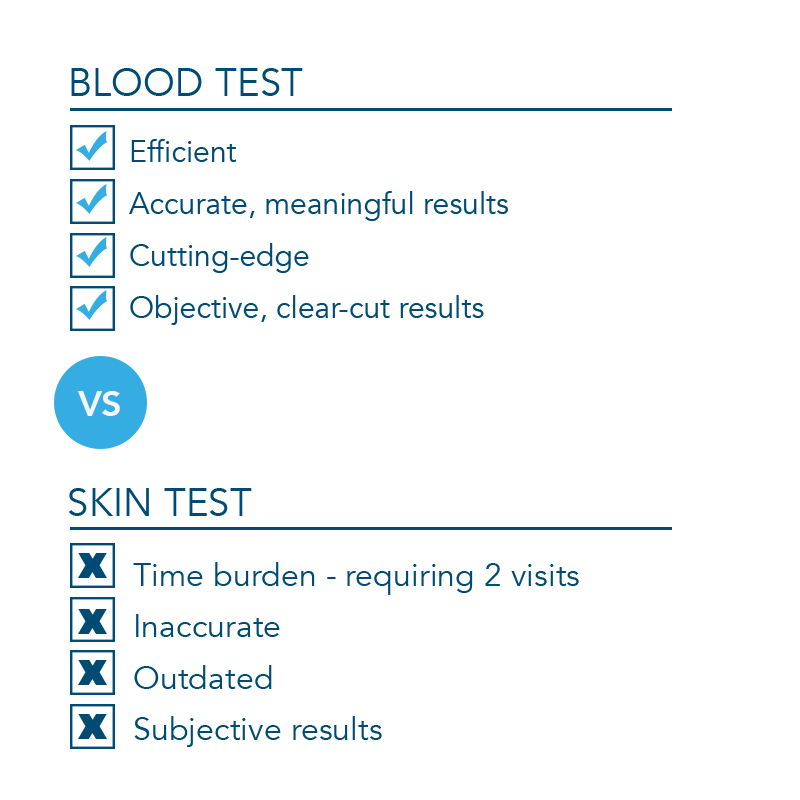
There are two types of diagnoses methods for TB which include the TB skin test and TB blood test. The conducting physician determines which test to use based on the reason behind the testing, availability of tests and the cost of administering the test. In most cases, both tests are not recommended to be administered.
TB Skin Test
This test requires two visits with a healthcare professional. During the first visit, the skin test is administered by injecting a small amount of tuberculin into the patient’s skin. This is usually done on the lower portion of their arm.
After a period of 48 to 72 hours, the patient returns to the clinic to have the healthcare professional determine if a reaction is present. The reaction is dependent on the size of the swelling.
A positive test concludes that the patient’s body was infected with the bacteria. More tests have to be conducted to determine if the patient has latent or active TB. If the test is negative, it usually indicates that latent TB or the TB disease is unlikely in this person.
If the test is repeated, it should be done on a different location on the body than the original test. This TB skin test is the recommended method for children below the ages of five years old.
TB Blood Test
This test is also referred to as the interferon-gamma release assays (IGRAs). The two TB blood tests that are approved are the QuantiFERON-TB Gold In-Tube test and the T-SPOT TB test.
A healthcare professional will draw a patient’s blood and the blood will be sent to a laboratory for analysis. A positive test would mean the person has the bacteria in their body. To determine if it is latent or active TB, additional tests are required. A negative test means the the individual’s blood had no reaction to the test. In this case, TB bacteria is unlikely in this individual.
The TB blood test is recommended for patients who have previously received the TB vaccine BCG or people who have a time constraint and are unable to return to the clinic for a second test for TST.
Limitations
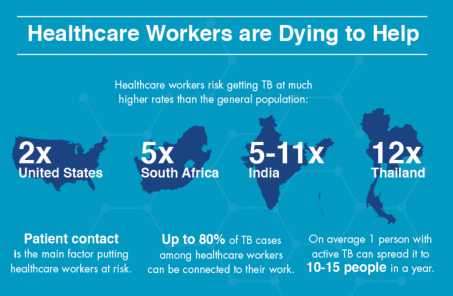
For individuals in the healthcare field, they must certify that they do not have active TB as this poses a risk to the patients they treat. To determine that you are not contagious, you must have two consecutive negative tuberculin skin tests (TST). If the first test is negative, employers will allow you to work under the condition that the second test must also be negative in one to three weeks.Healthcare workers should be tested for TB with a TST at least once a year thereafter. Workers who have more exposure to patients with TB may need to do it more often.
