Table of Contents
Atrial Fibrillation
Background
What is Atrial Fibrillation?
Atrial fibrillation (AF) is a condition characterized with an irregular and rapid activation of the atrium, consequently leading to an irregular heart rhythm (arrhythmia). Normally, the sinoatrial node, known as the cardiac pacemaker, controls the rhythmic contractions of the heart [4]. The sinoatrial node maintains the heart rate at 60 bpm at rest and fires at 180-200 bpm for intense physical activity. However in AF, the heart can beat to a rate of 400-600 bpm [6]. AF is the most common type of arrhythmia as around 350, 000 Canadians are affected [12].
In addition, AF can escalate to cardiac morbidity from stroke, heart failure, impaired quality of life and thromboembolism. The prevalence of AF has been substantially increasing as the elderly baby boomers are comprising a great portion of the population. Some general risk factors for the development of AF include diabetes, high blood pressure, increased age and heart disease [8]. Individuals suffering from AF have a high risk of stroke. AF can increase stroke risks by <hi #ffff00>5-folds</hi>. In addition, 1 in 6 strokes occur in patients suffering from AF [11].
Classification of Atrial Fibrillation
AF has been classified on the basis of the frequency and severity of episodes. The three main forms of AF include Paroxysmal, Persistent and Permanent [5].
Paroxysmal Atrial Fibrillation Episodes terminate spontaneously after no more than a few days (usually lasting less than 24 hours).++| Faulty electrical signals and rapid heart rate initiate sporadically and then self-terminate. Symptoms can range from being mild to severe [3].++
Persistent Atrial Fibrillation Episodes with abnormal heart rhythms last for longer than a week. ++| Generally, the termination of episodes require electrical or pharmacological cardioversion therapy [3].++
Permanent Atrial Fibrillation
This is the most severe type of AF. ++| The normal sinus rhythm can't be restored with cardioversion[3]. ++
Living with Atrial Fibrillation
Symptomatology
<style float-right>
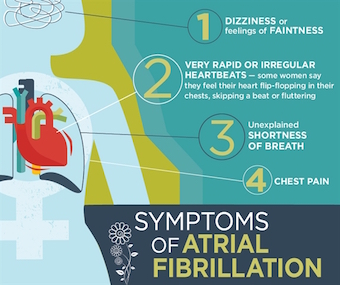
Figure 1: Commonly Reported Symptoms of Atrial Fibrillation [9].</style>
Although AF may present itself as an asymptomatic disorder, up to two thirds of patients report that the arrhythmia is disruptive to their day-to-day activities [9]. The presentation of symptoms can vary, depending on the individual's cardiac function, concomitant medical issues and ventricular rate [7]. Most patients report experiencing the following [7]:
- Palpitations
- Irregular and rapid heartbeat
- Chest pain and discomfort
- Shortness of breath
- Fatigue
- Presyncope
- Dizziness
- Dyspnea
Onset of Atrial Fibrillation: The Role of Triggers and Substrates
<style float-left>
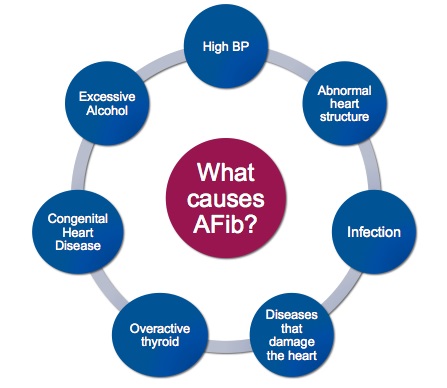
Figure 2: A general outline of the triggers involved in inducing</style>
atrial fibrillation [1].
AF requires a trigger that initiates the arrhythmia, and a substrate that further sustains the arrhythmia and its symptoms [1]. Triggers are extremely diverse and include high blood pressure, abnormal heart structure, infections, diseases that damage the heart, an overactive thyroid, congenital heart diseases, and excessive alcohol [1].
