Table of Contents
How Sleep Influences The Body
Presentation Slides
Introduction
Sleep is the most important thing that humans need. Going all the way back to the first lineage of human-like species, sleep would have created a state of vulnerability and thus those who slept would have been naturally selected against, but it was absolutely imperative for their bodies to repair and replenish themselves overnight. Sleep is a highly conserved behaviour across animal evolution, which demonstrates its importance for survival and fitness.
Sleep is characterized by altered consciousness, relatively inhibited sensory activity, reduced muscle activity, as well as the inhibition of nearly all voluntary muscles during deep sleep (John Hopkins Medicine, n.d.). There is a decreased overall reactivity to stimuli, but those who are asleep still show unique and active brain signals. During sleep, most of the body’s systems are in an anabolic state which helps to restore the immune, nervous, muscular, and skeletal systems; these are extremely vital processes that help to maintain a healthy mood, memory, and cognitive functions, and also plays are large role in ensuring proper functions of the endocrine and immune systems (John Hopkins Medicine, n.d.).
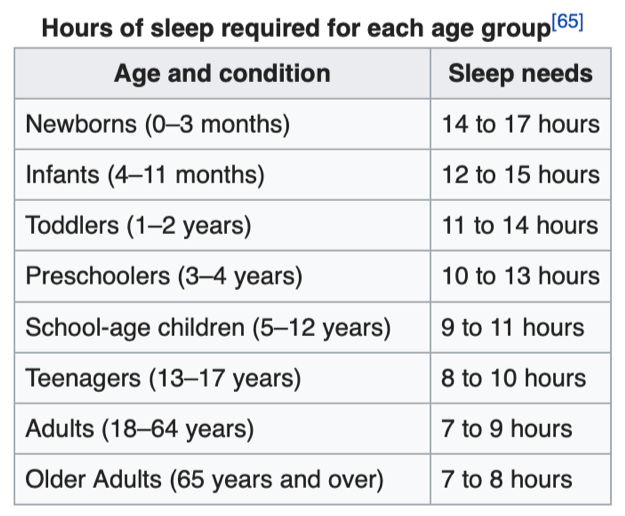
The internal circadian rhythm promotes daily sleep at night. This is our “internal clock” that recognizes the difference between day and night and ensures that our bodies are well rested at night in order to function properly throughout the day. The internal circadian rhythm is what causes individuals to become “jet-lagged” when they travel to different time-zones. Humans’ need for sleep varies depending on the individual; sleep is considered to be adequate when there is no daytime sleepiness or dysfunction (John Hopkins Medicine, n.d.). This would indicate that the body has fully replenished overnight and is able to function properly throughout the day. Age also plays a role in how much sleep individuals need on a given night. Younger children require more sleep in order to develop and function properly: up to 18 hours for newborns, with the rate decreasing as the child ages. The recommended amount of sleep for adults is between 7 to 9 hours per night (John Hopkins Medicine, n.d.).
Factors That Disturb Sleep
There are several factors that can disturb the balance of our circadian rhythm. One common factor is blue light exposure. Sources of blue light include the sun, digital screens, and LED light. Blue light suppresses the secretion of melatonin, a hormone that promotes sleepiness and shifts circadian rhythms (Harvard News Letter, 2018).
Inconsistent sleep schedules are another factor that disrupts sleep. The body is unable to establish a circadian clock, which leads to difficulty in falling asleep (Kang & Chen, 2009). Stress is also a factor that alters the sleep-wake cycle. Stress triggers the autonomic nervous system to release hormones, such as adrenaline and cortisol. These hormones are responsible for a reaction known as the flight-or-fight response, which raises one’s alertness and promotes arousal. Frequently being in a heightened state of alertness can delay the onset of sleep and adversely affect one’s sleep quality (Johnson, 2018).