Since TB can be active at any point, prevention is key. Usually, a doctor will order a chest x-ray to determine if the bacteria is active or inactive. In the case that the chest x-rays come out negative, the physician would provide medications for 6-9 months to control the bacteria from becoming active in the future.
In the case that the chest x-rays come out positive, the physician will treat your TB as active TB. Treatment includes medications for 9-12 months. Due to the fact that you contagious, you will be unable to work until the physician deems your antibiotics as effective. The effectiveness of the antibiotics ranges but usually takes a few weeks.
For individuals who do not follow the entire treatment plan as prescribed by their doctor, they face the possibility of not fully recovering from the bacterial infection. This can also lead to drug-resistant TB where the medications prescribed to you are no longer effective at treating the condition.
Etiology
Causes
- Mainly caused by Myobacterium tuberculosis, which is a small aerobic bacteria
- Spreads when a person with active TB in their lungs coughs or sneezes, and it is inhaled by another person (not as contagious as the cold)
- Not always infectious. People with TB infection occurring outside the lungs do not spread the disease.
Risks
- Mostly adults are affected, however all age groups are at risk
- People living in developing countries are responsible for over 95% of TB cases and deaths
- People suffering from conditions that affect their immune systems are at greater risk of developing active TB, especially people with HIV (20 to 30 times more likely)
- In 2017, 1 million children (ages 0-14) were infected with TB and 230,000 died (World Health Organization, 2018)
- 7.9% of worldwide TB cases are attributed to smoking tobacco
- Prolonged close contact with someone whos infected
- Living in crowded conditions
- Very young or very old (weaker immune systems)
If you are healthy, you probably have a strong immune system and your body can fight off infections from TB bacteria or viruses easily. However, if you are run down or have another illness, your immune system might not be strong enough to fight the TB bacteria effectively. Stress, poor diet, certain medications, being pregnant or elderly can also weaken a person’s immune system.
Effect of HIV on TB
People living with HIV are much more likely than others to get ill with TB if they breathe in the bacteria. This is because HIV weakens their immune system, which makes it harder for the body to fight off infections. Having HIV also makes TB more difficult to diagnose and treat. Leaving a TB infection untreated speeds up the damage to a person’s health from HIV. If you are diagnosed with TB, you can ask for an HIV test. Knowing you are HIV positive and have TB is important for you and for the people treating you. You can be treated for both infections at once and getting rid of TB will help your HIV medication work better. If you are HIV positive you need to know the symptoms of TB. Also, ask for a TB test if you think you might have been in contact with someone with TB, even if you don’t have any symptoms.
Effect of drugs and alcohol on TB
Drinking, smoking, taking drugs and late nights can affect your immune system – so you can’t fight off infections as easily. Smoking tobacco, cannabis and other drugs, such as crack and heroin, can also give you a cough. As a result, you may think you just have a smoker’s or a drug-related cough but this could be TB in your lungs.
Mechanism
Tuberculosis (TB) is transmitted through air droplets and can be contracted through sneezing and coughing (Smith, 2003). Mycobacterium tuberculosis (M. tuberculosis) is the pathogen that attaches itself onto lung alveolar surfaces (Smith, 2003), the effect that the disease has on a host depends on how your immune system responds to the virus. There are three known stages of the disease, the initial stage can last 3-8 weeks, this is when the bacteria adheres to the surface of the alveoli and is then dispersed through the lymphatic system, no symptoms are presented here (Sasindran & Torrelles, 2011). The second stage typically lasts for 3 months, at this stage the bacteria gets circulated through the blood to other parts of the body. The third stage is defined by inflammation on the membrane of the lungs which can last 3-7 months and causes severe chest pain, additionally, this stage can be delayed for 2 years depending on immune response (Ahmad, 2011).
Once M. tuberculosis adheres to the alveoli, immune responses are activated. The impact of the disease depends on the strain of the disease and the host's immune system as previously stated. The disease can affect your body in two ways, it can be latent or active. In latent TB cases, the disease is contracted but inactive and no symptoms are present however, there is a chance that the pathogen may become activated, your chances of re-activation are higher if you get a disease that weakens your immune system (Ahmad, 2011). In active TB, the virus proliferates, spreads to other areas of the body and is contagious.
