Table of Contents
Presentation Slides
Cancer: Rare and Recent
What is cancer?
Cancer is the generic term that is used to describe a large group of diseases that can affect any part of the body (“Cancer”, 2018). A defining feature of cancer is the rapid production of abnormal cells that grow beyond their normal boundaries (“Cancer”, 2018). While a normal cell would mature into specialized cells with specific functions, cancer cells do not; they are less specialized than normal cells (Nall, 2020). One reason cancer cells can divide without stopping is due to its ability to ignore signals that indicate they should stop dividing or begin a process known as programmed cell death - apoptosis, to get rid of unneeded cells (Nall, 2020). Under normal circumstances, human cells grow and proliferate new cells as the body needs them; when the cells grow old or become damaged, they die and new cells take their place. However, in cancerous cells, the process is broken down and cells become increasingly abnormal as old or damaged cells survive when they should have gone through apoptosis (Nall, 2020). In addition, new cells continue to form when they are not needed. These extra cells will continue to divide without stopping, which may become tumors.
All types of cancer have the ability to induce the body’s cells to keep dividing without stopping and to spread into surrounding tissues/organs (“What is Cancer?”, 2015); the latter process is known as metastasizing (“Cancer”, 2018). In this process, some cancer cells may break off and travel to other parts in the body through the systemic or the lymphatic system, forming new tumors that are far from its original source (“What Is Cancer?”, 2015). This is the major cause of death from cancer (“Cancer”, 2018).
In comparison, benign tumors are tumors that do not spread into or invade the nearby tissues. Although these can sometimes be larger in size, if they are removed, they usually do not grow back. Benign tumors are usually not life-threatening, however, if the benign tumor is found in the brain, it will become life-threatening.
Causes of Cancer
Cancer is a genetic disease that is caused by the changes to genes that control the way our cells function, specifically, how they divide and grow. Cancer can be inherited by parents, arise as a result of errors that occur as cells divide, or due to damage to the DNA caused by certain environmental exposures. (Nall, 2020). Some examples include the chemicals in tobacco smoke, radiation from the sun, heavy alcohol consumption, excess body weight, physical inactivity, and poor nutrition, amongst other variables. Currently, the most significant unpreventable risk factor is age. According to the American Cancer Society, 87% of cancer cases are found in people aged 50 or older (Nall, 2020).
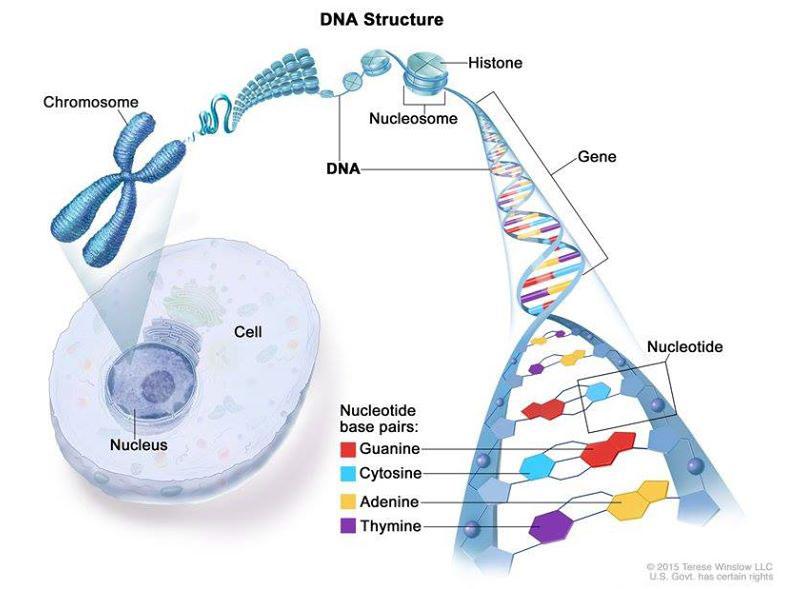
Figure 1: Cancer is caused by certain changes to genes, the basic physical units of inheritance. Genes are arranged in long strands of tightly packed DNA called chromosomes. (Winslow, 2015)
There are three main types of genes that contribute to the genetic changes of cancer: proto-oncogenes, tumor suppressor genes, and DNA repair genes (“What Is Cancer?”, 2015). These are sometimes known as the “drivers” of cancer. Proto-oncogenes play an important role in normal cell growth and division (“What Is Cancer?”, 2015). However, when these genes become more active than normal, they can become cancer-causing genes, known as oncogenes. They then allow cells to grow and survive when they should not (“What Is Cancer?”, 2015). Tumor suppressor genes are also involved in controlling cell growth and division (“What Is Cancer?”, 2015). When alterations occur within these genes of a cell, they start dividing in an uncontrolled manner (“What Is Cancer?”, 2015). DNA repair genes are involved in fixing damaged DNA, but cells with mutations in these genes become prone to developing mutations in other genes (“What Is Cancer?”, 2015). Together, these mutations may cause some cells to become cancerous (“What Is Cancer?”, 2015).