Many would assume exercising before bed will also negatively impact sleep quality as it is another activity that stimulates cortisol release. However, scientists found that vigorous late-night exercise has no association with sleep and does not affect sleep quality (Myllymäki, et al., 2011). The effect of caffeine on sleep is another controversial discussion. Over the years, researches showed contradicting findings. One study suggested that consumption of caffeine 6 hours before bedtime has a significant disruptive effect on sleep. On the other hand, another study examined the relationship between caffeine, alcohol, nicotine, and sleep. Nicotine and alcohol use within 4 hours of bedtime was associated with increased sleep fragmentation, but caffeine was not associated with any of the sleep parameters (Spadola, et al., 2019). The effect of caffeine appears to vary among individuals.
Last but not least, eating near bedtime may also undermine sleep. While some food, such as warm milk and chicken breast, may help us relax and contain chemicals that promote sleep, spicy and acidic food like citrus and tomatoes can induce heartburn, which can lead to insomnia (Peters, 2019).
Consequences of Sleep Deprivation
Nervous System
Animal and human studies have shown that the quantity and quality of sleep play a critical role in learning and memory. Sleep helps learning and memory by allowing an individual to focus their attention maximally throughout the day, thereby allowing efficient learning to occur (Fowler, 1973). Sleep also has a profound effect on memory consolidation, which is the process in our brain used to convert short term memory to long term memory (Stickgold, 2005). It is recommended that students get at least 6 hours of sleep for tests and exams in order to retain and recall information. This also partially explains why all-nighters are not recommended to students. Memory consolidation takes place during sleep through the strengthening of the neural connections that form our memories (Stickgold, 2005). During sleep, the brain organizes information and classifies information depending on what we need and what we don’t need (Sleep, Learning, and Memory, 2020).
Sleep is critical for learning as it contributes to the three essential stages of learning: Acquisition, Consolidation, and Recall, in which each of these steps is necessary for proper memory function (Graves, 2001). Acquisition refers to the introduction of new information into the brain. Consolidation represents the processes by which a memory becomes stable. Recall refers to the ability to access the information after it has been stored. Although acquisition and recalling of information occur when an individual is awake, the consolidation, which links the acquisition stage (i.e. learning of new information) to recalling stage (being able to remember and apply the information), occurs when an individual is asleep (Graves, 2001). In other words, recalling of information cannot occur efficiently nor effectively without a proper memory consolidation. Thus, sleep plays a critical role in learning, memory, and concentration.
Endocrine System
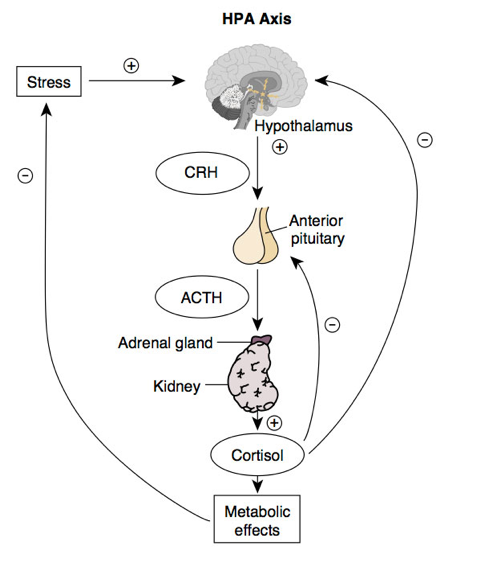
Getting a good quality of sleep is critical for the endocrine system to operate effectively. Significant hormonal changes affecting the hypothalamic-pituitary-adrenal (HPA) axis activity take place in the setting of sleep deprivation (Sleep and the Endocrine Brain, 2020). The HPA axis plays a critical role in the stress response, a neuroendocrine adaptation component that has been evolutionarily developed. The stress response initiates with the stimulatory release of corticotropin-releasing hormone (CRH) in the hypothalamus. The CRH binds to CRH receptors on the anterior pituitary gland, which stimulates the release of its hormone, or adrenocorticotropic hormone (ACTH). ACTH then binds to receptors on the adrenal cortex and stimulates the release of cortisol. In response to the stressors, cortisol will be released for several hours after encountering the stressor (Medscape, 2020).