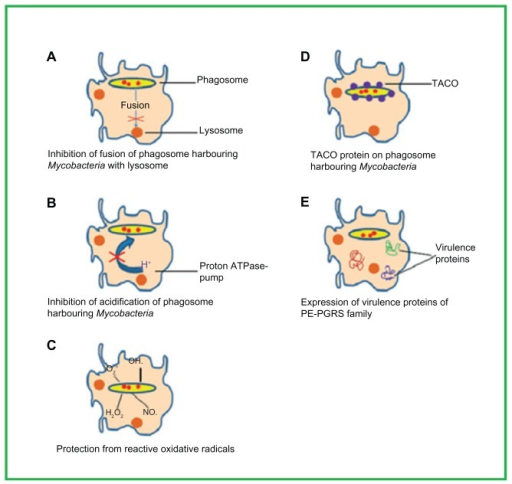
When M. tuberculosis is detected on alveolar surfaces macrophages phagocytose the bacterium and try to destroy it, in the case of active TB the virus is able to survive and proliferates in the cell and destroys it (Crevel et al., 2002). Once this happens, other immune cells such as monocytes, lymphocytes and neutrophils are called to try and ingest the virus and fail due to the survival mechanisms of the pathogen. This failed attempt to destroy the virus leads to inflammation and then causes the formation of granulomas which are a collection of macrophages that occur when an invader cannot be eliminated (Ferrari, 1999). The granulosa has a thick calcified core that prevents the virus from exiting the capsule. The important survival factors of M. tuberculosis include the inhibition of the fusion of the virus with the lysosome via tryptophan aspartate-containing coat (TACO) protein which surrounds the capsule containing M. tuberculosis. Normally, the protein is released before phagosome fusion with the lysosomes and the breakdown of the virus occurs this is the opposite with the presence of TACO on the phagosome (Ferrari, 1999). M. tuberculosis additionally thrives through inhibition of acidification, and the protection from reactive oxygen species. The virus continues to evade destruction and the granulosa then liquefies through unknown processes which enables the pathogen to continue to proliferate and mobilize to the lungs and other tissues through the lymphatic system which aids in the destruction of the lungs (Smith, 2003). At this stage symptoms such as coughing (lasting for more than 3 weeks), chest pain or pain with breathing or coughing, fever and chills are present.
Effects on Other Body Parts
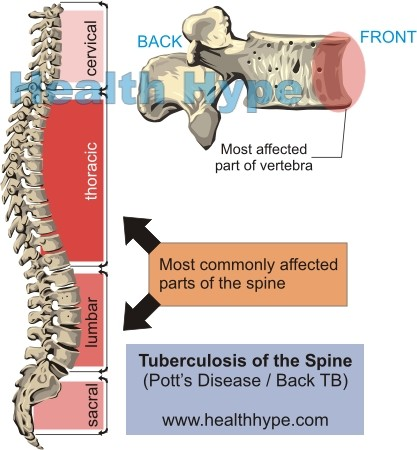
Although the lungs are the major site of damage caused by tuberculosis, many other organs and tissues in the body may be affected: The usual progression is for the disease to spread from the lungs to locations outside the lungs (extrapulmonary sites). In some cases, the first sign of disease appears outside the lungs. The many tissues or organs that tuberculosis may affect include:
- Bones: TB likely will attack the spine and the ends of the long bones. Children are especially prone to spinal tuberculosis. If not treated, the spinal segments (vertebrae) may collapse and cause paralysis in one or both legs.
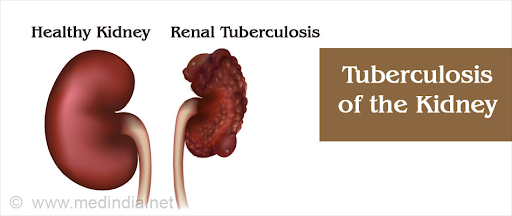
- Kidneys: Along with the bones, the kidneys are another common site of extrapulmonary TB. There may be few symptoms even though part of a kidney is destroyed. TB may spread to the bladder. In men, it may spread to the prostate gland and nearby structures.
