This is an old revision of the document!
Table of Contents
Presentation Slides
Introduction
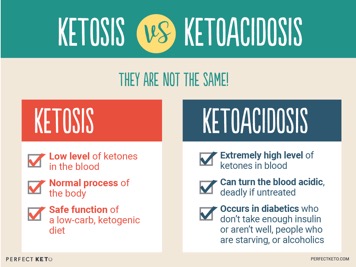
The Ketogenic Diet (KD) consists of low carbohydrates, and high fats. This forces the body to shift its primary source of fuel from carbohydrates to fats, resulting in an elevated production of ketones. With a normal diet, carbohydrates are broken down, and the body is supplied with glucose. Glucose is then used for energy throughout the body, which is especially important for the functioning of the brain. When the body is deprived of carbohydrates, like in the case of a KD, the liver begins to break down fats into ketones, which can also be used as a source of energy by the body and brain. Ultimately, the term ketogenic itself can be directly translated to mean the production of ketones in the body. By increasing ketone levels in the blood, the metabolic state of ketosis is achieved. The concept of KD mimics the body’s innate survival mechanism.[16] In the case of literal starvation, the body must burn its own fat and enter ketosis, and provide the body with another source of energy to stay alive. [17] In this way, KD allows the body to trigger ketosis without having the body actually starve. KDs ability to shift the body’s metabolic state, and decrease blood sugar and insulin levels, allows it to be a promising lifestyle filled with health benefits. [6]
Types of Diets
There are various types of KD, including: standard KD, high-protein KD, cyclical KD, and targeted KD. The standard KD consists of high fats, low carbohydrates, and sufficient protein. Similarly, the high-protein KD, is high on fats and low on carbohydrates, but has a relatively higher level of protein intake. Cyclical KD, however, allows days of high carbohydrate intake. Whereas, targeted KD allows for carbohydrate intake around one’s workout times. Although there are different types of KD, the standard version is the most researched and supported. The cyclical and targeted KDs are predominantly used by athletes and bodybuilders. [10]
History
Although KD is known as a relatively new and popular method for weight loss, it has been around for decades. Specifically, in the early 1920s, KD was introduced as an alternative treatment for epilepsy in children.[5] During this time,the few drugs that were available for epilepsy treatment were not only ineffective in controlling seizures, but they also has adverse side effects. With the belief that seizures are a result of intoxication in the brain from the intestine, Hugh Conklin introduced fasting as a treatment for epilepsy. In his 1922 report, Concklin expressed the efficacy of starvation as a treatment for epilepsy. Even before the release of his paper, word about the potential success of fasting as a treatment method spread to mainstream medicine. Studies were conducted to examine the relationship between fats, carbohydrates, and proteins. [5] Ultimately, in 1921 the ketogenic diet was introduced to clinical practice to treat epilepsy. The numbers from studies proved that KD has great promise in treating epilepsy. The diet consisted of sufficient protein to promote growth, minimal carbohydrates, and high levels of fats to provide enough calorie intake. This diet is essentially identical to the standard version used today.[5]
The Efficacy of Ketogenic Diet as a Treatment for Epilepsy
A dramatic outcome was reported by John Hopkins authors to demonstrate the efficacy of KD for children with epilepsy. In addition to examining the outcomes of 150 children 3, 6, and 12 months after diet implementation, they also followed up 3 to 6 years later. During the 12-month follow up, 20% of the children had a reduction in seizure frequency by 90%. Another 7% of the children were completely seizure free. 3-to 6- years after implementing the diet, 27% of the same children, had few to no seizures– many of them were now off the diet and on few to no medication.[8]
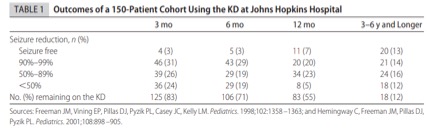 Studies, reporting back to even the 1920s, have been exceptionally consistent in identifying on the efficacy of KD as a treatment for epilepsy. Generally, 30% had a >90% reduction in seizure frequency, and approximately 10%-15% of children were seizure free 1 year after diet initiation.[5]
Studies, reporting back to even the 1920s, have been exceptionally consistent in identifying on the efficacy of KD as a treatment for epilepsy. Generally, 30% had a >90% reduction in seizure frequency, and approximately 10%-15% of children were seizure free 1 year after diet initiation.[5]
To this day, KD is an effective treatment for epilepsy, regardless of the new anticonvulsant drug treatments available. Specifically, KD is the best option to treat children with epilepsy who do not respond to drug options. Ultimately, KD allows the number and severity of seizures to be reduced, and helps with behavioural improvement. It is important to consider that KD is a treatment option for children and adolescents with epilepsy, more evidence on the efficacy in adults is needed. [14]
Sample Diet plan
The Ketogenic diet, contrary to popular belief, has a lot of variety in terms of edible options on the menu. To fit the standard macronutrients, there is often a range that people want to aim for in terms of the big three categories: fats, proteins and carbohydrates. The Ketogenic diet essentially strays away from using glucose as a fuel source and uses ketones as the primary energy source in the body. Thus, it becomes apparent that this diet would stay away from carbohydrates that would pump glucose throughout your body. Albeit the average range varies depending on BMI, people tend to aim for around 70% of calories from fat, 20% from protein and 10% from carbohydrates.