Good quality of sleep maintains and regulates the HPA activity to a body’s optimum level, establishing homeostasis. However, activation of the HPA axis by a stressor is known to disrupt normal sleep patterns (Trayhurn, 2005). Hence, lack of sleep can heighten an individual’s sensitivity to stress.
Studies show that sleep loss is associated with an elevation of sympathovagal balance, activating and stimulating the sympathetic system (i.e. fight or flight) while deactivating the parasympathetic system (i.e. rest or digest). Studies demonstrate that the HPA axis that controls the release of the stress hormones (i.e. cortisol in primates and corticosterone in rodents) is reciprocally connected to sleep (Sam & Dhillo, 2010). Therefore, the lower the number of hours of sleep an individual gets, the higher the activation of the HPA axis accompanied by greater secretion of stress hormones, thereby increasing an individual's sensitivity to stress, fatigue, and pressure.
Immune System
Sleep and the circadian system exert a strong regulatory influence on immune functions (Besedovsky & Born, 2012). There is general consensus in the literature that adequate “restorative” sleep is needed to maintain good immunity. Immune parameters like leukocyte numbers, function, proliferation and cytokine production are altered by lack of sleep. Sleep deprivation is linked to increased daytime levels of inflammatory mediators such as interleukin-1 (IL-1), IL-6, and tumor necrosis factor (TNF) (AlDabal & BaHammam, 2011). Several other studies have addressed increased pro-inflammatory cytokine levels in response to sleep deprivation (AlDabal & BaHammam, 2011).
Young, healthy women who demonstrated disturbed sleep have shown signs of increased inflammatory markers along with specific chronic inflammatory diseases (AlDabal & BaHammam, 2011). Chronic sleep deprivation might be linked to increased all-cause morbidity and mortality (AlDabal & BaHammam, 2011). Studies show that if inflammation is present during waking, it can cause malaise, fatigue, immobility, pain and other aspects of sickness behaviour that are incompatible with the demands of mental and physical activity required for functioning effectively and carrying out daily functions (Besedovsky & Born, 2012).
Digestive System
Improper sleeping patterns can harm the activity of the digestive system. The body’s circadian rhythm is responsible for maintaining a regular sleep-wake schedule and is responsible for contributing to homeostasis (Rhoads, Levitsky, & Tavakkoli, 2016). The origin of the circadian rhythm is rather interesting. It exists as a result of evolutionary progression since survival is dependent on an individual’s ability to obtain food and sleep without being hunted (Rhoads, Levitsky, & Tavakkoli, 2016). It is, therefore, necessary to maintain a pattern of when to perform daily activities, and when it is time to sleep.
The circadian rhythm when disturbed can result in severe metabolic changes and an increased risk of developing diabetes and obesity (Rhoads, Levitsky, & Tavakkoli, 2016). This is because the physiological processes in the body follow the circadian rhythm and normally perform the same activities at the same time each day, and improper sleep patterns can, therefore, disrupt the mechanisms of metabolism. Individuals who receive less sleep than required tend to have lower levels of leptin, and higher levels of ghrelin which lead to an increased appetite, ultimately increasing body mass index (BMI) (Taheri et al., 2004). Improper sleep can also result in an increased prevalence of gastrointestinal tract diseases, particularly those involving the inflammation of the intestines (Manzar, Zannat, & Hussain, 2015). Some of these include an increased risk of developing mucous colitis and irritable bowel syndrome (Manzar, Zannat, & Hussain, 2015).