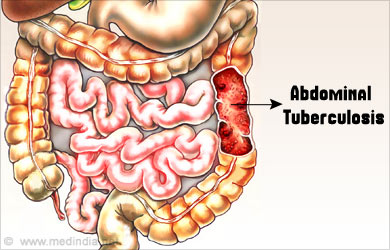
- Female reproductive organs: The ovaries in women may be infected; TB can spread from them to the peritoneum, which is the membrane lining the abdominal cavity.
- Abdominal cavity: Tuberculous peritonitis may cause pain ranging from the vague discomfort of stomach cramps to intense pain that may mimic the symptoms of appendicitis.
- Joints: Tubercular infection of joints causes a form of arthritis that most often affects the hips and knees. The wrist, hand, and elbow joints also may become painful and inflamed.
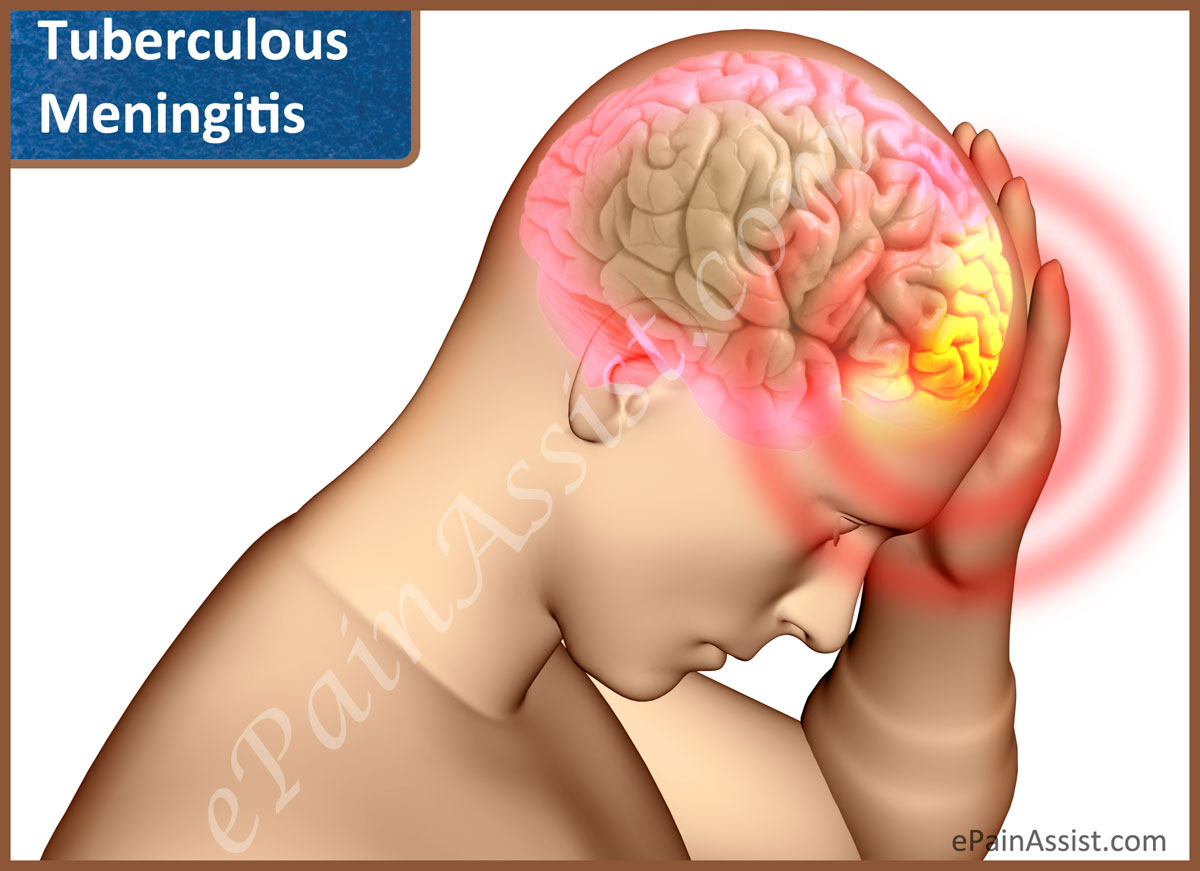
- Meninges: The meninges are tissues that cover the brain and the spinal cord. Infection of the meninges by the TB bacillus causes tuberculous meningitis, a condition that is most common in young children but is especially dangerous in the elderly. Patients develop headaches, become drowsy, and eventually comatose. Permanent brain damage is the rule unless prompt treatment is given. Some patients with tuberculous meningitis develop a tumor-like brain mass called a tuberculoma that can cause stroke-like symptoms.