To find the ideal diet plan for your lifestyle, the most important variable to consider is the threshold at which your body will retain the ketosis state. A good way to estimate this range is to take the recommended nutritional caloric intake for your age group and divide that by 10 to arrive at your carbohydrate ceiling (in cals). Since nutritional information is given in grams, the number of calories from carbohydrates would be divided by 4 as that is how many calories are in each gram of carbohydrates.
Once this value is achieved it becomes relatively easy to organize a sample diet plan.
The following sample diet plan is for a 180 pound 21-year-old male with a caloric intake of 2000 cals/day.
Carbohydrate ceiling would be 2000 calories *0.10 = 200 calories/4 = 50g
This diet is designed to decrease intake as the day progresses (breakfast will be more carb heavy than dinner).
Breakfast (Allowed carbs: 25g)
As this meal is the laxest with daily carbohydrates, there is quite a range of food available for consumption. A common staple that ketogenic dieters love are eggs because they're very low carb (<2g) and they are quite tasty. There is room to fit in a slice of toast, however, the preferred type would be a thin, flax slice as they are under 10g each. A good drink compliment would be a coffee with really low cream and sweeteners instead of sugar for taste. In the ketogenic diet, any food or drink item that utilizes pure sugar is most likely out of the edible spectrum.
Lunch (Allowed carbs: 15g)
As we move later throughout the day, the allocated carbohydrates slowly begin to decrease but the allocated calories can either stay the same or increase. A big reason for this trend is due to the types of foods that are traditionally set aside for lunch. There are a lot lower carb options compared to breakfast as people tend to gravitate away from lots of meat during breakfast. A good starter would be a sliced 3-ounce chicken breast because it has <1g of carbohydrates. To taste, a few leafy vegetables such as asparagus or broccoli can be eaten in moderation. Almost all sweetened drinks are off the table, however, a hand-squeezed lemonade without sugar is a good alternative.
Dinner (Allowed carbs: 10g)
As the final meal of the day, this portion has very few carbohydrates allocated to it because there is a plethora of available items to be eaten. Almost anything is traditionally acceptable to eat at dinner so there are many options available. A good staple meal would be to mix cheese with quinoa and add an optional meat to it. Quinoa does have a few carbohydrates in it, but not enough to make a difference. Cheese also has very carbohydrates (<1g for 100g) which makes it extremely ideal to fill up on your daily calories. As a drink, just water with dinner or a black coffee would help you stay within your carbohydrate ceiling.