Ectopic foci occurring in atrial tissues have also recently been identified as an AF trigger [1]. Once AF occurs, arrhythmias may occur even in the absence of the original trigger [1].
Some of the substrate that sustains the abnormal heart rhythm include abnormal calcium handling and an altered action potential due to irregular ion currents [1].
Pathophysiology
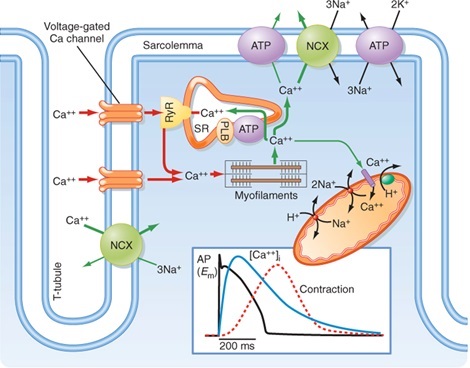
<style float-middle>
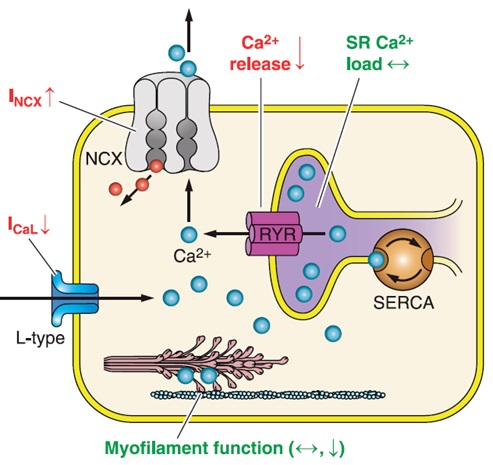
Figure 3: An illustration of the improper calcium handling of myocardial cells inflicted with atrial fibrillation. Note that adaptive responses include the upregulation of NCX, a decrease in calcium current, and a decrease in calcium release from the sarcoplasmic reticulum.[1] </style>
As noted as one of the substrates that sustains AF, the mishandling of excessive calcium occurs due to a cascade of abnormal amounts of repetitive atrial excitations [10]. Fundamentally, this mishandling occurs due to ectopic action potentials via afterdepolarizations [10].
As a result of this mishandling of calcium within myocardial cells, the body engages an adaptive response to upregulate NCX channels (Na+/Ca2+ exchanger), decrease the Ca2+ current, and impair the release of Ca2+ from the sarcoplasmic reticulum [10]. As a result of this adaptive response, there is a total decrease in the concentration of Ca2+ within myocardial cells of the atrium, directly resulting in contractile dysfunction due to the reduced activity of myofilament function [10].
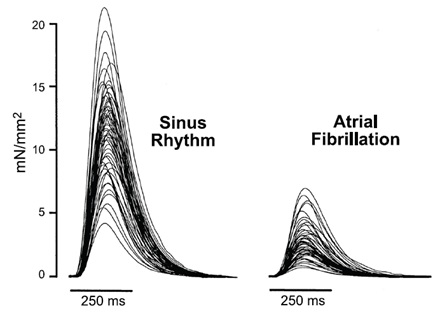
This can be quantitatively seen in a group showing the relationship between pressure and time of the atrial contraction; compared to normal sinus rhythms, atrial myocardial cells demonstrate a significant depression of the action potential plateau[10]. Potential effects stemming from AF include stasis of the atria, leading to thromboemboli, and further downstream a cardiac infarction (also known as a heart attack) [10].
<style float-left>
Figure 4: The relationship between pressure and time of the atrial </style>
contraction, comparing the normal sinus rhythm (left) with the sinus
rhythm suffering from atrial fibrillation (right) [10].
Normal Sinus Rhythm
The sinoatrial (SA) node, located in the right atrium is known as the pacemaker of the heart and is responsible for initiating action potentials via spontaneous firing. The pathway of the action potential is as follows: the action potential begins in the atria, then travels to the AV node, and finally to the ventricles. Together, this triggers coordinated contraction of the heart, and pushes blood out of the heart and into systemic circulation [1].