- Skin, intestines, adrenal glands, and blood vessels: All these parts of the body can be infected by M. tuberculosis. Infection of the wall of the body's main artery (the aorta), can cause it to rupture with detrimental results. Tuberculous pericarditis occurs when the membrane surrounding the heart (the pericardium) is infected and fills up with fluid that interferes with the heart's ability to pump blood.

- Miliary tuberculosis: Miliary TB is a life-threatening condition that occurs when large numbers of tubercle bacilli spread throughout the body. Huge numbers of tiny tubercular lesions develop that cause marked weakness and weight loss, severe anemia, and gradual wasting of the body.
Prevention
Those without TB should avoid exposure to those with active TB, especially in closed or crowded spaces such as prisons and homeless shelters. Healthcare workers are advised to consult infection control and occupational health experts for preventative measures (Centers for Disease Control and Prevention, 2018).
Vaccinations are the primary preventative measure against TB, with the Bacilli Calmette-Guerin (BCG) vaccine being the only available vaccine as of 2011. BCG is a bacterial strain commonly found in cows (Andersen and Doherty, 2005). The vaccine is administered in children, with one dose given closer to birth, especially in areas known to have a high prevalence of TB (Fine, 2001). BCG is not usually administered in adults as its protective effects are variable. As the BCG vaccine does not provide complete protection against TB, booster shots are accessible in order to supplement the effectiveness of the original vaccine for those with a high risk of TB. However, booster does of BCG are not recommended by the World Health Organization (WHO) as immunity tends to decrease after about 10 years (World Health Organization, (n.d.). There are many explanations behind the inconsistent effectiveness of BCG. For one, the use of different strains of BCG can lead to variable results. Different strains of BCG due to differences in genetic and antigenic composition may have occurred in response to the growing demands for the vaccine (Andersen and Doherty, 2005). In addition, the effectiveness of the vaccine may be reduced if the patient has an additional parasitic infection (Rook et al., 2005). For this reason, children with HIV will not be able to be vaccinated with BCG (Fine, 2001).
Treatments
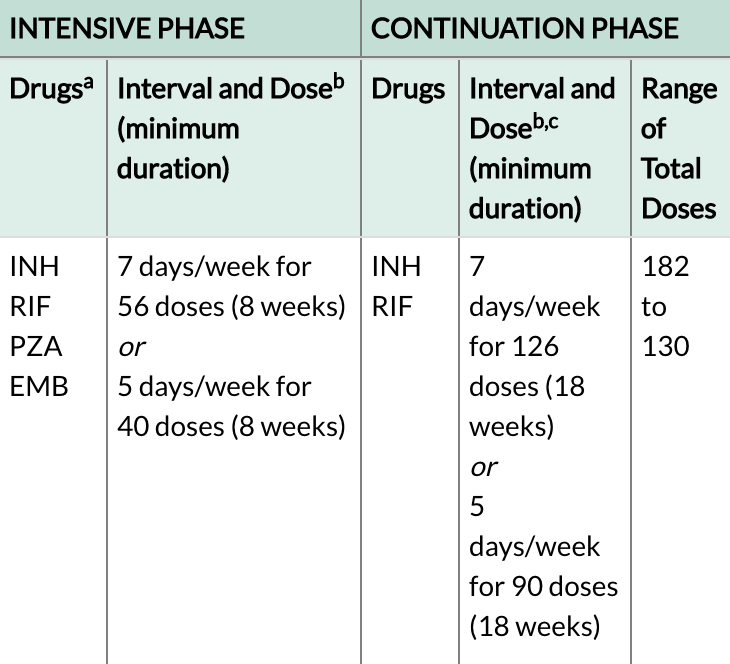
The exact course and length of treatment for TB depends on the patient’s age, overall health, form of TB, and location of TB in the body (Mayo Clinic, 2018). Doctors may suggest multi-drug regimens for patients as they are known to shorten the duration of treatment required to cure TB, and also expedite the response of the disease to treatment (Chan and Iseman, 2002). For latent TB, treatment duration is typically 6-9 months. To prevent the TB from becoming active, patients will take isoniazid pills either alone, or with rifampin (Mayo Clinic, 2018). For those with active TB, the course of treatment can last anywhere from 9-12 months. A combination of isoniazid, rifampin, ethambutol and pyrazinamide, known as the first line of anti-TB agents given to active TB patients (Mayo Clinic, 2018). An example regimen for a patient who is recently diagnosed with active TB would consist of a 2-month intensive phase, followed by a 4-7-month continuation phase as seen in the table below (Table 1) (Centers for Disease Control and Prevention, 2018).
