This is an old revision of the document!
Table of Contents
Origin and Background
In 1906, a German psychiatrist and neuropathologist by the name of Alois Alzheimer was drawn to the case of a woman showing unusual symptoms. Post mortem analysis of the brain tissue of the woman, started the journey of Dr. Alzheimer’s description of the neurodegenerative disease (Hippius, 2013). Alzheimer disease is an incurable disorder of cognitive and behavioural impairment with a long and progressive timeline. 75% of patients with dementia are thought to have genetically based Alzheimer’s, however the incidence can also be sporadic (Chapman et al, 2006). In Alzheimer’s, misfolded amino acid aggregates known as plaques develop in brain areas and impact and impede neuronal communication causing brain cell atrophy. This neurodegeneration begins in the hippocampus, then spreads to the rest of the brain over time and increasing severity of the disease. The affected region of the brain is the reduction of the memory encoding hippocampus, along with associated regions of the cerebral cortex involved in thinking, decision making, and planning (Purohit et al, 1998)
Symptoms
At first, language, strength, reflexes, sensory capacities and motor skills are spared. Memory loss increases as the disease progresses, often leading to confusion. Cognitive abilities such as problem solving, language, calculation and visuospatial skills are compromised with progression of the disease (Kandel et al, 2013). Due to the loss of cognitive abilities, experiencing psychotic symptoms are common such as hallucinations and delusions. Mental functions and the ability to carry out usual daily activities become impaired (Kandel et al, 2013). The late stages of Alzheimer's are related to becoming mute, loss of autonomic functions and eventually becoming bedridden, relying completely on a caregiver (Kandel et al, 2013). Because shrinkage of the amygdala is also a hallmark of Alzheimer’s, it is associated with mood changes.
Epidemiology
46 million people live with dementia worldwide, and most of these cases are attributed to Alzheimer’s disease. This number is expected to increase due to the elderly being the most rapidly growing portion of Canada and US populations (Abbott, 2011). As the population ages, Alzheimer’s disease is expected to become increasingly prevalent. Within the next 25 years, the number of people with Alzheimer’s disease in the US will triple (Kandel et al, 2013). It is important that enough research is being devoted to Alzheimer’s disease. Most funding is allocated to other research related to the main causes of death, but because the course of Alzheimer’s is between 7-10+ years whereas cancer for example is about 4 months, there are less deaths compared to cancer and this may be overridden (Leading causes of death, by sex (Both sexes), 2015). Due to the longer course, dementia and thus Alzheimer’s disease incurs more costs, even though there is not as much investment compared to other leading causes of death (Abbott, 2011).
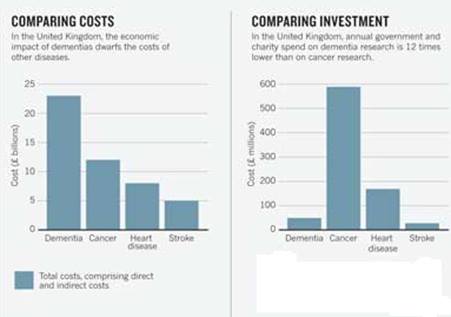 Figure 1:This figure shows a comparison cost and investment (Abott, 2011).
Figure 1:This figure shows a comparison cost and investment (Abott, 2011).
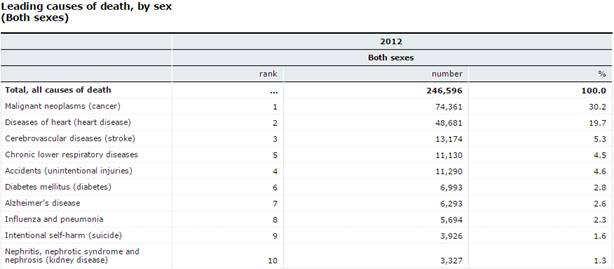 Figure 2:This figure shows the leading causes of death by sex (2015).
Figure 2:This figure shows the leading causes of death by sex (2015).
Symptoms
At first, language, strength, reflexes, sensory capacities and motor skills are spared. Memory loss increases as the disease progresses, often leading to confusion. Cognitive abilities such as problem solving, language, calculation and visuospatial skills are compromised with progression of the disease (Kandel et al, 2013). Due to the loss of cognitive abilities, experiencing psychotic symptoms are common such as hallucinations and delusions. Mental functions and the ability to carry out usual daily activities become impaired (Kandel et al, 2013). The late stages of Alzheimer's are related to becoming mute, loss of autonomic functions and eventually becoming bedridden, relying completely on a caregiver (Kandel et al, 2013). Because shrinkage of the amygdala is also a hallmark of Alzheimer’s, it is associated with mood changes.
Disease Progression
Mild: Patients with Alzheimer's may show physiological changes in the brain 10- 20 years prior to showing any symptoms. Shrinkage of the amygdala brings about symptoms of emotional outbursts and mood changes (Purohit et al, 1998)
Moderate: Memory loss at this stage advances to confusion of location in familiar places and poor judgement, mood changes, increased anxiety and language impairment (Hippius, 2013).