The Ketogenic diet has been recently used to combat epilepsy in children as a first mode of treatment. The mode of calculating macronutrients is the same as for healthy and active patients. The challenge that arises in the diet is primarily due to the age of the children because some of the foods normally eaten don't have enough nutritional benefits for their growing bodies. A good example would be feeding a 3 year old a heavy chicken breast with cheese, it just isn't suitable for them. [7]
Mechanism of Ketogenic Diet (KD)
During a ketogenic diet, the body shifts from a primarily glucose metabolism to a lipid metabolism due to the low carbohydrate and high fat presence.[1,12] When the body runs out of carbohydrates and insulin is no longer secreted, it shifts to utilizing the fat in the diet as well as adipose tissue, thus entering a state known as ketosis.[12]
Ketone Bodies
Dietary fat and free fatty acids (FFA) are converted by the liver into ketone bodies, which are three water soluble molecules known as 3-hydroxybutyrate, acetoacetate, and acetone.[6,12] Both 3-hydroxybutyrate and acetoacetate are dimers of acetyl coenzyme A, which is a transportable form of energy. The ketone bodies are then circulated around the body via the blood and absorbed by tissues for use in cells with a mitochondria. Once the ketone bodies are taken up by tissues they are broken down into acetyl CoA. [6]
Lipolysis
In a ketogenic diet, tissues begin the process of lipolysis. Adipose tissue fatty acids undergo lipolysis due to the activation of beta-adrenergic catecholamines.[6] These are highly sensitive to insulin such that if insulin levels rise, this pathway would shut off. This process maintains homeostasis as insulin would only be secreted when there is excess glucose in the blood, which would allow the body to shift back to using glucose as the primary source of fuel and fatty acids (FA) would not need to be broken down for energy. When beta-adrenergic activation has occurred, cyclic AMP levels increase and activate protein kinase A (PKA). PKA phosphorylates hormone-sensitive lipase (HSL) via various serine residues on the protein.[6] HSL then interacts with adipocyte fatty acid binding protein (aP2) to prevent local accumulation of FA, thereby releasing the FA into circulation. When there is high concentration of acetyl-coenzyme A (Ac-CoA) formed through the oxidation of FA, the liver converts it into acetoacetate (AcAc), which is one of the three ketone bodies. Overproduction of AcAc leads to conversion to 3-Hydroxybutyrate (3HB) which is the main ketone body in circulation and is picked up by various tissues for use in energy metabolism.[6] Once picked up by the tissues 3HB is brought to the mitochondria, where it is converted back into AcAc via 3-hydroxybutyrate dehydrogenase. A protein complex known as SCOT converts AcAc to acetoacetyl-coenzyme A (AcAc-CoA). This complex also uses succinyl-CoA in the process resulting in succinic acid as a byproduct. AcAc-CoA is converted into two molecules of Ac-CoA via an enzyme known as thiolase. These molecules then enter the Kreb’s/ TCA cycle where it is broken down into energy.[6]
Energy for the brain
The brain uses the most glucose for energy metabolism compared to any other organ in the body.[12] In a state of ketosis, there is a decrease in concentration of glucose available for use by the brain. While the rest of the body can utilize fatty acid oxidation as well as ketone bodies for energy production, the brain is limited. FFA are not able to cross the blood brain barrier due to their size, so the brain cannot oxidize fatty acids as an energy source.[1,12] Instead, the brain derives its energy through the use of ketone bodies. When circulating KB concentration reaches 4mmol/L the monocarboxylate transporter brings them into the CNS.[12] Here they undergo the same process as in other tissues (i.e. conversion of 3HB→ AcAc→ AcAc-CoA→ 2Ac-CoA).[6] Since this occurs in the mitochondria and axons are too far away from the main body of the neuronal cell to use KB as a source of fuel, they rely primarily on glucose.[12] This is consistent with the KD as the parameters of the diet include low carbohydrate intake and high fat intake. Therefore, there is a small amount of glycolysis occurring even during a KD. Although there is a lack of glucose intake, glucose levels within the blood remains within physiological levels, due to the breakdown of glucogenic amino acids as well as glycerol from triglycerides. Both these sources contribute to the glucose available to the brain.[6,12] Tissues such as the heart and muscle cells use ketone bodies over glucose, thereby allowing for more available glucose to be utilized by the brain. [6]
Treatment in other Diseases (low carb, moderate protein, high fat)
Obesity