Reproductive System
The reproductive system can be affected by improper sleep, as with the other systems in the body. Fewer hours of sleep contributes to decreased levels of follicle-stimulating hormone (FSH), and increasing luteinizing hormone (LH) amplitude in women (Manzar, Zannat, & Hussain, 2015). FSH is responsible for stimulating the growth of follicles just as the name implies, and a decrease in its activity can result in a lack of maturation of follicles, and possibly implying a lower sex drive (or libido). The luteinizing hormone spikes can be harmful because it compromises the integrity by which the hormone acts on the body and this can result in the detrimental release of the hormone.
For pregnant women, sleep deprivation has been associated with an increase in levels of pro-inflammatory serum cytokines (Chang et al., 2010). This change can promote the incidence of postpartum depression (after giving birth), along with negative birth outcomes such as preterm delivery (Chang et al., 2010). Sleep deprivation for 4 to 7 days has been shown to result in significant decreases in testosterone levels (Choi et al., 2016). Studies have shown that decreased levels of testosterone have been linked with low libido (Travison et al., 2006). Sperm viability also significantly decreases with sleep deprivation (Alvarenga et al., 2015).
Cardiovascular System
The cardiovascular system can be impacted by sleep deprivation leading to complications such as an increased risk of cardiovascular disease (Manzar, Zannat, & Hussain, 2014). Sleeping less than 5 hours a day has been shown to increase the risk of developing hypertension (Gangwisch et al. 2006). Conditions such as sleep apnea and insulin resistance can also promote the incidence of developing cardiovascular disease and atherosclerosis (Manzar, Zannat, & Hussain, 2014). Improper sleep patterns have been associated with increased levels of insulin resistance (which has shown to increase the risk of developing cardiovascular disease), along with increased sympathetic activation and levels of cortisol (a stress hormone) (Bopparaju & Surani, 2010). The strongest contributors to cardiovascular disease are increased insulin resistance, CRP (C-reactive protein), and leptin levels (Bopparaju & Surani, 2010). Studies have shown that leptin plays a role in the etiology of insulin resistance, therefore increased levels of it would increase the risk of cardiovascular disease (Bopparaju & Surani, 2010). CRP has been shown to be a good biomarker for the development of cardiovascular disease when measuring its levels in blood tests (Karakas & Koenig, 2009).
Mechanisms of Sleep
Normal Sleep
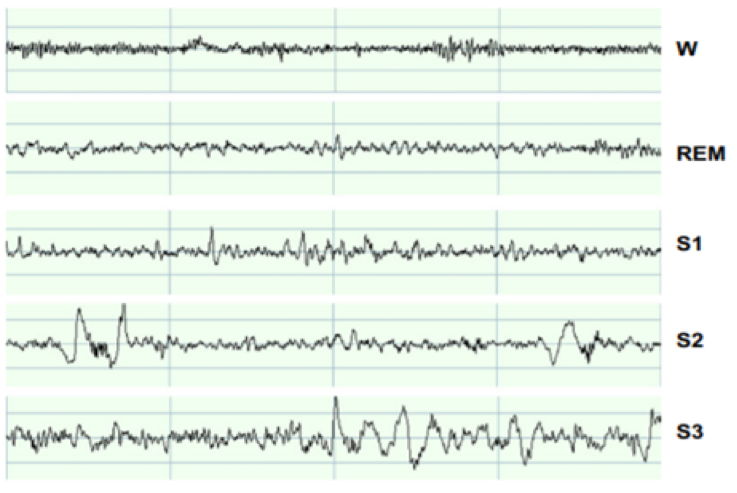
Sleep consists of two main phases, non‐rapid‐eye‐movement sleep (NREM) and rapid‐eye‐movement (REM) sleep. A measure of vigilance can be obtained by measuring brain electrical activity with electroencephalography (EEG). In EEG, waking is characterized by low‐amplitude, high‐frequency waves. During NREM sleep, the amplitude of EEG waves increases and the frequency decreases, while in REM sleep, EEG is indistinguishable from waking state. These states can be separated based on muscle activity (measured using electromyography, EMG) and saccadic eye movements (measured using electro‐oculography, EOG). During waking, muscle activity is high; in NREM sleep, it decreases; and in REM sleep, it practically disappears.
