Table of Contents
Presentation Link: https://docs.google.com/presentation/d/1JTOyofzyonkOJB61Z4LkGVThkePZB4uRO4ffWTzTRkY/edit#slide=id.gc6f90357f_0_0
The Effects of Exercise on Cardiovascular Function

Introduction
Exercise training and high levels of physical activity have many health benefits, and physical inactivity becomes a risk factor for cardiovascular diseases based on changes in blood lipids, hypertension, diabetes and other diseases (Joyner and Green, 2009). Furthermore, physical exercise reduces the effects of pathological conditions such as arterial hypertension, coronary artery disease, atherosclerosis. This can be done by altering the autonomic nervous system, which is correlated with reduction of heart rate and blood pressure (Zanesco and Antunes, 2007).
The Electrical Conduction System of the Heart
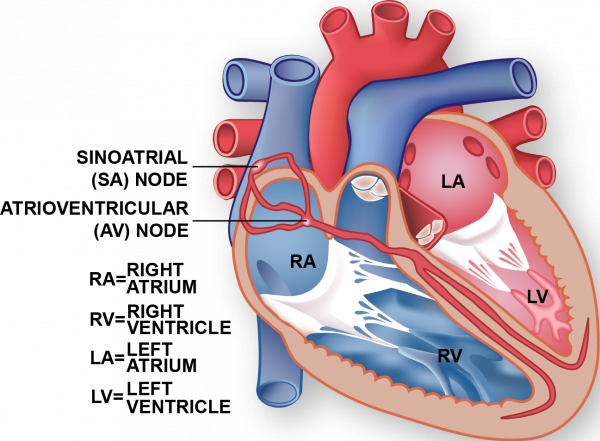
The cardiac electrical conduction system sets and maintains the rhythmic pumping action of the heart. The electrical impulses from the myocardium cause the heart to contract. The impulse begins at the sinoatrial (SA) node, which is found at the top of the right atrium. The electrical impulse form the SA node leads to the contraction of the atria, which signals the atrioventricular (AV) node. The impulse is then sent through the muscle fibres of the ventricles, cause the heart to contract. The cycle repeats (Cheng et al., 1999).
Adaptations of the Heart during Exercise
The heart’s mechanism of blood pumping drives adequate oxygen delivery to the muscles during exercise. Efficient delivery of oxygen and substrates for ATP production to cardiac and skeletal muscle is critical in meetings the metabolic demands of muscles necessary for exercise. During exercise, the demand for oxygen to the muscles is 15-25 times greater than demand at rest (Fu & Levine, 2013). Blood flow is redistributed to specifically target working muscles that are in greatest need of energy. Redistribution is facilitated through vessel constriction and dilation where vessels delivering blood to active muscle tissue will dilate and vessels to less active organs will constrict. To supply excess oxygen during exercise, cardiac output i.e. the amount of blood pumped through the circulatory system per minute, must be increased greatly. In the same way, there is also higher demand for removal of excess carbon dioxide and waste products from the muscles during exercise through the circulatory system back to the heart (Evans, 1985).
Heart Rate Changes
 The need for increased cardiac output during exercise drives the significant increase in heart rate during exercise. During exercise, heart rate first increases then plateaus at the elevated level as you sustain the same exercise pace. During strenuous exercise, heart rate increases to about 90% of their maximum values. Heart rate plateaus when the muscles are receiving an adequate flow of oxygen to meet the metabolic demands of the exercising muscles. Cardiovascular function is the limiting factor for oxygen delivery. Oxygen utilization by the body cannot exceed the rate at which the circulatory system transports oxygen to the muscles (Burton, Stokes, & Hall, 2004).
The need for increased cardiac output during exercise drives the significant increase in heart rate during exercise. During exercise, heart rate first increases then plateaus at the elevated level as you sustain the same exercise pace. During strenuous exercise, heart rate increases to about 90% of their maximum values. Heart rate plateaus when the muscles are receiving an adequate flow of oxygen to meet the metabolic demands of the exercising muscles. Cardiovascular function is the limiting factor for oxygen delivery. Oxygen utilization by the body cannot exceed the rate at which the circulatory system transports oxygen to the muscles (Burton, Stokes, & Hall, 2004).