Obesity is a rapidly increasing epidemic worldwide that has doubled since 1980.[11] It is a risk factor for various cardiovascular and metabolic disorders such as hypertension and type 2 diabetes.[11] In the society today, genetic predisposition, inactive lifestyles and high caloric intake all leads to uncontrolled weight gain.[11] Many studies have shown that the KD approach has a credible physiological and biochemical mechanism that has the ability to stimulate effective weight loss along with improvement in many cardiovascular disease risks.[11] Dashti et al (2004) conducted a study to determine the effects of a 24-week KD consisting of 30 g carbohydrate, 1 g/kg body weight protein, 20% saturated fat, and 80% polyunsaturated and monounsaturated fat in obese patients. In this experiment, 83 obese patients (39 men and 44 women) with a body mass index (BMI) greater than 35 kg/m2, and high glucose and cholesterol levels were selected.[4] The patient's’ body weight, BMI, total cholesterol, high density lipoprotein (HDL), low density lipoprotein (LDL), and triglycerides were monitored after 8, 16 and 24 weeks of treatment.[4] Dashti et al (2004) found that the body weight, BMI, and total cholesterol of the patients decreased significantly (P<0.0001). HDL cholesterol, the “good cholesterol” that travels in the bloodstream and removes extra cholesterol and carries it back to the liver which reduces the risk for heart disease, has significantly increased after treatment.[4] Whereas the level of LDL cholesterol has significantly decreased after treatment.[4] The level of triglycerides decreased significantly following 24 weeks of treatment as well.[4] The study also finds that administering a ketogenic diet for 24 weeks did not produce any significant side effects in the patients.[4] As a result, the study demonstrates the beneficial effects of a KD showing improvement in all the parameters being measured. [7]
Cancer
Cancer cells rewire their metabolism to increase rate of growth, survival, proliferation, and long-term maintenance.[9] The predominant characteristic of this altered metabolism is increased glucose uptake and fermentation of glucose to lactate.[9] This phenomenon is known as the Warburg Effect, where cancer cells uses aerobic glycolysis instead of oxidative phosphorylation to produce energy.[9] KD target the Warburg effect, since some cancers lack the ability to metabolize ketone bodies, due to mitochondrial dysfunction and down-regulation of enzymes necessary for ketone utilization.[19] Ketone bodies are produced by the liver from fatty acids and used as an energy source when glucose is not readily available during periods of low food intake or prolonged exercise.[9] The rationale in providing a fat-rich, low-carbohydrate diet in cancer therapy is to decrease glucose levels in the body and induce ketosis leading to the starvation of cancer cells while healthy cells modify their metabolism to use ketone bodies and survive.[19] Furthermore, by reducing glucose levels in the bloodstream also decreases levels of insulin and insulin-like growth factor, which are both vital for cancer cell proliferation.[19] Many preclinical studies have strong evidence indicating the anti-tumor effect of KD. In a study conducted by Weber, Aminazdeg-Gohari, & Kofler (2018), the researchers investigated the anti-tumor effect of KDs in combination with or without low-dose chemotherapy. They found that the growth of neuroblastoma, a type of cancer that forms in nerve tissues, significantly declined by a KD consisting of a 2:1 ratio of fat to carbohydrate & protein when combined with caloric restriction.[19] The result was as efficacious when administered an 8:1 ratio without caloric restriction.[19] In addition to neuroblastoma, glioblastoma has the strongest evidence for a KD tumor-suppressing effect, whereas little or no benefit was found for two other brain tumors, astrocytoma and medulloblastoma.[19] Thus, available preclinical evidence suggests the effectiveness of a KD as an adjuvant cancer treatment differs based on the type of tumor and its genetic alterations.[19]
Effects of the Diet
Positive Aspect
One positive aspect of the diet is that it loses body weight as intended by restricting carbohydrate intake.[4] It uses a natural mechanism of ketosis to achieve this by breaking down adipose fat tissue for energy.[4] The diet can be used over a couple of months due to its ability to use the high fat content to keep the stomach satiated, even though the body is still in ketosis.[4] The diet is best for people that do not have a very active lifestyle. For the KD diet it is beneficial for people that have desk jobs or that don’t have physical activity. For these people the body is storing all the carbohydrates into fat, since the carbohydrates are not being used by the body.