During REM sleep, eyes undergo characteristic rapid movements, of which the state has got its name. A finer division of NREM sleep is based on the proportion of the low‐frequency, high‐amplitude waves (called slow‐wave activity, SWA). NREM sleep is divided into three stages (S1, S2 and S3) in increasing order of SWA. Sleep stages alternate in the course of the night in a regular manner: sleep starts by S1 and deepens via S2 to S3 and then proceeds to REM sleep. After the REM sleep period, the cycle starts from the beginning. The duration of one sleep cycle is about 90 min. The sleep stages calculated across the night are often presented as a hypnogram, which describes the order and duration of each sleep stage. During SWA sleep, virtually all cortical neurons are engaged in a slow (<1 Hz) oscillation consisting of alternating ON and OFF periods. During ON periods, cortical cells are depolarized and fire action potentials at a high rate, while during OFF periods, cells are hyperpolarized and silent. (Porkka-Heiskanen et al., 2013)
Sleep Regulation
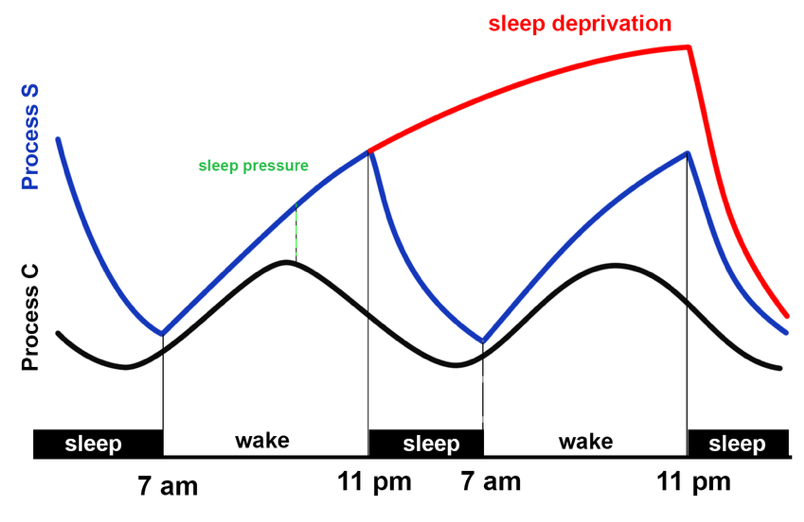
The two‐process model says that a homeostatic process (Process S) interacts with a process controlled by the circadian pacemaker (Process C), with time‐courses derived from physiological and behavioural variables. The model simulates successfully the timing and intensity of sleep in diverse experimental protocols. Electrophysiological recordings from the suprachiasmatic nuclei (SCN) suggest that Processes S and C interact continuously. A deficiency of Process S was proposed to account for both depressive sleep disturbances and the antidepressant effect of sleep deprivation (Borbely et al., 2016). The homeostatic process represents the need for sleep. It increases while awake and decreases while sleeping. The circadian rhythm depends on the suprachiasmatic nucleus. It is entrained in the external light-dark cycle, firing most rapidly during the light period, under the regulation of a special class of light‐sensitive retinal ganglion cells that contain the photopigment melanopsin. The C process would increase during the sleep state, thus ensuring continued sleep despite the diminishing homeostatic need for it toward the end of the sleep cycle (Saper et al., 2005).