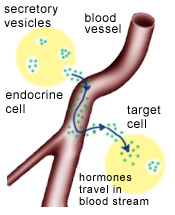
Role of Nervous System in Heart Rate Changes
The peripheral nervous system, specifically the autonomic nervous system, controls cardiac muscle contraction. Heart rate is increased when the sympathetic nervous system releases hormones epinephrine and norepinephrine. The resultant innervation from the sympathetic nervous system causes an increase in the rate of spontaneous depolarization of the pacemaker cells. As an integral part of the heart’s electrical conduction system, pacemaker cells set heart rate and rhythm (Scott, 2018).
Heart Rate Differences by Gender and Age
Heart rate responds differently to exercise based on gender and age. Men’s heart rate tends to rise more dramatically toward peak levels during exercise and return to resting levels after exercise more quickly than women. Men’s maximum heart rate is expected to be 200 minus 93% of their age. Women’s maximum heart rate is expected to be 200 minus 67% of their age. Furthermore, peak heart rate declines with age but the decline is more rapid in men (“The Heart Responds Differently to Exercise in Men vs. Women,” n.d.).
Effects on Blood Pressure
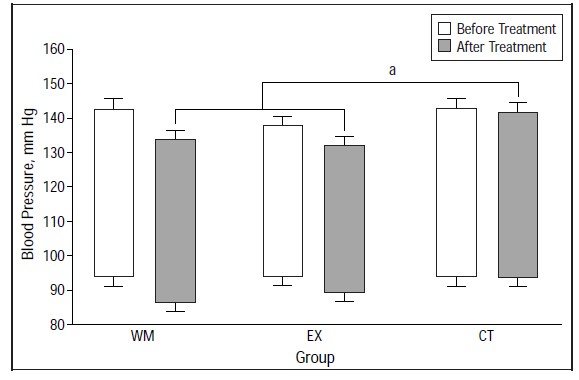
Blood pressure has been deemed as a risk factor for cardiovascular disease for several decades. However, aerobic exercise has been shown to mitigate this risk. In fact, aerobic exercise has been shown to decrease ambulatory blood pressure in individuals (Brownley, West, Hinderliter, & Light, 1996). This can be seen in the figure above. In the graph, blood pressure at work (usually higher due to a variety of stressors at the workplace) shows greater reduction in blood pressure than at home. This is because the work segment of the day is usually shortly after morning exercise whereas the home segment is usually several hours later. In the study, exercise was shown to decrease blood pressure 2-5 hours post exercise after which the effects start to diminish (Brownley et al., 1996).
Furthermore, several studies have found varying levels of reduction in blood pressure. One particular study has shown that exercise can reduce blood pressure by 4 mm Hg (Blumenthal et al., 2000). This is depicted in the above figure. The bars on the left (exercise + diet) show the greatest reduction in blood pressure however, the bars in the middle show that exercise alone is also sufficient in reducing blood pressure.
Effects on Cardiac Output
The heart, like any muscle, can grow with exercise since it is required to perform at a high level during such activity. The growth of cardiac muscle and simultaneous thickening of ventricular walls has been shown to lead to increased overall perfusion (Burton, Stokes, & Hall, 2004). Additionally, blood returns to the heart using skeletal muscles (which perform better with exercise). Therefore, exercise allows for greater smoothness of the venous blood flow which allows more blood to return to the heart (Lee & Oh, 2016). This allows the heart to pump more blood with each contraction. Higher levels of cardiac output also increase exercise capacity since trained athletes can show up to 40L greater cardiac output than untrained individuals (Lee & Oh, 2016). Lastly, with exercise the heart is able to undergo angiogenesis/coronary collateralization (Gertz et al., 2006). This essentially means that additional vessels are grown and perfuse the heart much better which allows for better cardiac function. Specifically, this increases overall perfusion as well as cerebral blood flow which has been shown to improve long-term stroke outcomes (Gertz et al., 2006).