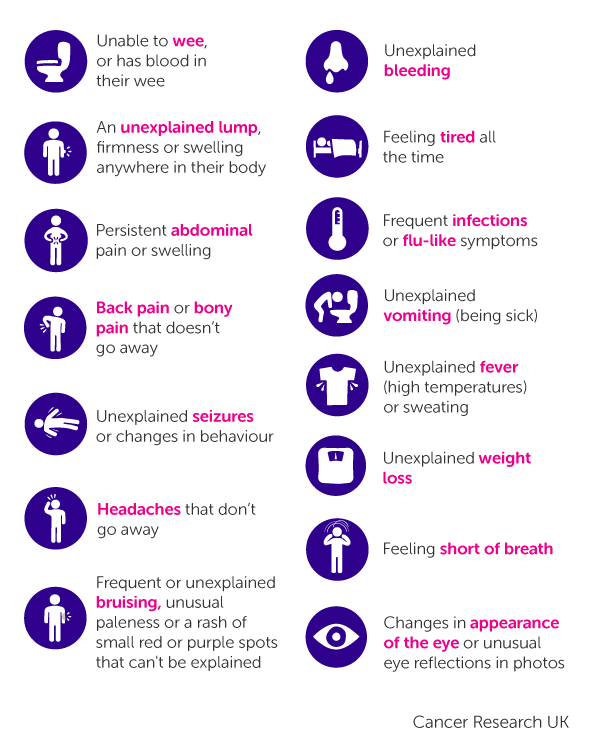 Figure 2: General symptoms of Cancer External Link
Figure 2: General symptoms of Cancer External Link
General/Common symptoms of cancer
The signs and symptoms that are a result of cancer can vary depending on which part of the body is affected. General signs and symptoms that are associated with cancer, but not specific to cancer, include:
- Fatigue
- Lump or area of thickening that can be felt under the skin
- Weight changes, including unintended loss or gain
- Skin changes (e.g. yellowing, darkening or redness of the skin), sores that won’t heal, or changes to existing moles
- Changes in bowel or bladder habits
- Persistent cough or trouble breathing
- Difficulty swallowing
- Hoarseness
- Unexplained bleeding or bruising (“Cancer”, 2018)
Rare Cancer: Von-Hipple Lindau Disease (VHL)
The VHL syndrome is a hereditary condition, specifically an autosomal dominant genetic condition (Varshney et al., 2017). This suggests that the risk of developing and acquiring this disease is passed on from generation to generation within a family (Varshney et al., 2017). Even though the disease is genetic, there have been many patients who have no family history of the condition (Maher et al., 1995). Infact, about 20% of people with VHL do not have any family history of the condition (Maher et al., 1995). The cause of this is the mutation, or the alteration, of the VHL gene which can give the person an increased chance of developing different types of cancer and a range of symptoms that are discussed below (Mukhopadhyay et al., 2002).