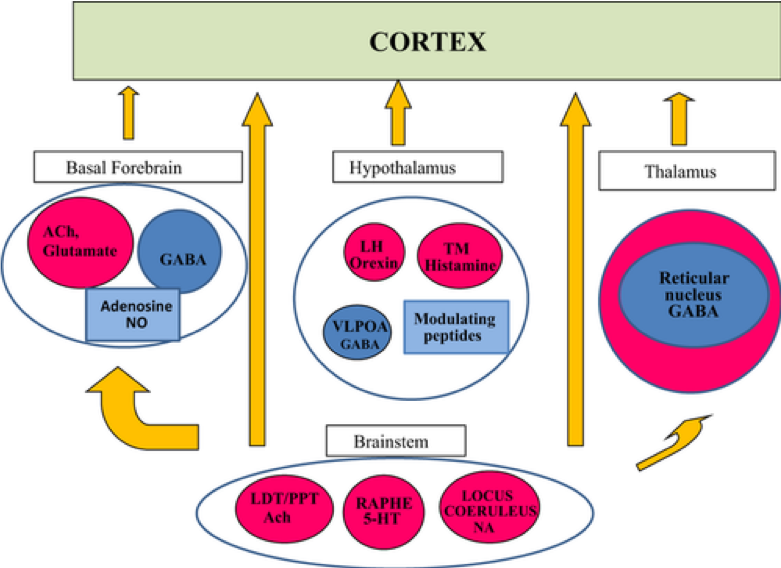
Sleep is regulated by the interaction of a variety of neurotransmitter systems in the brainstem, forebrain, and hypothalamus. A core region that is active during REM sleep is the subcoeruleus nucleus (SubC). It is hypothesized that glutamatergic SubC neurons regulate REM sleep and its defining features such as muscle paralysis and cortical activation. REM sleep paralysis is initiated when glutamatergic SubC cells activate neurons in the ventromedial medulla (VMM), which causes the release of GABA and glycine onto skeletal motoneurons. REM sleep timing is controlled by the activity of GABAergic neurons in the ventrolateral periaqueductal gray and dorsal paragigantocellular reticular nucleus as well as melanin-concentrating hormone neurons in the hypothalamus and cholinergic cells in the laterodorsal and pedunculo-pontine tegmentum in the brainstem (Fraigne et al., 2015).
Conclusion - How To Improve Sleep Quality
Maintaining good sleep hygiene is the key success in promoting a restful night’s sleep. Sleep hygiene refers to healthy sleep habits that can improve one’s sleep quality. There are four main sets of recommendations. First is to have a consistent sleep schedule. This helps the body to maintain a natural circadian rhythm and optimize the quality of sleep. Naps should be taken with caution. While some studies suggest that daytime naps benefit long term memory, other researches demonstrated that improper napping can disturb our circadian rhythm (Cousins, et al., 2019; Mayo Clinic. 2018).
The general consensus is that short naps (10 – 20 min) in the early afternoon produce the most benefit in terms of reduced sleepiness and improved cognitive performance (Sleep Foundation, n.d.). Any time longer or later may adversely affect the length and quality of nighttime sleep (Sleep Foundation, n.d.).
Second is to create an ideal sleep environment. The room should be quiet and dark, with a comfortable pillow and mattress. Because our body temperature naturally drops to prepare for sleep, keeping the room temperature between 60 and 67 Fahrenheit (15.5 to 19.4 Celsius) facilitates a better sleep environment and helps us fall asleep faster (Lauriello, 2019).
Third is to avoid consumption of stimulant substances before sleep. Caffeine, alcohol, and nicotine are all common chemicals that can interfere with sleep. On the other hand, several supplements, including melatonin and lavender, can induce relaxation and improve sleep quality (Mawer, 2018).
Last is to establish a soothing pre-sleep routine. Relaxing activities, such as hot showers and meditation, can clear our mind from the stresses we experience during the day (Mawer, 2018). Activities that can raise arousals, such as blue light exposure or late-night eating, should be avoided. By adhering to these four sets of recommendations, sleep quality can be improved tremendously.
References
AlDabal, L., & BaHammam, A. S. (2011). Metabolic, Endocrine, and Immune Consequences of Sleep Deprivation. The Open Respiratory Medicine Journal, 5, 31–43. https://doi.org/10.2174/1874306401105010031
Alvarenga, T. A., Hirotsu, C., Mazaro-Costa, R., Tufik, S., & Andersen, M. L. (2015). Impairment of male reproductive function after sleep deprivation. Fertility and sterility, 103(5), 1355-1362.
