Table of Contents
Introduction
There is a positive correlation between adults who sleep 6-8 hours per night and their lifespan. Excessive sleep results in cardiovascular disease and diabetes whereas insufficient sleep can also cause cardiovascular disease, obesity and even brain damage. The physiology of sleep is categorized as non-rapid eye movement (NREM) sleep and rapid eye movement (REM) sleep. NREM sleep is divided into stages 1-4 with each stage representing its relative depth. Each sleep stage has unique characteristics including variations in brain wave patterns, eye movements and muscle tone. The cycles can be detected through electrical brain activity using an EEG. 1,2
Signals from the environment help play a role in why we sleep. Adenosine and melatonin are two hormones in the brain that encourage sleep. NREM sleep is when the body replenishes itself and DNA repair occurs. During a period of sleep, NREM and REM sleep alternate cyclically. The cycle between NREM and REM sleep is not clearly understood but irregular cycling or the absent of a stage is associated with sleep disorders. A sleep episode begins in the NREM stage and progresses from stage 1-4 and then further into REM sleep where dreams may occur. 1,2
What is Sleep Deprivation?
Sleep deprivation can occur in two ways. Total sleep deprivation is the complete lack of sleep while partial sleep deprivation is chronically having insufficient sleep or less than 6 hours of sleep a night. Chronic sleep deprivation will negatively impact cognitive performance by decreasing alertness, concentration, attention and vigilance. In addition, it will also impair memory, executive functions and psychomotor skills. 3,4
What Happens when we don't sleep?
After the first sleepless night, mesolimbic system becomes stimulated and dopamine is overexpressed. This may result in a slightly increase of energy, mood or sex drive. However, the portions of the brain that is responsible for planning and evaluating decisions may become inactive leading to impulsive behavior. In addition to impulsive behavior, reaction time, perception and cognitive functions are affected once exhaustion starts. After 2 days without sleep, the body’s ability to metabolize glucose is greatly reduced. Eventually, the continuing sleep deprivation whether it is total sleep deprivation or partial will lead to death. 3,4
Physiology of Glymphatic System (Glymphatic Clearance Pathway)
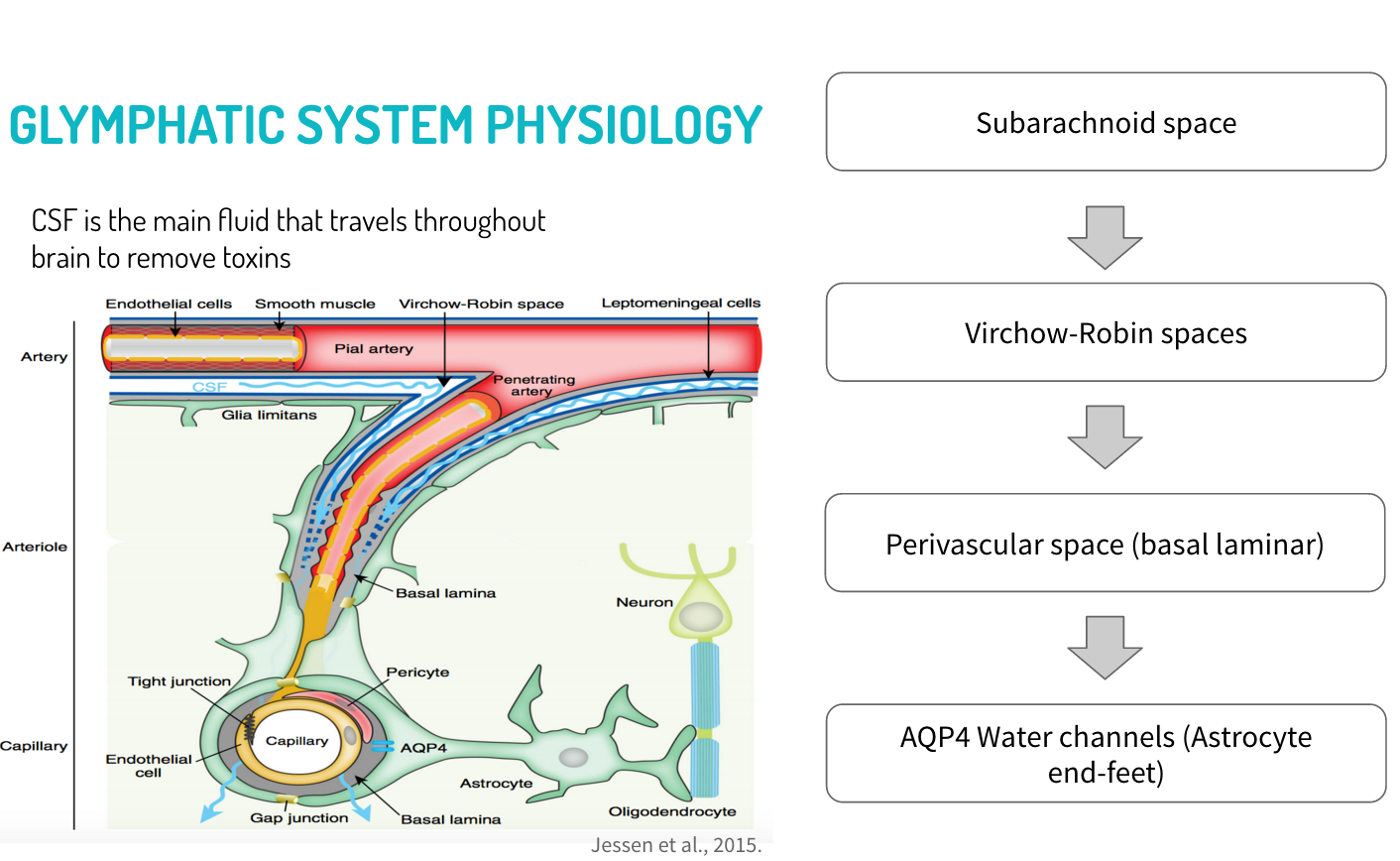