Normal Excitation Coupling
Cardiac excitation - contraction coupling is the manner in which electrical excitation generates contraction of the heart.
Calcium plays a key role in the regulation of cardiac contractility, and is the activator of myofilaments; the key structures responsible for contraction. During the onset of an action potential within cardiomyocytes, intracellular calcium enters through depolarized activated calcium channels contributing to the characteristic cardiac action potential plateau. Subsequently, calcium entry prompts calcium release from the sarcoplasmic reticulum via the ryanodine receptors [1]. Thus, the intracellular concentration of calcium rises and calcium then binds to the myofilament protein troponin C.
In order for relaxation to occur, the intracellular concentration of calcium must decrease, which allows for calcium to dissociate from troponin. Calcium is then transported out of the cytosol by four pathways++| utilizing the sarcoplasmic reticulum ATPase, sarcolemma Na+/Ca2+ exchange, sarcolemma Ca2+ transport ATPase or mitochondrial CA2+ uniport [1]. ++
<style float-right>
Figure 5: The role of calcium in normal excitation coupling
Normal Excitation Coupling
Excitation within the heart is characterized by two phases; systole and diastole. During systole, calcium is released inside the sarcomere leading to an increase of intracellular calcium. Calcium then binds to troponin initiating contraction of the heart, and blood from the heart is pumped throughout the body. Subsequently, during diastole there is an uptake of calcium into the sarcoplasmic reticulum via the Ca2+ ATPase. This then results in relaxation of the heart [1].
Sinus Rhythm in Atrial Fibrillation
Atrial fibrillation is characterized by an irregular heart rhythm that begins in the atria. Contrary to normal sinus rhythm where the SA node is responsible for initiating action potentials, in atrial fibrillation there are many different impulses that all rapidly fire at once leading to a very rapid rhythm in the atria. The consequence of this rapid rhythm is that the atria cannot contract or squeeze blood into the ventricle. Thus, in affected patients there is a large number of impulses that get into the ventricle leading to irregular contraction and subsequently an irregular and rapid heartbeat [2].
Managing Atrial Fibrillation
Treatment Objectives
Atrial fibrillation cannot be 'cured', however, many treatments are available to manage the symptoms. In particular, the objectives of atrial fibrillation treatment are to:
- Reset the abnormal heart rhythm back to normal sinus rhythm or to control the rate [2].
- Prevent and/or reduce the likelihood of developing blood clots that may lead to strokes, pulmonary emboli, deep vein thrombi, and other complications [2].
There are four main treatment options.
Treatment Options
1. Anticoagulants
Individuals with this condition, usually receive anticoagulants immediately to reduce risk of stroke and myocardial infarction. As the name implies, 'anti'-coagulants prevent clot formation. A commonly used anticoagulant is Warfarin (also known as Coumadin); these are blood thinners [13].
The dosage of anticoagulant is crucial and is monitored carefully by regularly testing INR-especially during initial use. This is because excessive dosages can lead to abnormal and/or excessive bleeding and can be potentially life-threatening [13].
<style float-left>
Figure 6: Cardioversion [13]</style>
2. Cardioversion
This medical procedure is done to restore normal sinus rhythm of the heart. There are two types of cardioversion, the most common being electrical cardioversion. With electrical cardioversion, synchronized electrical pulses are delivered through electrodes [2].
This procedure prevents the atria from contracting during the refractory period. The second type of cardioversion is drug cardioversion, where numerous antiarrhythmics are used to revert the heart back to normal sinus rhythm [13]. The two different types can be used in conjunction or separately.
3. Antiarrhythmics
Class of pharmaceutical drugs that are used to help control and maintain normal sinus rhythm [5]. They suppress cardiac arrhythmias by working as ion channel blockers. One of the newest antiarrhythmic options is Dronedarone. Other commonly used antiarrhythmics are Amiodarone and Sotatol. They work by inhibiting potassium channels; this, prolongs the duration of depolarization and/or lengthens the refractory period [13].