Besedovsky, L., Lange, T., & Born, J. (2012). Sleep and immune function. Pflugers Archiv, 463(1), 121–137. https://doi.org/10.1007/s00424-011-1044-0
Bopparaju, S., & Surani, S. (2010). Sleep and diabetes. International journal of endocrinology, 2010.
Borbély, A. A., Daan, S., Wirz‐Justice, A., & Deboer, T. (2016). The two‐process model of sleep regulation: a reappraisal. Journal of sleep research, 25(2), 131-143.
Chang, J. J., Pien, G. W., Duntley, S. P., & Macones, G. A. (2010). Sleep deprivation during pregnancy and maternal and fetal outcomes: is there a relationship?. Sleep medicine reviews, 14(2), 107-114.
Choi, J. H., Lee, S. H., Bae, J. H., Shim, J. S., Park, H. S., Kim, Y. S., & Shin, C. (2016). Effect of sleep deprivation on the male reproductive system in rats. Journal of Korean medical science, 31(10), 1624-1630.
Cohorte, L. (n.d.). Que Faire S’il Y A Des Problèmes De Concentration? Retrieved from https://www.sapaldia.net/sante/que-faire-sil-y-a-des-problemes-de-concentration/ Cousins, J. N., Wong, K. F., Raghunath, B. L., Look, C., & Chee, M. W. L. (2018). The long-term memory benefits of a daytime nap compared with cramming. Sleep, 42(1). doi: 10.1093/sleep/zsy207
Drake, C., Roehrs, T., Shambroom, J., & Roth, T. (2013). Caffeine Effects on Sleep Taken 0, 3, or 6 Hours before Going to Bed. Journal of Clinical Sleep Medicine, 09(11), 1195–1200. doi: 10.5664/jcsm.3170
Fowler, M. J., Sullivan, M. J., & Ekstrand, B. R. (1973). Sleep and Memory. Science, 179(4070), 302–304. https://doi.org/10.1126/science.179.4070.302
Fraigne, J. J., Torontali, Z. A., Snow, M. B., & Peever, J. H. (2015). REM sleep at its core–circuits, neurotransmitters, and pathophysiology. Frontiers in neurology, 6, 123.
Graves, L., Pack, A., & Abel, T. (2001). Sleep and memory: A molecular perspective. Trends in Neurosciences, 24(4), 237–243. https://doi.org/10.1016/S0166-2236(00)01744-6
Harvard Health Publishing. (n.d.). Blue light has a dark side. Retrieved from https://www.health.harvard.edu/staying-healthy/blue-light-has-a-dark-side
How Does Circadian Rhythm Impact Pilots? | Travel Blog. (2019, April 27). APR Travel Blog. https://www.airportparkingreservations.com/blog/circadian-rhythm-aviation/
How to get a great nap. (2018, November 20). Retrieved from https://www.mayoclinic.org/healthy-lifestyle/adult-health/in-depth/napping/art-20048319
John Hopkins Medicine. (n.d.). The Science of Sleep: Understanding What Happens When You Sleep. Retrieved from https://www.hopkinsmedicine.org/health/wellness-and-prevention/the-science-of-sleep-u nderstanding-what-happens-when-you-sleep
Johnson, J. (2018). Stress and sleep: What's the link? Retrieved from https://www.medicalnewstoday.com/articles/322994
Kang, J.-H., & Chen, S.-C. (2009). Effects of an irregular bedtime schedule on sleep quality, daytime sleepiness, and fatigue among university students in Taiwan. BMC Public Health, 9(1). doi: 10.1186/1471-2458-9-248
Karakas, M., & Koenig, W. (2009). CRP in cardiovascular disease. Herz, 34(8), 607-613.
