Table of Contents
Schizophrenia: A Severe Mental Disorder
Background
“1 in 100 individuals have schizophrenia in the general population.” [12]
Schizophrenia is complex to the degree that one is solving a puzzle without all the pieces. This neurological disorder inhibits the otherwise seamless distintion between what is fact and fiction; hence generating reality from a grey zone. Simply put, the brain incorrectly perceives signals and stresses in effect leading to false perceptions of reality. However, a common misconception is the belief that this serious mental illness is not treatable.
Clinical Symptoms
The current DSM IV determines an individual clinically schizophrenic if two or more of the following are persistently apparent.
- ++Delusions|Fixed false beliefs that can be terrifying to the person experiencing them.++
- ++Hallucinations|Sensory experiences aka hearing voices, imaginary friends, etc.++
- Disorganized speech
- Disorganized or catatonic behavior
- ++Negative symptoms|Includes social withdrawal and disturbed thinking.++
In some cases, severe cases of just delusions or hallucinations can warrant diagnosis.
Etiology
The cause of schizophrenia is unknown. However, there are numerous theories and hypotheses surrounding the etiology of schizophrenia. Ranging from an individual's genetic makeup, personal experiences in the womb to viral infections, there are numerous possible causes leading to the diagnosis of schizophrenia [13]. One of the most promising and studied theories revolves around brain activity and biochemical imbalances in the brain [13].
Genetic Factors
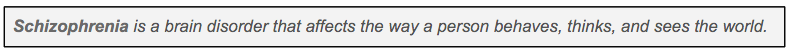
Figure 1: Rates of Schizophrenia Among Relatives
</style>
Several studies have shown that the incidence of schizophrenia and likelihood of developing schizophrenia is equal among males and females and all ethnicities [13]. However, other studies have argued this point. Regardless of these conflicting studies, it is generally accepted that schizophrenia has a strong hereditary component. Opposed to the 1 percent chance [14] of developing schizophrenia in the general population, individuals with a first-degree relative, such as a biological parent or sibling with schizophrenia, have a 10 percent chance of developing schizophrenia. Studies done on identical twins about schizophrenia have further strengthened the notion of hereditary in schizophrenia. It has been observed that if one twin develops schizophrenia, the other twin has a 50% chance of developing the condition [13].
Attempts to locate and identify specific genes and chromosomes related to schizophrenia have been difficult. There are hundreds of on-going studies examining the genome of schizophrenic individuals. Regardless its apparent hereditary nature, there is yet to be a gene that has been linked to increased risk of schizophrenia. However, the vast majority of current studies believe that schizophrenia arises due to effects of multiple genes, and/or combined effects of multiple susceptibility loci [13]. In particular, many scientists believe that the combination of genes increase the risk of developing this condition. It is also believed that chemical imbalances in the brain that are associated with schizophrenia are a result of inherited factors. It is important to acknowledge that there are numerous intertwined factors including genetics and the surrounding environment.
Environmental Factors
<style float-right>
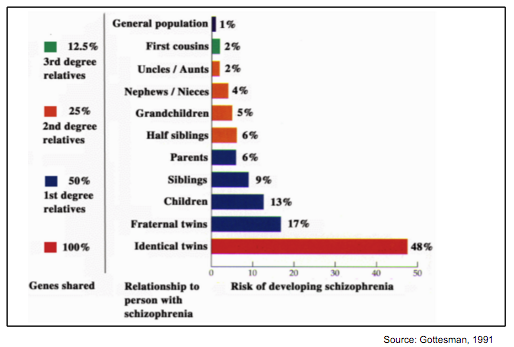
Figure 2: The Interaction Model
</style>
Certain situations trigger or increase the risk of developing schizophrenia, especially in those individuals that are already at risk of developing schizophrenia due to genetic predisposition [19]. Stressful events ranging from physical stress to emotional stress can trigger symptoms relating to schizophrenia. These stressful events are the most common trigger for schizophrenia. The nature of stresses induced on an individual can range from prenatal stress in the womb to drug and alcohol abuse.