If patients show resistance to any one of the first line anti-TB drugs, either isoniazid or rifampin, they may be diagnosed with drug resistant TB (DRTB). Those with suspected DRTB will have extended active TB regimens before a different course of treatment can be used (Chan and Iseman, 2002). Treatment for DRTB is used when there are no other alternatives, and will consist of 20-30 months of fluoroquinolones and injectable medications such as amikacin, kanamycin and capreomycin (Mayo Clinic, 2018). These drugs are known as second line anti-TB drugs. The FDA recommends that the DRTB course of treatment should not be used if patients have sinusitis, bronchitis, and UTIs in order to prevent extremely adverse side effects (Centers for Disease Control and Prevention, 2017).
A major issue with TB treatments is that patients are failing to abide by their treatment plan. Patients may need to take part in Direct Observed Therapy (DOT), where a nurse or surrogate will ensure that patients follow their treatment plan and take all their medications (Chan and Iseman, 2002). DOT is found to be effective in encouraging successful treatment.
Side Effects
TB medications can be highly toxic to the liver. Patients may experience nausea, loss of appetite, easy bruising, abdominal tenderness, jaundice, dark urine, blurred vision and high fever while being treated with TB medications (Mayo Clinic, 2018).
Geographic Prevalence
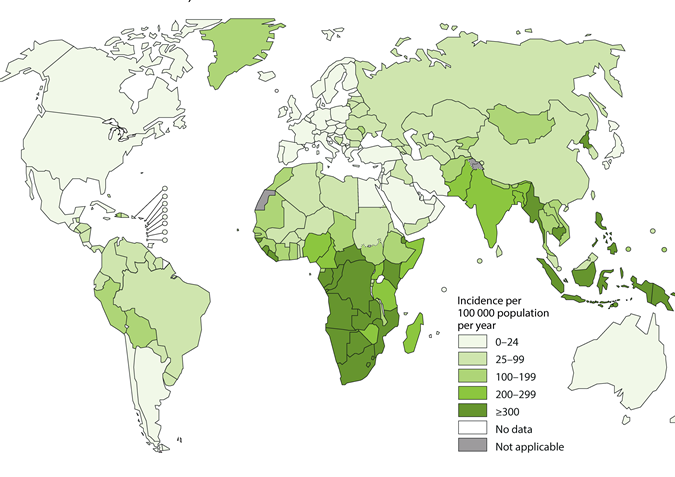
The world health organization defines TB as one of the top ten causes of death worldwide. All age groups are at risk of contracting the disease notably, individuals who are HIV positive are 20 to 30 times more likely to develop the active form of TB thus speeding the progression of both diseases. Approximately one quarter of the world's population has latent TB, these individuals have a 5-15% risk of developing active TB (WHO, 2018). The majority of cases and deaths are in developing countries although cases occur in every part of the world. India and China account for 40% of the total global TB cases. This is because TB is usually unrecognized till symptoms show additionally, the route of transmission via air particles is undetected. In spite of this, the global incidence of TB is decreasing by 2% each year (WHO, 2018).
Conclusion
In spite of this, the global incidence of TB is decreasing by 2% each year (WHO, 2018). Researchers are working on developing vaccinations to potentially replace BCG and its booster doses with one that provides complete immunity and is 100% effective in adults. The issue with developing vaccinations is that it is hard to imitate TB in non-human species. Researchers have suggested using zebrafish as a model species (Oksanen et al., 2013). Researchers are also looking into using aerosol vaccinations. In addition, researchers are working to create regimens that are shorter and require patients to take drugs less frequently. For example, patients would take medications once a week, for four months. Researchers are also looking to develop improved medications that are non-toxic and affordable TB treatments. Anti-TB drugs are costly, ranging from $18,000 to $513,000. (Centers for Disease Control and Prevention, 2017). Drugs such as bedaquiline and linezolid are examples of new anti-TB drugs (Mayo Clinic, 2018).