VHL is a very rare type of cancer (Vortmeyer & Alomari, 2015). To illustrate, it only affects 1 in 36,000 people worldwide (Vortmeyer & Alomari, 2015). Individuals with this disease can experience the formation of tumors in up to 10 parts of the body, usually in the brain, spine, kidneys and eyes (Mukhopadhyay et al., 2002). The tumors that are formed in the eye particularly are known as angiomas (Poulsen et al., 2010). One thing to note about this disease is that most of the tumors are benign (however some can be malignant) but they can still cause some serious physiological damage (Poulsen et al., 2010). The process initiates when these tumors start to grow in size, putting pressure on surrounding organs and eventually leading to internal bleeding within patients and ultimately organ failure (Varshney et al., 2017).
Patients diagnosed with this disease also have an increased risk of developing cancers like clear cell renal cell carcinoma, also known as kidney cancer (Bader & Hsu, 2012). This condition is very common between VHL patients as the risk of development of kidney cancer in families with VHL is estimated to be about 40% (Poulsen et al., 2010).
VHL Symptoms
One of the most common symptoms of VHL is hemangioblastomas, which are basically these benign tumors developing mostly in the spine and brain (Lonser et al., 2004). These tumors might be encapsulated with a fluid filled sac within them which can further form cysts within the organ they are located in (Lonser et al., 2004). These cysts then press upon nearby nerves or brain tissue eventually leading to secondary symptoms such as headaches, migraine, trouble balancing, and muscle weakness (Sakaguchi, 2012). Hemangioblastomas occurring near or in the eye can result in fluid leakage which poses serious implications on one’s vision and ability to move the pupil (Bader & Hsu, 2012). Early detection of the formation of tumors is key to maintaining healthy vision in case of tumors occurring near or in the eye (Bader & Hsu, 2012). Moreover, these tumors can also occur in the kidneys but they usually metastasize or are removed and reportedly are not associated with any type of symptoms (Mukhopadhyay et al., 2002). VHL can also cause a tumor to form in the inner ear which is referred to as an endolymphatic sac (Vortmeyer & Alomari, 2015). The formation of this tumor can lead to problems in balance when walking as well as issues with the tympanic membrane causing hearing loss (Vortmeyer & Alomari, 2015). Tumors in the livers and lungs can occur but are not considered problematic (Maher et al., 1995).
VHL syndrome is also linked with a type of tumor called a pheochromocytoma, which most commonly occurs in the adrenal glands (Sakaguchi, 2012). However, it is important to note that scientists have not found these tumors to be cancerous (Poulsen et al., 2010). These tumors do not cause any symptoms but some studies reported patients having increased blood pressure as a result (Poulsen et al., 2010). In more rare cases, pancreatic tumors, and cystadenomas of the epididymis or broad ligament can occur (Mukhopadhyay et al., 2002).
Causes of VHL
Mutations in the VHL gene cause Von Hippel-Lindau syndrome (Von Hippel-Lindau syndrome, 2020). The VHL gene is a tumor suppressor gene. Tumor suppressor genes slow down cell division. In other words, these genes keep the cells from dividing in an uncontrollable manner (Von Hippel-Lindau disease, n.d.). However, mutation in this gene can lead to an abnormal VHL protein. It can also prevent the production of VHL protein (Von Hippel-Lindau syndrome, 2020). This means cell division cannot be regulated. Therefore, cells grow and divide rapidly to form cysts (fluid-filled sacs) and tumors (Von Hippel-Lindau syndrome, 2020).
Mutations in the VHL gene are inherited in an autosomal dominant manner (Von Hippel-Lindau syndrome, 2020). This means that having one copy of the mutated VHL gene is enough to increase an individual's chance of developing the VHL syndrome (Von Hippel-Lindau syndrome, 2020). With most autosomal dominant inheritance cases, having one copy of mutated gene is enough for an individual to develop the disease but with VHL syndrome, an individual needs to have two copies of the mutated gene for the disease to develop (Von Hippel-Lindau disease, n.d.). Most people who are born with a copy of mutated VHL gene will eventually acquire a mutation in the second copy of the gene and as a result, will develop VHL disease (Von Hippel-Lindau syndrome, 2020). In addition, most individuals inherit the mutated VHL gene from their affected parents but in approximately 20% of cases, mutations occur in people with no family history. This is known as de novo mutation (Von Hippel-Lindau disease, n.d.). Lastly, children of individuals who have a mutated VHL gene have a 50% chance of inheriting that mutation (Von Hippel-Lindau disease, n.d.).