Some common stressors include:
- ++Prenatal Stress| Infections, malnutrition, effects as early as the first trimester++ [19]
- ++Perinatal Stress| Infections, C-section, etc.++ [19]
- ++Infections| Viral infectons++ [18]
- ++Adolescence| Puberty, social changes, etc.++ [16]
- ++Drug Abuse| Cannabis, cocain, LSD, etc.++ [19]
- ++Psychosocial Factors| Dysfunctional family, area raised in, etc.++ [19]
- ++Emotional Stress| Epigenome++ [19]
- ++Adolescence| Puberty, social changes, etc.++ [19]
- Winter Birth [18]
It is important to note that environmental triggers alone are not sufficient to cause schizophrenia (for the most part) [14]. Thousands of individuals experience stressful situations throughout their lives without developing schizophrenia and the predetermined susceptibility is, therefore, significant. In other words, the interaction between genetics, brain activity, and other factors along with environmental triggers are generally required for the development of schizophrenia [19]. For example,++predisposing genetic factors| such as single nucleotide polymorphisms or copy number variations,++ may interact with a wide range of environmental factors. The combined effects may trigger a cascade of pathophysiological processes in the brain. These changes may eventually lead to maladaptive behaviors, thoughts and emotions related to schizophrenia [14].
Brain Structural Changes
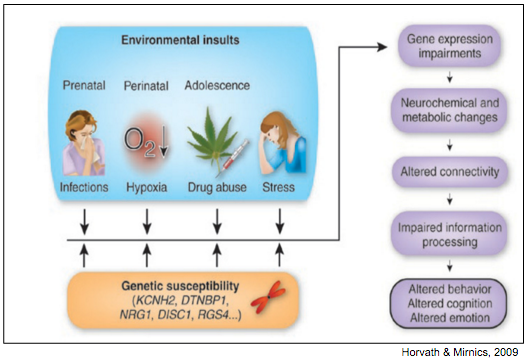
Individuals suffering from schizophrenia have abnormalities in brain structure and function. Autopsy studies have compared the brains of individuals who had schizophrenia from those who did not. The study found the brains of indiviudals with schizophrenia were atrophied in comparison to the brains of individuals without the disorder [12].
The characteristic brain structural abnormality in the brains of individuals with schizophrenia is enlarged cerebral ventricles. Cerebral vertices are the cavities in the center of the brain that contain the cerebrospinal fluid. The enlarged cerebral ventricles entails a reduction in brain size, which correlates with the autopsy findings mentioned above [21]. It has been suggested that the reduction in brain size could be due to medications used to treat schizophrenia. However this possibility was ruled out when a longitudinal study revealed that individuals with schizophrenia had smaller overall brain volume and a reduced cerebral schizophrenia at the time of their first episode. Thus, the enlarged cerebral ventricles is not a result of medications [9].
Figure 3: Enlarged Cerebral Ventricles in Schizophrenia
</style>
The hippocampus, the brain structure involved with storing new memories, is also a focus in schizophrenia research. Studies have demonstrated the hippocampus being smaller in individuals with schizophrenia and their first degree relatives compared to control participants without a family history of schizophrenia [15].
Additionally, it has been noted that individuals with schizophrenia have reduced brain asymmetry. Brain functions tend to be lateralized, as visual functions are primarily concentrated on the right hemisphere of the brain whereas language is concentrated on the left hemisphere (crow). Individuals with schizophrenia are lacking this lateralization, which results in them being ambidextrous [23].
Brain Activity
Hypofrontality of the brain regions with increasing brain activity towards the back of the brain has been noted in individuals with schizophrenia. Pruning is known as the elimination of excess neural connections and a normal part of maturation from birth is the pruning of unneeded connections from birth [1]. However it has been noted that excessive pruning takes place during the adolescent periods in individuals developing schizophrenia – excessive neural connections in the frontal regions of the brain are eliminated [4].
In addition, EEG analysis have revealed beta waves in the temporal regions of the brain and delta waves in the frontal lobes. Beta waves are associated with alertness and as there are more beta waves in the temporal regions, this reflects the symptomatology of auditory hallucinations. The temporal area is where the auditory cortex resides and the beta activity in the temporal lobes supports the presentation of these auditory symptoms [11]. Delta waves are present in the slow waves during our sleep state. Lower levels of activity are associated with delta waves and hypofrontality is reflected through the presence of delta waves in the frontal lobes. Frontal lobes are responsible for executive functions such as planning. Thus, the decreased level of activity in the frontal lobes reflects the reduced ability to perform executive functions [11].
Viral Agents
A high prevalence of antibodies within schizophrenia patients has been observed, emphasizing a possible role of viral agents in the pathogenesis of schizophrenia. Individuals with schizophrenia could have been exposed to viral agents early in life, likely in the womb [18]. Neurons through cell migration as the fetus develops. However if the mother catches a viral infection during the second trimester, the cell migration can be disrupted. Neurons are consequentially dispositioned and form abnormal neural communications [18].