Epicardial Fat
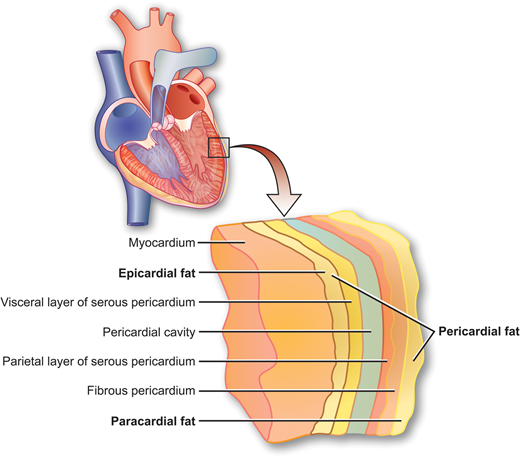
Epicardial fat is a build up of triglycerides usually located between the myocardium, also known as the muscular tissue of the heart, and the pericardium, which is the sac that encloses the heart (Bertaso, Bertol, Duncan & Foppa, 2013). This area does not typically contain large amounts of triglycerides. Consequently, when there is a large build up of epicardial fat it may lead to issues such as high blood pressure, coronary atherosclerosis, obesity and diabetes mellitus, among other problems (Bertaso et al., 2013). Thus, epicardial fat is often used as a key marker for cardiovascular risk. In addition, there are a variety of factors that affect the amount of epicardial fat such as age, gender, and ethnicity (Bertaso et al., 2013).
Epicardial Fat & Atherosclerosis
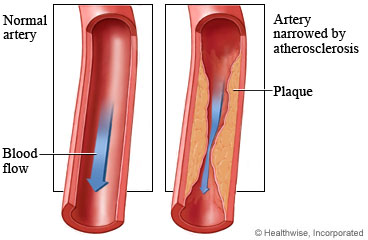
Epicardial fat may instigate many different diseases cardiovascular diseases, such as atherosclerosis.This is a disease in which plaque deposits in the arteries. In the long-term these plaque deposits harden, and actually narrow the arteries (“Atherosclerosis”, 2018). This narrowing is quite dangerous because it makes it difficult for oxygen-rich blood, which moves through arteries, to reach vital organs in the human body. The epicardial fat and coronary vessels are quite close to each other (Gleeson et al., 2011). This allows for fatty acids and adipokines to seamlessly move between adipose tissue and the arteries. In addition, this build-up may lead to other issues such as lipotoxicity, which can lead to cell death (Golbidi & Laher, 2012).
Effects of Exercise on Epicardial Fat
Exercise has been shown to reduce epicardial fat. A study was conducted to understand if aerobic exercises alone, without a significant alteration in diet would reduce ventricular epicardial fat. Participants completed a twelve week program in which they performed aerobic exercises, and their diet remained the same (Kim et al., 2009). These aerobic exercises were based on the participant’s maximum heart rate, and increased over time. For example, during week 1 the participants were doing exercises meant to reach 50-60% of their maximal heart rate, and by week 4, this number increased to 60-70% (Kim et al., 2009). These exercises included running and simple stretches. After the program, epicardial fat of participants was measured using an echocardiogram. It had decreased from 8.11 mm before exercise to 7.39 mm after exercise, a change of approximately 8.61%, which researchers determined was significant (Kim et al., 2009). Furthermore, there was also a decrease in the visceral adipose tissue (VAT).
Anti-inflammatory effects of exercise
Moreover, exercise has been shown to promote anti-inflammatory effects and thus reduce the risk of cardiovascular diseases. There are various possible different pathways in which exercise can produce anti-inflammatory effects. When an individual is exercising, and for up to an hour after the exercise session is over, skeletal muscles may release interleukin 6 into the bloodstream from contracting muscle fibres (Gleeson et al., 2011). This release leads to the increase of interleukin 10 and interleukin 1 receptor antagonist, both of which are anti-inflammatory cytokines. These cytokines subsequently increase anti-inflammatory effects. Interleukin 10 also functions to impede the formation of pro-inflammatory cytokines, thus promoting an anti-inflammatory state in the human body (Gleeson et al., 2011). In addition, exercise has been shown to reduce proinflammatory monocytes in the blood, specifically CD14 and CD16. Studies have shown that patients suffering from various diseases have an increased number of CD14 and CD16 monocytes in their blood (Gleeson et al., 2011). However when patients engaged in exercise, the number of these monocytes decreased significantly in their blood. Researchers believe that this reduction is due to the rise in plasma cortisol levels which occur during exercise. Overall, the anti-inflammatory effects in the human may function by reducing visceral fat in the body as well as promoting an anti-inflammatory environment (Gleeson et al., 2011).