[13] Therefore if those extra carbohydrates are cut out from their diet then weight loss is possible. The KD will still works for people that exercise for certain periods of the day, like going to the gym for 30 minutes. These people can use the targeted KD or cyclic KD to increase carbohydrate intake before and after workout session to ensure they have enough carbohydrates for their exercise.[13] The KD has been linked to having medical applications in people with diabetes, Parkinson’s disease, Alzheimer’s disease and epilepsy. KD is linked to insulin sensitivity for diabetics, because the body is no longer using glucose as a form of energy. So, when the KD is stopped and a regular diet is reintroduced the body reacts better to insulin, because it had a chance to become more receptive to the insulin.[18] It has been shown that this does not affect the patient’s performance or endurance.[18] It is also linked to neurological diseases, like Alzheimer’s, because the normal pathways that the brain uses for energy are not used and this can disrupt the diseases progression and symptoms.[15]
Negative Aspects
Glucose is the primary fuel for the brain, therefore it cannot be taken out of the diet indefinitely. There are short-term problems with starting the diet, such as fatigue and dizziness due to the brain not receiving energy.[15] For this reason the diet can only be used short-term and not be used indefinitely. The body also requires carbohydrates in order to fuel muscles using muscle glycogen, therefore if your body is not getting enough carbohydrates it will not function optimally.[13] For this reason, the diet is not recommended for people that are extremely active, as their performance will lose performance and endurance unless a dietitian helps determine exactly how many carbohydrates are required in order to maintain ketosis. A person that exercises more will require a higher carbohydrate ceiling than someone that does not exercise as much. It becomes more difficult to maintain ketosis for these people, since variability in the type of exercise or the schedule will make staying in ketosis very difficult.[13]
Also, any water-loss due to the diet will come back after the diet, because the water content will return when you switch back to a regular diet. A KD focuses on counting carbohydrates, so that the patient can maintain ketosis, however, the patient is not counting their calorie input or output. Essentially, carbohydrates do not directly translate to weight loss, instead a loss of calories directly translates to a loss of weight.[4] This is due to the fact that weight loss is due to more calories being used then being stored, regardless of the macronutrient (carbohydrate) ratio used.[4]
Side Effects
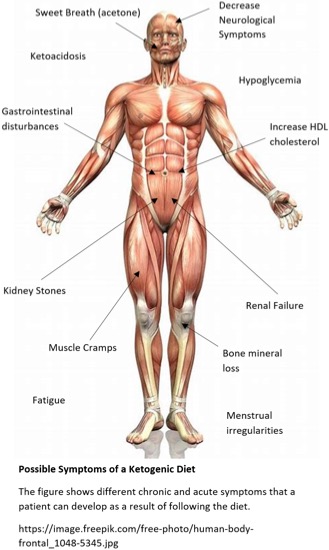
The positive symptoms of KD include a decrease of epileptic seizures as shown by Hemingway, C. et al (2001). The diet also increases insulin sensitivity which can help diabetic’s better control their blood sugar levels.[18] A KD also improves the cardiovascular system by increasing HDL Cholesterol (good cholesterol) which decreases the chances for heart disease by removing LDL cholesterol in the bloodstream and sending it to the liver.[2] It is also linked to a decrease in tumor sizes depending on if the tumor needs the normal pathway for its energy supply to proliferate.[19] Similarly, the diet can also decrease symptoms from neurological disease, also depending on if the normal energy pathway aggravates the symptoms.[3] Negative symptoms related to the KD diet include short-term (2-4 weeks) neurological symptoms due to a lack of glucose energy for the brain, such as dizziness and fatigue.[3] Chronic symptoms include ketoacidosis (increased ketone levels in the body which are acidic and can affect the pH of blood which can cause problems for other organ systems in the body), gastrointestinal disturbances, kidney stone (liver cannot process the ketone bodies properly), renal damage, hypoglycemia (low glucose levels in the blood) and increase in LDL cholesterol (normally an increase in HDL cholesterol leads to a decrease of LDL cholesterol in most of the population but for certain people it increases; certain genetic predispositions and diseases make people’s bodies respond to the loss of glucose by increasing production of LDL).[2] Other effects include, cardiomyopathy, muscle cramps (lack of muscle glycogen)13, and menstrual irregularities.[2]
References
[1] Barañano, K. W., & Hartman, A. L. (2008). The Ketogenic Diet: Uses in Epilepsy and Other Neurologic Illnesses. Current Treatment Options in Neurology, 10(6), 410–419.
[2] Brehm, B. J., Seeley, R. J., Daniels, S. R., & D’alessio, D. A. (2003). A randomized trial comparing a very low carbohydrate diet and a calorie-restricted low fat diet on body weight and cardiovascular risk factors in healthy women. The Journal of Clinical Endocrinology & Metabolism, 88(4), 1617-1623.