VHL Diagnosis
As mentioned, VHL affects multiple organs, thus different imaging tools can be utilized to identify characteristic VHL lesions in the regions most commonly affected by VHL. These regions include the eye, central nervous system and the endocrine system. Magnetic Resonance Imaging of the brain and spine, ultrasound for abdomen, and blood and urinary levels of adrenal gland hormones are often utilized to provide a provisional diagnosis (Genetic and Rare Disease Information Center (GARD), 2016).
Since VHL is a genetic disorder, genetic screening is the best tool to identify a mutation in the VHL gene, and thus to provide a definite diagnosis for an individual with the disease. Genetic screening is advised in the case of an individual with blood relatives suffering from VHL; individuals exhibiting VHL-like lesions along with a family history of the disease, and individuals exhibiting multiple VHL-like lesions. In the last case, a family history is not necessary since 20% of VHL mutations are de novo (GARD, 2016).
VHL Treatment
Preventative measures can be taken to avoid long-term damage that could be caused by benign or malignant VHL associated lesions. Individuals receiving an early diagnosis of the disease are referred for frequent screening to detect the formation of lesions in their early stages. Once the lesion is detected and identified, treatment varies depending on the type of lesion, organ affected, imaging test reports and the general overall physical condition of the individual (National Organization of Rare Diseases (NORD), n.d.).
Benign lesions are usually not capable of invading surrounding areas, however they can grow in size and may cause damage to surrounding structures. Malignant tumors show accelerated growth and are capable of metastasis, hence early detection is necessary to prevent the spread and damage (NORD, n.d.). In cases where damage is observed due to the size of the lesion or its malignancy, a suitable surgical method is utilized to remove the lesion depending on its location (NORD, n.d.). Surgical method could involve removing the organ partially or entirely depending on the lesion. Malignant tumors less than 3cm in size in the kidneys are often removed via kidney sparing technique as it allows for the preservation of kidney function (Partial Nephrectomy, n.d). Additionally, small tumors associated with kidneys can also be treated using radio frequency ablation technique. This technique involves using one of the many imaging tools available (Ultrasounds, MRI or CT) to locate the tumor, and then through the insertion of a needle, high frequency electrical currents are passed into the tumor. This causes the tumor to heat up eventually leading to its death (Hwang et al., 2004).
Varying surgical procedures are utilized depending on the type of lesion and the organ affected. Radiation is also sometimes used; however, it is generally avoided to prevent radiative damage (NORD, n.d.). Sometimes, a benign lesion can be left for observation as many stay stable and may even regress without intervention (Davis, S. & Uwaydat, S., 2010). Hemangioblastomas, benign lesions that can occur in the eye, brain and spinal cord arise from new vascularized tissue and usually benefit from growth hormones such as vascular endothelial growth factors (VEGF). Certain medications such as bevacizumab (Avastin) or ranibizumab (Lucentis) may serve as antiangiogenic agents that can benefit individuals experiencing hemangioblastoma related complications in the eye. These agents have shown to reduce discharge from a cyst and improve vision, while having no effect on the size of the lesion (Davis, S. & Uwaydat, S., 2010).
Recent Advances in Cancer Treatment
Stadtmauer, E. A., Fraietta, J. A., Davis, M. M., Cohen, A. D., Weber, K. L., Lancaster, E., … June, C. H. (2020). CRISPR-engineered T cells in patients with refractory cancer. Science, 367(6481). doi: 10.1126/science.aba7365
crispr-engineered_t_cells_in_patients_with_refractory_cancer.pdf
Background Information: Gene Editing
Gene editing has been a revolutionary discovery for the field of science because it is an opportunity to correct DNA mutations. It is a method in which we can treat or eliminate countless human genetic disease. Gene editing has the ability to change the DNA of cells with single-base pair precision. Genetic material can be added, removed or altered at a particular location in the genome. A recent advance in gene editing is the discovery of CRISPR-Cas9, short for clustered regularly interspaced short palindromic repeats and CRISPR-associated protein 9.