Lauriello, S. (2019, July 9). This Is the Best Temperature for Sleeping, According to Experts. Retrieved from https://www.health.com/condition/sleep/best-temperature-for-sleeping
Manzar, M. D., Zannat, W., & Hussain, M. E. (2015). Sleep and physiological systems: a functional perspective. Biological rhythm research, 46(2), 195-206.
Mawer, R. (2018, November 2). 17 Proven Tips to Sleep Better at Night. Retrieved from https://www.healthline.com/nutrition/17-tips-to-sleep-better
Mong, J. A., Suchecki, D., Semba, K., & Parry, B. L. (2010). Sleep and the endocrine brain. International journal of endocrinology, 2010.
Myllymäki, T., Kyröläinen, H., Savolainen, K., Hokka, L., Jakonen, R., Juuti, T., … Rusko, H. (2011). Effects of vigorous late-night exercise on sleep quality and cardiac autonomic activity. Journal of Sleep Research, 20(1pt2), 146–153. doi: 10.1111/j.1365-2869.2010.00874.x
Paddock, C. (2018). How a key protein boosts memory, learning in the adult brain. Retrieved from https://www.medicalnewstoday.com/articles/323623
Peters, B. (2019). Timing of Last Meal May Contribute to Nighttime Heartburn or Insomnia. Retrieved from https://www.verywellhealth.com/eating-before-bed-3014981
Porkka‐Heiskanen, T., Zitting, K. M., & Wigren, H. K. (2013). Sleep, its regulation and possible mechanisms of sleep disturbances. Acta physiologica, 208(4), 311-328.
Rhoads, D. B., Levitsky, L. L., & Tavakkoli, A. (2016). Rhythms in the Digestive System. In Circadian Clocks: Role in Health and Disease (pp. 267-293). Springer, New York, NY.
Sam, A. H., & Dhillo, W. S. (2010). Endocrine links between fat and reproduction. The Obstetrician & Gynaecologist, 12(4), 231–236. https://doi.org/10.1576/toag.12.4.231.27614
Saper, C. B., Cano, G., & Scammell, T. E. (2005). Homeostatic, circadian, and emotional regulation of sleep. Journal of Comparative Neurology, 493(1), 92-98.
Sleep, Learning, and Memory | Healthy Sleep. (n.d.). Retrieved February 13, 2020, from http://healthysleep.med.harvard.edu/healthy/matters/benefits-of-sleep/learning-memory
Sleep Foundation. (n.d.). Napping Benefits & Tips. Retrieved from https://www.sleepfoundation.org/articles/napping
Spadola, C. E., Guo, N., Johnson, D. A., Sofer, T., Bertisch, S. M., Jackson, C. L., … Redline, S. (2019). Evening intake of alcohol, caffeine, and nicotine: night-to-night associations with sleep duration and continuity among African Americans in the Jackson Heart Sleep Study. Sleep, 42(11). doi: 10.1093/sleep/zsz136
Stickgold, R. (2005). Sleep-dependent memory consolidation. Nature, 437(7063), 1272–1278. https://doi.org/10.1038/nature04286
Taheri, S., Lin, L., Austin, D., Young, T., & Mignot, E. (2004). Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS medicine, 1(3).
The Impact of Sleep Deprivation on Hormones and Metabolism. (n.d.). Medscape. Retrieved February 24, 2020, from http://www.medscape.org/viewarticle/502825
Travison, T. G., Morley, J. E., Araujo, A. B., O’Donnell, A. B., & McKinlay, J. B. (2006). The relationship between libido and testosterone levels in aging men. The Journal of Clinical Endocrinology & Metabolism, 91(7), 2509-2513.
Trayhurn, P. (2005). Endocrine and signalling role of adipose tissue: New perspectives on fat. Acta Physiologica Scandinavica, 184(4), 285–293. https://doi.org/10.1111/j.1365-201X.2005.01468.x