This is an old revision of the document!
Pathophysiology
The limbic brain regions associated with mood and depression include the hippocampus and the prefrontal cortex. Studies suggest that stress and depression are associated with atrophy and loss of neurons and glia, which contribute to the decreased size and function of these brain areas.
break
The Monoamine-deficiency hypothesis:
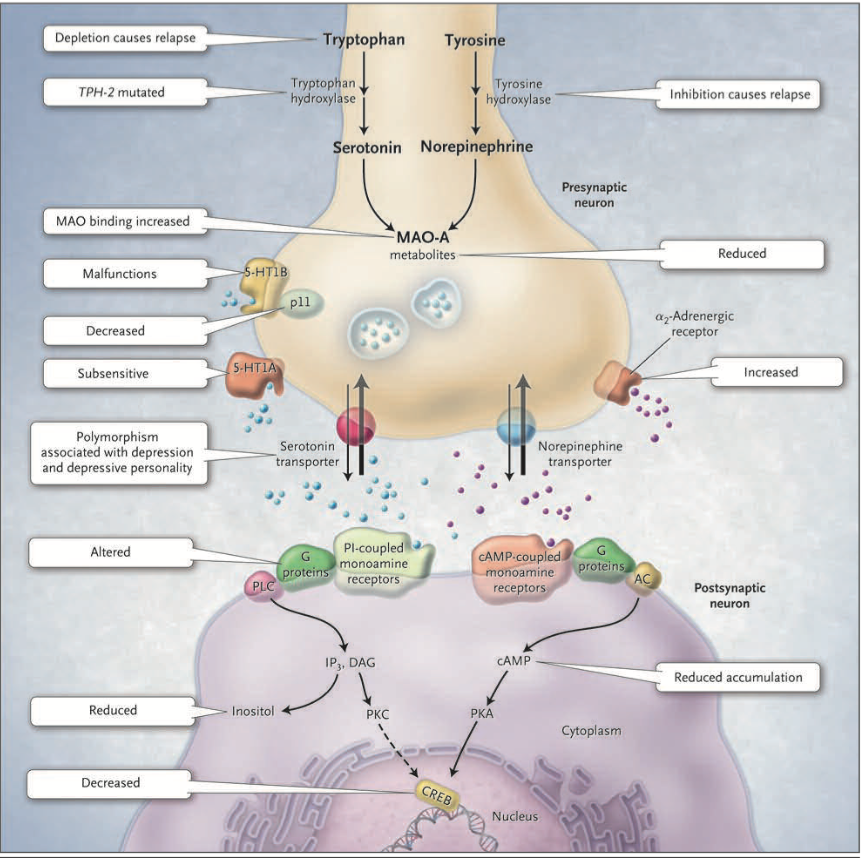
The first real indication that depression might result from a problem with the central nervous system modulatory systems came in the 1960s. A drug called reserpine, introduced to control high blood pressure, caused psychotic depression in about 20% of cases. Its mechanism of action involves the depletion of central catecholamines and serotonin by interfering with their loading into synaptic vesicles. Another class of drugs introduced to treat tuberculosis caused a marked elevation in mood. These drugs inhibit monoamine oxidase (MAO) which is the enzyme that degrades catecholamines and serotonin in the synaptic cleft. Furthermore, when it was discovered that the drug imipramine, introduced as an antidepressant years earlier, inhibits the reuptake of released serotonin and norepinephrine, thus promoting their action in the synaptic cleft. As a result of these observations, researchers developed the hypothesis that mood is closely tied to the levels of released monoamine neurotransmitters, norepinephrine and/or serotonin, in the brain. According to this monoamine hypothesis, depression is a consequence of a deficit in one of these diffuse modulatory systems.