Most Effective Types of Exercises
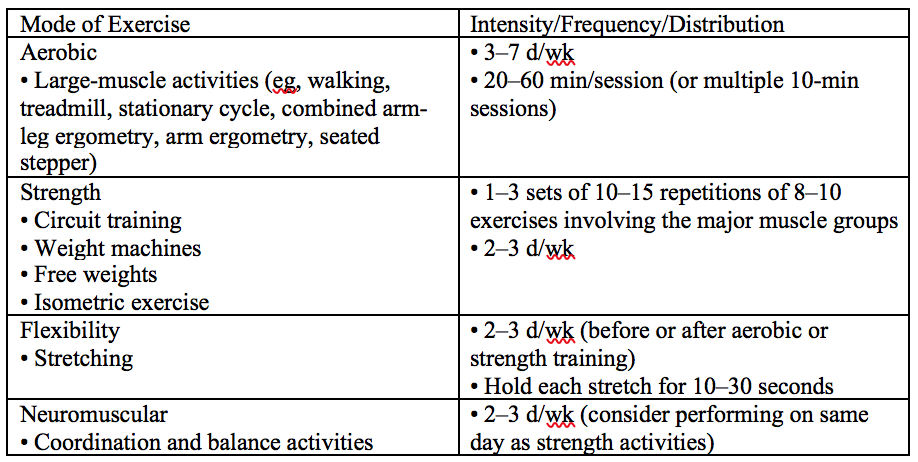
There are several exercises that are beneficial to maintaining healthy cardiovascular function. There are four types of exercises that are recommended for people who have suffered a stroke before (Gordon et al., 2004). These include any aerobic, strength, flexibility, and neuromuscular exercise. The key is to vary the intensity, frequency, and duration of each exercise depending on your age and health conditions. For stroke survivors, the intensity, frequency, and duration for each of the four types of exercises are summarized in the table below (Gordon et al., 2004).
The most recommended exercise was aerobic because that has the largest impact on the heart. Researchers stated that the treadmill is an excellent machine to use because stroke survivors can increase the incline of the treadmill while maintaining the same speed (Gordon et al., 2004). This function on the treadmill is very beneficial because some stroke survivors have difficult climbing stairs. By using the treadmill, the stroke survivors will gradually build up the strength to be able to climb stairs again. The other exercises are recommended for people who are able to do it in addition to aerobic exercises. These exercises can help speed up the rehabilitation process by helping stroke survivors to strengthen muscles and maintain proper balance and posture.