References
Ahmad, S. (2011). Pathogenesis, Immunology, and Diagnosis of Latent Mycobacterium tuberculosis Infection [Research article]. https://doi.org/10.1155/2011/814943
American Academy of Family Physicians (2006, January 1). Health Care Workers and Tuberculosis. Retrieved October 31, 2018, from https://familydoctor.org/health-care-workers-and-tuberculosis/
Andersen, P., & Doherty, T. M. (2005). The success and failure of BCG—implications for a novel tuberculosis vaccine. Nature Reviews Microbiology, 3(8), 656.
BC Centre for Disease Control (n.d.). About Tuberculosis. Retrieved October 31, 2018, from http://www.bccdc.ca/health-info/diseases-conditions/tuberculosis
Centers for Disease Control and Prevention. (2017, November 9). Drug-Resistant TB. Retrieved October 31, 2018, from https://www.cdc.gov/tb/topic/drtb/default.htm
Centers for Disease Control and Prevention (2018, October 24). Retrieved October 31, 2018, from https://www.cdc.gov/tb/topic/testing/tbtesttypes.htm
Centers for Disease Control and Prevention. (2018, August 17). Treatment for TB Disease. Retrieved October 31, 2018, from https://www.cdc.gov/tb/topic/treatment/tbdisease.htm
Chan, E. D., & Iseman, M. D. (2002). Current medical treatment for tuberculosis. BMJ (Clinical research ed.), 325(7375), 1282-6.
Ferrari, G., Langen, H., Naito, M., & Pieters, J. (1999). A Coat Protein on Phagosomes Involved in the Intracellular Survival of Mycobacteria. Cell, 97(4), 435–447. https://doi.org/10.1016/S0092-8674(00)80754-0
Fine, P. E. (2001). BCG: the challenge continues. Scandinavian journal of infectious diseases, 33(1), 58-60.
Herzog, B. H. (1998). History of tuberculosis. Respiration, 65(1), 5-15
Kompala, T., Shenoi, S. V., & Friedland, G. (2013). Transmission of Tuberculosis in Resource-Limited Settings. Current HIV/AIDS Reports, 10(3). https://doi.org/10.1007/s11904-013-0164-x
Mayo Clinic. (2018, January 4). Tuberculosis. Retrieved October 31, 2018, from https://www.mayoclinic.org/diseases-conditions/tuberculosis/diagnosis-treatment/drc-20351256
Mayo Clinic Staff. (2018, January 4). Tuberculosis - Symptoms and causes. Retrieved October 31, 2018, from https://www.mayoclinic.org/diseases-conditions/tuberculosis/symptoms-causes/syc-20351250
Oksanen, K. et al. “An adult zebrafish model for preclinical tuberculosis vaccine development.” Elsevier 31 (2013): 5202–5209. Print.
Rook, G. A., Dheda, K., & Zumla, A. (2005). Do successful tuberculosis vaccines need to be immunoregulatory rather than merely Th1-boosting?. Vaccine, 23(17-18), 2115-2120.
Sasindran, S. J., & Torrelles, J. B. (2011). Mycobacterium Tuberculosis Infection and Inflammation: what is Beneficial for the Host and for the Bacterium? Frontiers in Microbiology, 2. https://doi.org/10.3389/fmicb.2011.00002
Smith, I. (2003). Mycobacterium tuberculosis Pathogenesis and Molecular Determinants of Virulence. Clinical Microbiology Reviews, 16(3), 463–496. https://doi.org/10.1128/CMR.16.3.463-496.2003
Tuberculosis. (n.d.). Retrieved October 24, 2018, from http://www.who.int/news-room/fact-sheets/detail/tuberculosis
Tuberculosis (TB). (n.d.). Retrieved October 24, 2018, from https://www.healthlinkbc.ca/health-topics/hw207301
World Health Organization. (2018). Tuberculosis. Retrieved October 23, 2018, from http://www.who.int/en/news-room/fact-sheets/detail/tuberculosis
World Health Organization. (n.d.). Tuberculosis - Vaccines. Retrieved October 31, 2018, from http://www.who.int/ith/vaccines/tb/en/