CRISPR-Cas9
CRISPR-Cas9 is adapted by naturally occurring genome editing system that is used by bacteria when it detects viral DNA. When viral DNA is detected inside the bacteria, the bacteria creates two short RNA's, one of which is an exact match to a segment on the viral DNA. The two short RNAs go on to form a complex with Cas9 (a nuclease). A nuclease is an ezyme that can DNA. The matching RNA (also known as the guide RNA), finds its matching target within the viral DNA. Following the match, Cas9 cuts the target DNA which disables the virus.
Continuous research with CRISPR-Cas9 made discoveries that later allowed for its use in test tubes and within the nucleus of a living cell as well. Once it is inside the nucleus, the CRISPR-Cas9 complex can lock onto the known short sequence (also known as PAM) and then using its molecular scissors it cuts the DNA. The cell will try and fix this damage, how ever the repair process is highly error prone, with leads to mutations. These mutations disable the gene.
Further research, allowed for the discovery that this mutated gene can be replaced with a healthy copy by just adding another piece of DNA which carries the desired sequence.
To best explain how CRISPR-Cas9 works an animation and video is optimal. Understanding CRISPR-Cas9 is an important aspect for the study being done.
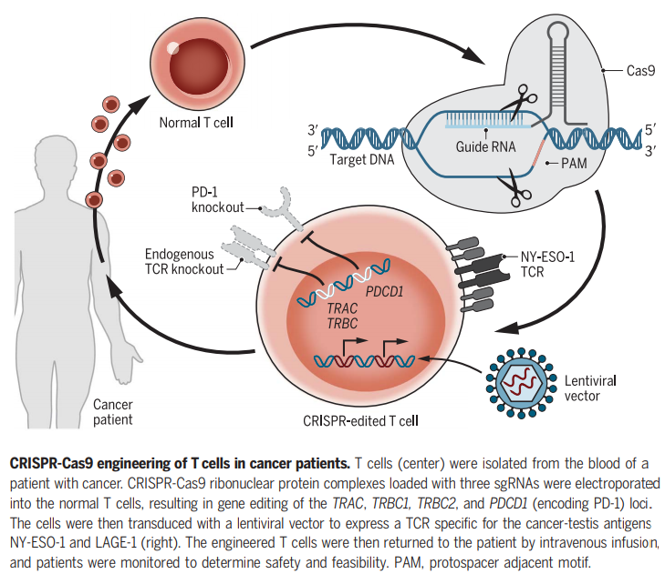
What did the study do?
The researchers began by collecting the patients T-cells from their blood. Following that, they used the CRISPR-Cas9 system to edit three genes (TRAC, TRBC, PD-1). TRAC and TRBC are the T-cell's natural receptors and they were removed and reprogrammed to express a synthetic T-cell receptor which would seek out and destroy tumors. The research article mentions that the transgenic TCR ( T-cell) Receptor has been shown to mis pair and/or compete for expression with the a and b chains of the endogenous/original TCR. Mispairing of the therapeutic TCR a and b chains with endogenous a and b chains reduces therapeutic TCR cell surface expression and potentially generates self-reactive TCRs. The third edit removed PD-1, a natural checkpoint that sometimes blocks T cells from doing their job. Once the three genes are knocked out, a fourth genetic modification was accomplished using a lentivirus to insert the cancer-specific synthetic T cell receptor, which tells the edited T cells to target an antigen called NY-ESO-1. Previously published data show these cells typically survive for less than a week, but this new analysis shows the edited cells used in this study persisted, with the longest follow up at nine months.
Conclusion
In conclusion, cancer is a very complicated disease that can develop in any part of the body. As mentioned, the causes of cancer are diverse, typically resulting in the disruption of genes monitoring cell cycle growth. Rare cancers, such as VHL are defined as cancers affecting 1-3% of the population. 80% of VHL cases are familial, meaning it is commonly observed in individuals with a family history of VHL. VHL lesions, both benign and malignant can cause damage to the affected organ. Similar to other cancers, malignant VHL tumors have the potential to metastasize becoming fatal. Hence, a lot of research is being conducted on cancer, focusing on finding an effective cure as many therapies offered today are time extensive and painful with many other adverse effects. Thus, research on more efficient types of cancer therapies is being conducted. One such discovery has been made involving CRISPR-Cas9 that entails genetic engineering of T-cell receptors to specifically target cancer cell antigens. Although in its initial stages, if successful, this therapy has the potential to treat multiple types of cancer in a unique way that allows health care physicians to use the patient’s own immune system to combat the disease effectively.