Electrocardiogram (ECG)
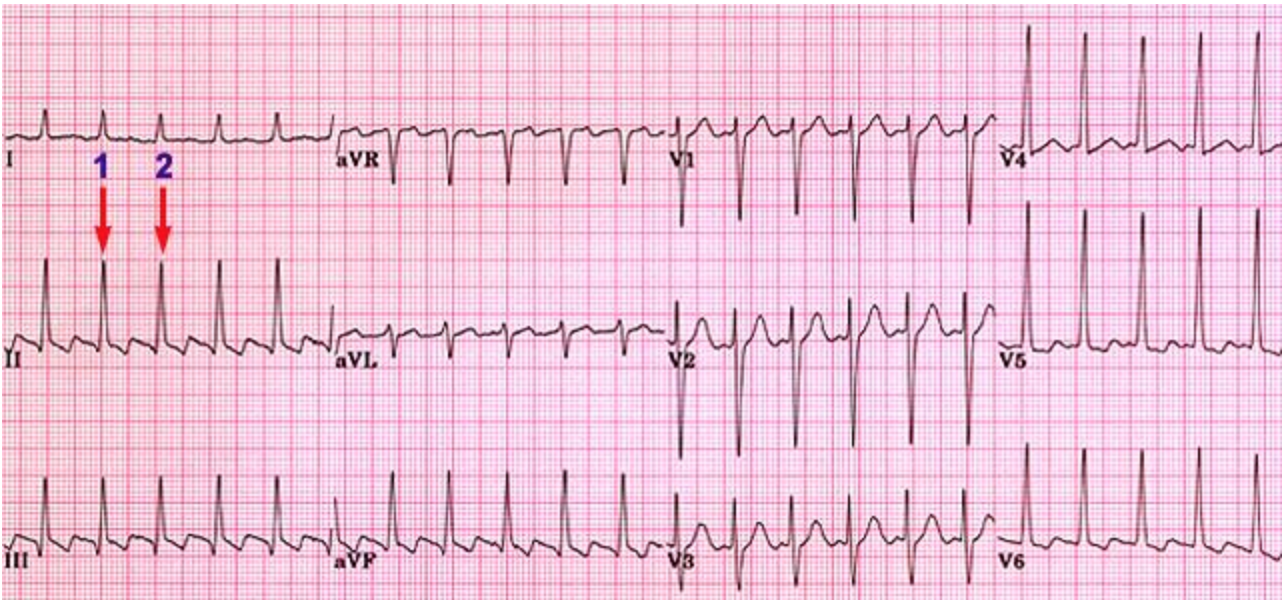
An ECG is a quick non-invasive test that is conducted to detect a patient’s risk of experiencing a heart problem (Adam Szulewski, n.d.). It is a common test that is given to many people that complain of chest pains or burning sensations around the area of the heart. Although it is a very simple and easy test to perform, it is very difficult to interpret the results and requires a lot of practice. One type of information that can be obtained through an ECG is a person’s heart rate (Adam Szulewiski, n.d.). The way to calculate the heart rate is to first locate two QRS complexes on the ECG. The QRS complex is the movement of electrical impulses through the lower chambers of the heart (Healthwise Staff, 2012).
The QRS complex in the ECG shown above is indicated by the two red arrows labelled 1 and 2. Now the distance between these two peaks is about 2 full box lengths. To obtain the heart rate, you simply divide 300 by the distance between the two peaks which is two. So, for this ECG the heart rate is approximately 150bpm.
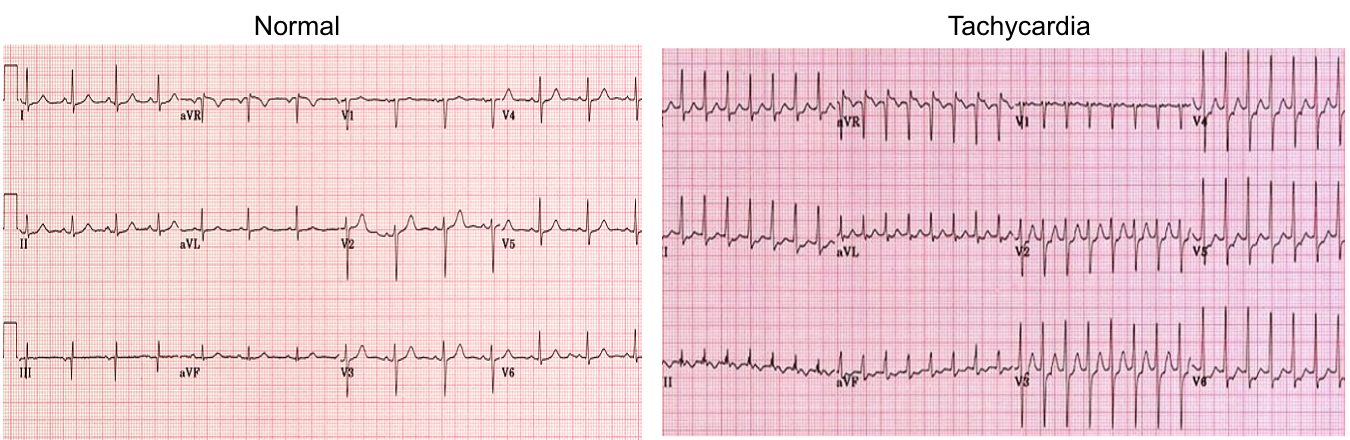
The two ECG images shown above indicate the differences between a resting heart rate and heart rate during exercise (Adam Szulewski, n.d.). The image on the left is what a normal ECG would look like for a healthy person at rest. You can see that the distance between two QRS complexes (peaks) is about 3.4 box lengths. So, the heart rate for this person would be approximately 88bpm. The actual number calculated by the author for this ECG is 82bpm (Adam Szulewski, n.d.). So, this quick method of measuring heart rate is very useful as the estimate is relatively close to the actual calculated value. On the right is an image of what an ECG looks like for tachycardia which means fast heart. This is what a person’s ECG would look like when they are exercising. The distance between the two QRS complexes (peaks) is approximately 1.8 box lengths which means the heart rate is approximately 166bpm.