[3] Cheng, B., Yang, X., An, L., Gao, B., Liu, X., & Liu, S. (2009). Ketogenic diet protects dopaminergic neurons against 6-OHDA neurotoxicity via up-regulating glutathione in a rat model of Parkinson's disease. Brain research, 1286, 25-31.
[4] Dashti, H. M., Mathew, T. C., Hussein, T., Asfar, S. K., Behbahani, A., Khoursheed, M. A., Al-Sayer, M. H., Bo-Abbas, Y. Y., Al-Zaid, N. S. (2004). Long-term effects of a ketogenic diet in obese patients. Experimental & Clinical Cardiology, 9(3), 200-205.
[5] Freeman, J. M., Kossoff, E. H., & Hartman, A. L. (2007). The ketogenic diet: one decade later. Pediatrics, 119(3), 535-543.
[6] Fukao, T., Lopaschuk, G. D., & Mitchell, G. A. (2004). Pathways and control of ketone body metabolism: On the fringe of lipid biochemistry. Prostaglandins Leukotrienes and Essential Fatty Acids, 70(3), 243-251. https://doi.org/10.1016/j.plefa.2003.11.001
[7] Health Canada. (2011). Eating Well with Canada's Food Guide: A Resource for Educators and Communicators. Publications Health Canada.
[8] Hemingway, C., Freeman, J. M., Pillas, D. J., & Pyzik, P. L. (2001). The ketogenic diet: a 3-to 6-year follow-up of 150 children enrolled prospectively. Pediatrics, 108(4), 898-905.
[9] Liberti, M. V., & Locasale, J. W. (2017). The Warburg Effect: how does it benefit cancer cells?. Trends Biochem Sci, 41(3), 211-218. doi: 10.1016/j.tibs.2015.12.001
[10] Mawer, R. (2018, July 30). The Ketogenic Diet: A Detailed Beginner's Guide to Keto. Retrieved September 20, 2018, from https://www.healthline.com/nutrition/ketogenic-diet-101
[11] Paoli, A. (2014). Ketogenic diet for obesity: friend or foe?. International Journal of Environmental Research and Public Health, 11(2), 2092-2107. doi: 10.3390/ijerph110202092
[12] Paoli, A., Bianco, A., Damiani, E., & Bosco, G. (2014). Ketogenic Diet in Neuromuscular and Neurodegenerative Diseases. BioMed Research International, 2014, 474296. http://doi.org/10.1155/2014/474296
[13] Pinckaers, P. J., Churchward-Venne, T. A., Bailey, D., & van Loon, L. J. (2017). Ketone bodies and exercise performance: the next magic bullet or merely hype?. Sports Medicine, 47(3), 383-391.
[14] Schoeler, N. (2016, March). Ketogenic diet. Retrieved September 20, 2018, from https://www.epilepsysociety.org.uk/ketogenic-diet#.W67K4qZKjIV
[15] Tiano, J., & Liebrecht, J. (2002). U.S. Patent Application No. 09/809,738.
[16] Vining EPG, Freeman JM, Ballaban-Gil K, et al. A Multicenter Study of the Efficacy of the Ketogenic Diet. Arch Neurol. 1998;55(11):1433–1437. doi:10.1001/archneur.55.11.1433
[17] Westman, E. C., Mavropoulos, J., Yancy, W. S., & Volek, J. S. (2003). A review of low-carbohydrate ketogenic diets. Current Atherosclerosis Reports, 5(6), 476–483. https://doi.org/10.1007/s11883-003-0038-6
[18] Westman, E. C., Yancy, W. S., Mavropoulos, J. C., Marquart, M., & McDuffie, J. R. (2008). The effect of a low-carbohydrate, ketogenic diet versus a low-glycemic index diet on glycemic control in type 2 diabetes mellitus. Nutrition & metabolism, 5(1), 36.
[19] Weber, D. D., Aminazdeg-Gohari, S., & Kofler, B. (2018). Ketogenic diet in cancer therapy. Aging, 10(2), 164-165. doi: 10.18632/aging.101382
[20] Wheless, J. W. (2008). History of the ketogenic diet. Epilepsia, 49, 3-5.