References
Bader, H., & Hsu, T. (2012). Systemic VHL gene functions and the VHL disease. FEBS Letters, 586(11), 1562-1569. https://doi.org/10.1016/j.febslet.2012.04.032
Cancer. (2018, September 12). Retrieved March 3, 2020, from https://www.who.int/news-room/fact-sheets/detail/cancer
Cancer. (2018, December 12). Retrieved March 4, 2020, from https://www.mayoclinic.org/diseases-conditions/cancer/symptoms-causes/syc-20370588
Genetic and Rare Disease Information Center (GARD). (2016). Von Hippel-Lindau disease. https://rarediseases.info.nih.gov/about-gard/pages/23/about-gard
Hwang, J. J., Walther, M. M., Pautler, S. E., Coleman, J. A., Hvizda, J., Peterson, J., … & Wood, B. J. (2004). Radio frequency ablation of small renal tumors: intermediate results. The Journal of urology, 171(5), 1814-1818.
Lonser, R., Kim, H., Butman, J., Vortmeyer, A., Choo, D., & Oldfield, E. (2004). Tumors of the Endolymphatic Sac in von Hippel–Lindau Disease. New England Journal Of Medicine, 350(24), 2481-2486. https://doi.org/10.1056/nejmoa040666
Maher, E., Webster, A., & Moore, A. (1995). Clinical features and molecular genetics of Von Hippel-Lindau disease. Ophthalmic Genetics, 16(3), 79-84. https://doi.org/10.3109/13816819509059966
Mukhopadhyay, B., Sahdev, A., Monson, J., Besser, G., Reznek, R., & Chew, S. (2002). Pancreatic lesions in von Hippel-Lindau disease. Clinical Endocrinology, 57(5), 603-608. https://doi.org/10.1046/j.1365-2265.2002.01637.x
Nall, R. (2020, January 6). Cancer: Overview, causes, treatments, and types. Retrieved March 4, 2020, from https://www.medicalnewstoday.com/articles/323648
National Organization of Rare Diseases (NORD). (n.d.). Von Hippel-Lindau Disease. Retrieved from https://rarediseases.org/rare-diseases/von-hippel-lindau-disease/
Partial Nephrectomy. (n.d.). John Hopkins Medicine. Retrieved from https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/partial-nephrectomy
Poulsen, M., Budtz-Jørgensen, E., & Bisgaard, M. (2010). Surveillance in von Hippel-Lindau disease (vHL). Clinical Genetics, 77(1), 49-59. https://doi.org/10.1111/j.1399-0004.2009.01281.x
Sakaguchi, M. (2012). von Hippel-Lindau Disease. Journal Of Nihon University Medical Association, 71(4), 237-239. https://doi.org/10.4264/numa.71.237
Varshney, N., Kebede, A., Owusu-Dapaah, H., Lather, J., Kaushik, M., & Bhullar, J. (2017). A Review of Von Hippel-Lindau Syndrome. Journal Of Kidney Cancer And VHL, 4(3), 20. https://doi.org/10.15586/jkcvhl.2017.88
Vortmeyer, A., & Alomari, A. (2015). Pathology of the Nervous System in Von Hippel-Lindau Disease. Journal Of Kidney Cancer And VHL, 2(3), 114. https://doi.org/10.15586/jkcvhl.2015.35
Von Hippel-Lindau disease. (n.d.). Retrieved from https://rarediseases.info.nih.gov/diseases/7855/von-hippel-lindau-disease
Von Hippel-Lindau syndrome - Genetics Home Reference - NIH. (2020, March 3). Retrieved from https://ghr.nlm.nih.gov/condition/von-hippel-lindau-syndrome#genes
What Is Cancer? (2015, February 9). Retrieved March 4, 2020, from https://www.cancer.gov/about-cancer/understanding/what-is-cancer