How Exercise Prevents Different Cardiovascular Diseases
Diabetes
Exercise has both acute and chronic influences on patients with diabetes. Rapid changes in glucose concentration in blood occurs during and following an exercise. Type 2 diabetes are commonly comorbid with other cardiovascular diseases, and exercise can help with the improvement of insulin sensitivity as well as glucose disposal. Furthermore, exercise with diet can achieve weight loss, which can reduce the risk factor of diabetes (Chipkin et al., 2001).
Obesity
Exercise is helpful in controlling obesity. Patients with BMI above 31 are considered obese, and regular exercise at an intensity of about 50% of their maximum heart rate, 5 times/week for about one hour/session (such as walking) has the potential to normalize weight body composition. Exercise can also reduce abdominal visceral fat, which is associated with impairments in carbohydrate and lipid metabolism. Exercise is helpful in controlling the energy intake and increases resting metabolic rate (Bouchard et al., 1993).
Conclusion and Future Implications
In conclusion, exercise can improve a number of aspects of cognition and performance as well as prevention of cardiovascular disease such as coronary artery disease. Also, it can help control blood lipid abnormalities, diabetes and obesity. It would be important to come up with an effective exercise plan for patients with spinal cord injuries, the elderly or other conditions that may hinder an individual from practiing cardiovascular exercises.
Works Cited
Atherosclerosis. (2018). National Heart, Lung and Blood Institute. Retrieved from https://www.nhlbi.nih.gov/health-topics/atherosclerosis
Bertaso, A. G., Bertol, D., Duncan, B. B., & Foppa, M. (2013). Epicardial Fat: Definition, Measurements and Systematic Review of Main Outcomes. Arquivos Brasileiros De Cardiologia. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3998169/
Blumenthal, J. A., Sherwood, A., Gullette, E. C., Babyak, M., Waugh, R., Georgiades, A., … & Hayano, J. (2000). Exercise and weight loss reduce blood pressure in men and women with mild hypertension: effects on cardiovascular, metabolic, and hemodynamic functioning. Archives of internal medicine, 160(13), 1947-1958.
Bouchard, C., Depres, J., & Tremblay, A. (1993). Exercise and Obesity. Obesity Research,1(2), 133-147. doi:10.1002/j.1550-8528.1993.tb00603.x
Brownley, K. A., West, S. G., Hinderliter, A. L., & Light, K. C. (1996). Acute aerobic exercise reduces ambulatory blood pressure in borderline hypertensive men and women. American journal of hypertension, 9(3), 200-206.
Burton, D. A., Stokes, K., & Hall, G. M. (2004). Physiological effects of exercise. Continuing Education in Anaesthesia Critical Care & Pain, 4(6), 185–188. https://doi.org/10.1093/bjaceaccp/mkh050
Cheng, G., Litchenberg, W., Cole, G., Mikawa, T., Thompson, R., & Gourdie, R. (1999). Development of the cardiac conduction system involves recruitment within a multipotent cardiomyogenic lineage. Development,126, 5061-5049. Retrieved from http://dev.biologists.org/content/126/22/5041.short
Chipkin, S. R., Klugh, S. A., & Chasan-Taber, L. (2001). Exercise and diabetes. Cardiology Clinics,19(3).