Pathophysiology
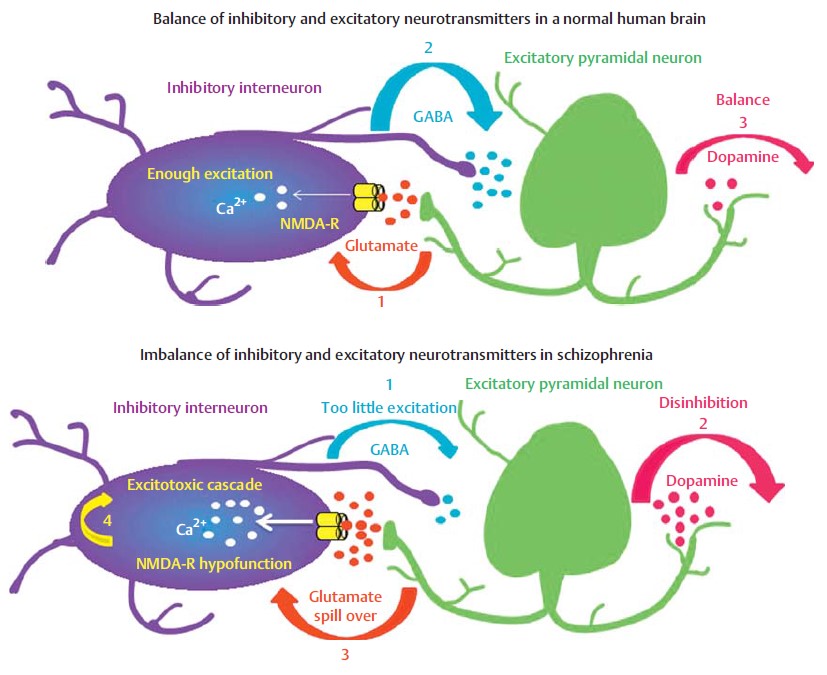
Normal Glutamate System
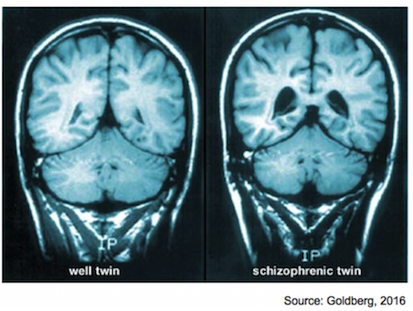
Figure 4: (Above) There is balanced excitation and inhibition between the pyramidal
neuron and inhibitory interneuron.
(Below) There is a lack of balance between
excitation and inhbition, resulting in the disinhibition of dopamine release [19].
</style>
Glutamate is a key excitatory neurotransmitter involved in neuronal migration, growth, synaptogenesis, and neuron pruning via apoptosis [19]. Additionally, glutamate in the hippocampus is involved in long-term potentiation, a pivotal process in learning and long-term memory [19]. The receptors involved in this process are the ionotropic glutamate receptors, amino-3-hydroxy-5-methyl-isoxazoloe-4-proprionic acid (AMPA) and N-methyl-D-aspartate (NMDA) [19]. Upon glutamate binding, the AMPA receptors are activated and allow mainly Na+ ions to flow down their gradients (inwards) [19]. When the pre-synaptic neuron receives high-frequency stimulation via action potentials, an increased amount of glutamate is released into the synaptic cleft [19]. This increased amount of glutamate allows for a large influx of positive ions, which then interacts with an Mg2+ ion that normally blocks the NMDA channel pore at rest [19]. This interaction between positive ions results in the repulsion of the Mg2+ block, allowing Na+ and Ca2+ ions to flow freely through the NMDA receptor as well [19].
Under these normal conditions, there is sufficient excitation of the post-synaptic cell (inhibitory interneurons) resulting in the release of the inhibitory neurotransmitter gamma-Aminobutyric acid (GABA) [19]. This GABA allows the inhibitory interneuron to modulate the activity of the pre-synaptic cell (the excitatory neuron, or pyramidal neuron) [19]. This pyramidal neuron is also involved in releasing dopamine, the “pleasure neurotransmitter”, to other cells in the hippocampus [19]. This modulation allows the pyramidal cell to release balanced amounts of dopamine and glutamate to interacting neurons [19].