Severe: Plaques and tangles become widespread, memory loss advances to severe dementia and atrophy of other brain regions leads to progressive loss of autonomic functions (Hippius, 2013).
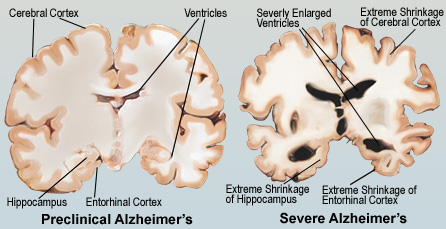 Figure 3:This figure illustrates the comparison between a pre-clinical and severe Alzheimer's brain.
Figure 3:This figure illustrates the comparison between a pre-clinical and severe Alzheimer's brain.
Etiology
Sporadic cases: The greatest risk factor for Alzheimer’s is aging, but Alzheimer’s is not a normal part of aging. The most common form of Alzheimer’s disease is called sporadic Alzheimer’s disease, meaning it has no specific family link (Understanding Genetics and Alzheimer's Disease, 2016). Sporadic Alzheimer’s is associated with late-onset Alzheimer’s disease, which includes individuals older than 60 years of age. A certain form of a protein called apolipoprotein E (ApoE), has been found to increase the risk for sporadic Alzheimer’s (Kandel et al, 2013). The specific allele of the ApoE gene is ApoE4. This gene is expressed as three alleles, ApoE2, ApoE3, and ApoE4 (Kandel et al, 2013). The normal function of the ApoE protein is to carry cholesterol and other lipids in the blood. It also plays a fundamental role in the maintenance and repair of neurons, and it binds amyloid beta (Mahley, 2006). However, isoforms may bind amyloid beta differently, which may influence aggregation, deposition and clearance of amyloid beta (Kandel et al, 2013). In this case, ApoE4 is the poorest at binding to and clearing amyloid beta from the bloodstream, so amyloid beta continues to aggregate and the cascade of events, including neuronal injury, follows (Kandel et al, 2013). The exact mechanism through which ApoE4 works is unknown, but some studies have shown features of Alzheimer's pathology in transgenic mice expressing the human ApoE4 allele in neurons (Mahley, 2006). The features included reduced numbers of presynaptic terminals, increased phosphorylation of tau, increased plaque deposition and impaired learning and memory, found by testing mice in a water maze (Mahley, 2006).
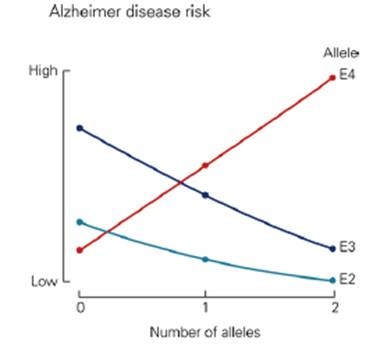 Figure 4:This graph shows the risk of developing Alzheimer's based on alleles.
Figure 4:This graph shows the risk of developing Alzheimer's based on alleles.
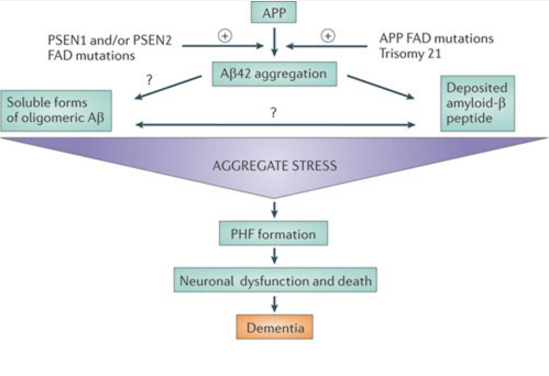
Familial Cases The familial, or inherited form of Alzheimer’s is associated with early-onset Alzheimer’s, which includes individuals 60 years of age or younger. Mutations in three genes are associated with this form of Alzheimer’s; APP, presinilin-1 and presinilin-2 (Kandel et al, 2013). The mutations influence the cleavage of APP, increasing the production of amyloid beta peptides, or increasing the ratio of the more toxic amyloid beta 42 kind. Some APP mutations are amino acid substitutions within the amyloid beta region (Kandel et al, 2013). Cells with this mutation secrete more amyloid beta peptides compared to wildtype APP. Another APP mutation influences gamma-secretase to selectively produce amyloid beta 42 instead of amyloid beta 40 (Kandel et al, 2013). The presinilin mutants are similar, as they produce mutant gamma-secretase as well, causing over activity of gamma-secretase, and again generating a higher ratio of amyloid beta 42 (Kanel et al, 2013). The mutations in APP or presinilin genes lead to a gain of function for overproducing amyloid beta 42.
Amyloid Hypothesis
Figure 4:This figure shows a simplification of the cascade of events that occur in Alzheimer's disease as predicted by the Amyloid Hypothesis. (Karran, 2011).