Evans, D. L. (1985). Cardiovascular adaptations to exercise and training. The Veterinary Clinics of North America. Equine Practice, 1(3), 513–531.
Fletcher, G. F., Balady, G., Blair, S. N., Blumenthal, J., Caspersen, C., Chaitman, B., . . . Pollock, M. L. (1996). Statement on Exercise: Benefits and Recommendations for Physical Activity Programs for All Americans. Circulation,94(4), 857-862. doi:10.1161/01.cir.94.4.857
Fu, Q., & Levine, B. D. (2013). Exercise and the autonomic nervous system. Handbook of Clinical Neurology, 117, 147–160. https://doi.org/10.1016/B978-0-444-53491-0.00013-4
Gertz, K., Priller, J., Kronenberg, G., Fink, K. B., Winter, B., Schröck, H., … & Dirnagl, U. (2006). Physical activity improves long-term stroke outcome via endothelial nitric oxide synthase–dependent augmentation of neovascularization and cerebral blood flow. Circulation research, 99(10), 1132-1140.
Gleeson, M., Bishop, N., Stensel, D.J., Lindley, M.R., Sarabjit, S., Nimmo, M.A. (2014). The Anti-Inflammatory Effects of Exercise: Mechanisms and Implications for the Prevention of Common Diseases. Rheumatology, 53. Retrieved from http://www.nature.com/articles/nri3041
Golbidi, S., Laher, I. (2012). Exercise and the Cardiovascular System. Cardiol Res Pract. 2012, 210852. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3371347/
Gordon, N. F., Gulanick, M., Costa, F., Fletcher, G., Franklin, B. A., Roth, E. J., & Shephard, T. (2004). Physical activity and exercise recommendations for stroke survivors: an American Heart Association scientific statement from the Council on Clinical Cardiology, Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention; the Council on Cardiovascular Nursing; the Council on Nutrition, Physical Activity, and Metabolism; and the Stroke Council. Stroke, 35(5), 1230-1240.
Joyner, M. J., & Green, D. J. (2009). Exercise protects the cardiovascular system: Effects beyond traditional risk factors. The Journal of Physiology, 587(23), 5551-5558. doi:10.1113/jphysiol.2009.179432
Kim, M., Tomita, T., Kim, M., Sasai, H., Maeda, S., & Tanaka, K. (2009). Aerobic exercise training reduces epicardial fat in obese men. Journal of Applied Physiology, 106(1), 5-11. Retrieved from https://www.physiology.org/doi/abs/10.1152/japplphysiol.90756.2008?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub=pubmed.
Lee, B. A., & Oh, D. J. (2016). The effects of long-term aerobic exercise on cardiac structure, stroke volume of the left ventricle, and cardiac output. Journal of exercise rehabilitation, 12(1), 37.
The Heart Responds Differently to Exercise in Men vs. Women. (n.d.). Retrieved October 8, 2018, from http%3a%2f%2fwww.acc.org%2fabout-acc%2fpress-releases%2f2014%2f03%2f27%2f12%2f29%2fallison-peak-hr-pr
Scott, G. Regulation of the heart [PDF document]. Retrieved from Lecture Notes Online Web site: https://avenue.cllmcmaster.ca/d2l/le/content/229910/viewContent/1974510/View
Staff, H. (2012, March 6). Exercise Electrocardiogram. Retrieved October 31, 2018, from https://www.cardiosmart.org/Healthwise/hw23/4760/hw234760
Szulewski, A. (n.d.). Analysis and Interpretation of the Electrocardiogram. Retrieved October 30, 2018, from https://meds.queensu.ca/central/assets/modules/ts-ecg/index.html
Zanesco, A., & Antunes, E. (2007). Effects of exercise training on the cardiovascular system: Pharmacological approaches. Pharmacology & Therapeutics,114(3), 307-317. doi:10.1016/j.pharmthera.2007.03.010