Abnormal Glutamate System
High-frequency action potentials stimulate the pyramidal neurons as normal, resulting in glutamate release towards the inhibitory interneuron [19]. Glutamate then binds to AMPA receptors as normal, and there is a large Na+ influx. However, at this point because of a defective NMDA receptor (nondefinitive cause), there is an insufficient Ca2+ influx, which in term results in an insufficient depolarization of the inhibitory interneuron [19]. As a result, there is an insufficient GABA release to the pyramidal cells, and there is inhibition of the dopamine pathway [19]. This excessive dopamine is involved in the presentation of classic schizophrenic symptoms. Additionally, because there is still excessive glutamate in the synaptic cleft between the pyramidal neuron and interneuron, resulting in the overexcitation of AMPA receptors, leading to the activation of excitotoxic cascades and cell death [19].
Treatments
Antipsychotic Medication
Antipsychotics are often the first line of treatment prescribed to those affected with schizophrenia. Antipsychotics are used to alleviate positive symptoms associated with schizophrenia. There are two subtypes of antipsychotics available; typical and atypical.
- Typical Antipsychotics
- Also known as neuroleptics and conventional antipsychotics induce the slowing of psychomotor processes, and are helpful for managing emotions. Typical antipsychotics were first developed in the 1950s. They exert their effect by blocking receptors in the dopamine pathway. In schizophrenia, there is an excess production of dopamine resulting in damage to the mesocortical and mesolimbic pathways.
- The mesocortical pathway is responsible for pleasure, motivation and social skills. Damage to these pathways results in the positive symptoms associated with schizophrenia. The mesolimbic pathway is responsible for speech and understanding reality and damage to this pathway leads to the negative symptoms associated with schizophrenia. A downside to typical antipsychotics is that they induce extrapyramidal side effects (EPS). EPS include involuntary motor tremors, continuous muscle spasms and tardive dyskinesia [9] .
- Atypical Antipsychotics
- Also known as second generation antipsychotics have recently found to be more effective in alleviating schizophrenia symptoms. Similar to typical antispychotics, they bind to dopamine receptor resulting in dopamine blockade. However, unlike typical antipsychotics, atypical antipsychotics are also able to bind to serotonin receptors, inhibiting the production of excessive serotonin; responsible for the “mania-like” symptoms of Schizophrenia, allowing them to reduce both negative and positive symptoms.
- In addition, atypical antipsychotics also have a lower incidence of EPS. The most commonly prescribed atypical antipsychotic is clozapine [9] .
Therapy
To combat a decrease in social skills and the lack of motivation that many people affected with schizophrenia face, physicians often encourage patients to seek out therapy as part of their treatment. Different types of therapy include: individual ++psychotherapy|or cognitive behavioral therapy (CBT)++, family therapy and group therapy [9] .
Electroconvulsive Therapy
Physicians often recommend electroconvulsive therapy to patients whom display symptoms of depression and anxiety. Research has shown that electroconvulsive therapy (ECT) is most effective at alleviating symptoms of ++catatonia|moments when individuals cannot speak or appear to be motionless++. Research has indicated that ECT is most effective when used in combination with antipsychotics. During ECT, the patient is given an anesthetic and an electric current is given to the patient under the scalp to produce a seizure while they are asleep. Depending on the severity of the symptoms ECTs are administered anywhere between 3-15 times [9] .
Conclusion
Schizophrenia is a severe mental illness that can be extremely debilitating. There is a false notion that schizophrenia is a 'rare' disorder; however, it affects 1 in 100 individuals across the globe. The actual cause of this illness is unknown, however, there are numerous theories which have been tested and studied in great detail. The most promising theory is based on the assumption of brain activity imbalances and chemical changes due to the interacting roles of numerous factors such as genetics and the environment.
Even though there is no cure for this disorder, treatment is crucial. Antipsychotics are often recommended to treat certain symptoms such as hallucinations. Unfortunately, they can produce severe and unpleasant side-effects; therefore, given regimens can be hard to follow. Cognitive therapy has proven to be more successful in terms of treating schizophrenia, especially with regards to maintaining relationships, as well as managing stressful stimuli, emotions, and thoughts.
References
[1] Andreasen, Nancy C., et al. “Hypofrontality in schizophrenia: distributed dysfunctional circuits in neuroleptic-naive patients.” The Lancet 349.9067 (1997): 1730-1734.