4. Surgical Intervention
This treatment option would be the last resort of treatment. Surgical intervention involves physical damage to the heart cells [13]. This can be achieved by promoting formation of scar tissue in the myocyte cells. As a result, the scar tissue of the myocyte cells will not be able to conduct electrical signals. Usually, a pacemaker has to be inserted afterwards.
Two types of surgical interventions++| catheter ablation and the surgical maze procedure.++ Catheter ablation is when you selectively destroy areas of the heart by inserting a catheter through the groin. Surgical maze procedure is an open heart surgery where you use a scalpel to scar parts of the heart [5]. As mentioned, surgical intervention is the last resort; it is an invasive procedure and only used if severity of symptoms justifies the intervention.
<style center>Figure 7 - A Summary of Catheter Ablation For Atrial Fibrillation (AFIB). </style>
Concluding Remarks
There are many questions that need to be answered in order to better understand the mechanisms underlying AFib, such as the genes responsible for familial Afib and how they lead to arrhythmia. Continued research in determining the relative roles of ectopic activity, single-circuit reentry and multiple-circuit reentry in maintaining clinical AFib is important to better understand the mechanisms underlying AFib. Answering these questions will lead to new and improved possibilities in prevention and therapy.
References
[1] Allessie, M. A., Boyden, P. A., Camm, A. J., Kléber, A. G., Legato, M. J., Rosen, M. R., … & Waldo, A. L. (2001). Pathophysiology and prevention of atrial fibrillation. Circulation, 103(5), 769-777.
[2] Atrial fibrillation. (2015). Retrieved March 29, 2016, from http://www.mayoclinic.org/diseases-conditions/atrial-fibrillation/diagnosis-treatment/treatment/txc-20164944.
[3] Gallagher, Mark M., and A. Camm. “Classification of atrial fibrillation.” Pacing and clinical electrophysiology 20.6 (1997): 1603-1605.
[4] Lip, Gregory YH, and Hung-Fat Tse. “Management of atrial fibrillation.” The Lancet 370.9587 (2007): 604-618.
[5] Markides, Vias, and Richard J. Schilling. “Atrial fibrillation: classification, pathophysiology, mechanisms and drug treatment.” Heart 89.8 (2003): 939-943.
[6] Pai, G. R., and J. M. Rawles. “The QT interval in atrial fibrillation.” British heart journal 61.6 (1989): 510-513.
[7] Prystowsky, Eric N., et al. “Management of Patients With Atrial Fibrillation A Statement for Healthcare Professionals From the Subcommittee on Electrocardiography and Electrophysiology, American Heart Association.” Circulation 93.6 (1996): 1262-1277.
[8] Sage, J. I., and R. L. Van Uitert. “Risk of recurrent stroke in patients with atrial fibrillation and non-valvular heart disease.” Stroke 14.4 (1983): 537-540.
[9] Savelieva, Irina, et al. “Quality of life in patients with silent atrial fibrillation.” Heart 85.2 (2001): 216-217.
[10] Schotten, U., Verheule, S., Kirchhof, P., & Goette, A. (2011). Pathophysiological mechanisms of atrial fibrillation: a translational appraisal.Physiological reviews, 91(1), 265-325.
[11] Wolf, Philip A., Robert D. Abbott, and William B. Kannel. “Atrial fibrillation as an independent risk factor for stroke: the Framingham Study.” Stroke 22.8 (1991): 983-988.
[12] Xu, Yan, et al. “Prescribing patterns of novel oral anticoagulants following regulatory approval for atrial fibrillation in Ontario, Canada: a population-based descriptive analysis.” CMAJ open 1.3 (2013): E115-E119.
[13] Yap, Y. G., & Camm, J. (2014). Anticoagulant Treatment Strategies for Atrial Fibrillation. Essentials of Atrial Fibrillation, 37-47.