[2] Andreasen, Nancy C., et al. “Magnetic resonance imaging of the brain in schizophrenia: the pathophysiologic significance of structural abnormalities.” Archives of General Psychiatry 47.1 (1990): 35-44.
[3] Carlton University. (2016, March 3). Neuroscience – Long-term Potentiation [Video file]. Retrieved from https://www.youtube.com/watch?v=vso9jgfpI_c
[4] Chechik, Gal, Isaac Meilijson, and Eytan Ruppin. “Neuronal regulation: A mechanism for synaptic pruning during brain maturation.” Neural Computation 11.8 (1999): 2061-2080.
[5] Coyle, J. T. (1996). The glutamatergic dysfunction hypothesis for schizophrenia. Harvard review of psychiatry, 3(5), 241-253.
[6] Crow, T. J., D. J. Done, and A. Sacker. “Cerebral lateralization is delayed in children who later develop schizophrenia.” Schizophrenia research 22.3 (1996): 181-185.
[7] Harrison, Paul J. “The neuropathology of schizophrenia.” Brain 122.4 (1999): 593-624.
[8] Messias, E. L., Chen, C., & Eaton, W. W. (2007). Epidemiology of Schizophrenia: Review of Findings and Myths. Psychiatric Clinics of North America, 30(3), 323-338.
[9]Miyamoto, S, Duncan G, Marx C, and Lieberman J. “Treatments for schizophrenia: a critical review of pharmacology and mechanisms of antipsychotic drugs.” Molecular Psychiatry. (2005): 79-104.
[10] Pantelis, Christos, et al. “Neuroanatomical abnormalities before and after onset of psychosis: a cross-sectional and longitudinal MRI comparison.” The Lancet 361.9354 (2003): 281-288.
[11] Paulman, Ronald G., et al. “Hypofrontality and cognitive impairment in schizophrenia: dynamic single-photon tomography and neuropsychological assessment of schizophrenic brain function.” Biological psychiatry 27.4 (1990): 377-399.
[12] Rosenthal, Randall, and Llewellyn B. Bigelow. “Quantitative brain measurements in chronic schizophrenia.” The British Journal of Psychiatry121.562 (1972): 259-264.
[13] Schizophrenia - Canadian Mental Health Association. (n.d.). Retrieved March 08, 2016, from https://www.cmha.ca/mental-health/understanding-mental-illness/schizophrenia/
[14] Schizophrenia Slideshow: How Schizophrenia Affects Thoughts, Behavior, and More. (n.d.). Retrieved March 08, 2016, from http://www.webmd.com/schizophrenia/ss/slideshow-schizophrenia-overview
[15] Seidman, Larry J., et al. “Thalamic and amygdala–hippocampal volume reductions in first-degree relatives of patients with schizophrenia: an MRI-based morphometric analysis.” Biological psychiatry 46.7 (1999): 941-954.
[16] Sharma, Tonmoy, et al. “Brain changes in schizophrenia. Volumetric MRI study of families multiply affected with schizophrenia–the Maudsley Family Study 5.” The British Journal of Psychiatry 173.2 (1998): 132-138.
[17] Strelets, V. B., V. Y. Novototsky-Vlasov, and J. V. Golikova. “Cortical connectivity in high frequency beta-rhythm in schizophrenics with positive and negative symptoms.” International Journal of Psychophysiology 44.2 (2002): 101-115.
[18] Torrey, E. Fuller, and Michael R. Peterson. “The viral hypothesis of schizophrenia.” Schizophrenia Bulletin 2.1 (1976): 136.
[19] Tsuang, M. (2000). Schizophrenia: Genes and environment. Biological Psychiatry, 47(3), 210-220.
[20] Veerman, S. R. T., Schulte, P. F. J., Begemann, M. J. H., Engelsbel, F., & de Haan, L. (2014). The Glutamate Hypothesis: A Pathogenic Pathway from which Pharmacological Interventions have Emerged. Pharmacopsychiatry, 47, 121-130.
[21] Watson, Charles G., et al. “Schizophrenic birth seasonality in relation to the incidence of infectious diseases and temperature extremes.” Archives of General Psychiatry 41.1 (1984): 85.
[22] Weinberger, Daniel R., et al. “Lateral cerebral ventricular enlargement in chronic schizophrenia.” Archives of General Psychiatry 36.7 (1979): 735.
[23] Wright, Ian C., et al. “Meta-analysis of regional brain volumes in schizophrenia.” American Journal of Psychiatry (2000).