Scientists believe that the accumulation of waste products in the brain is the cause for the detrimental effects of sleep deprivation. During the waking hours, the cells of the human body are constantly metabolizing substrate in order to provide sufficient energy for daily activities. The body breaks down substances into byproducts including adenosine. As adenosine builds up, it increases the body’s urge to sleep. This is also known as sleep pressure. There are other waste products that build up within the brain. The accumulation of the waste products during our waking hours is linked to the negative consequences of sleep deprivation. Sleep is necessary in the removal process of waste accumulation in the brain. During the sleeping period, scientists discovered that there is a glymphatic system that removes waste products from the brain. This glympatic system uses cerebrospinal fluid (CSF) in order to remove toxins from the extracellular space of the brain. In addition to the discovery of the glymphatic system, scientists have also found lymphatic vessels that act as a pathway for immune cells in the brain. The lymphatic system removes toxins, waste products and other unwanted materials from the body. 5
Glymphatic system
The glymphatic system is a macroscopic waste clearance system that utilizes a system of perivascular tunnels formed by astroglial cells in order to remove soluble proteins and metabolites from the CNS. In addition to waste eliminiation, the glympatic system also plays a role in the distribution of brain compounds such as glucose, lipids, amino acids, neuromodulators and growth hormones. In the glympatic system, cerebrospinal fluid (CSF) and interstitial fluid (ISF) continuously interchange. This is facilitated by convective influx of CSF along the periarterial space. CSF is driven from the subarachnoid space into the Virchow-Robin spaces by a combination of arterial pulsatility, respiration, slow vasomotion and CSF pressure gradients. The CSF is then transported into the dense and complex brain parenchyma through AQP4 water channels that is expressed in a highly polarized manner in astrocytic end-feet that surround the brain vasculature. This movement drives convective interstitial fluid fluxes in the tissue towards the perivenous surrounding the large deep veins. The ISF collects in this perivenous space and then drains out of the brain towards the cervical lymphatic system. 5,6,7
The glymphatic system is suppressed during wakefulness but it is dramatically enhanced during sleep. This was likely a result of the sleep-wake difference in glymphatic influx that is correlated with the volume fraction of the interstitial space. The interstitial space expands from 13-15% in the awake state to 22-24% during the sleep state. This observation suggests that the sleep state is significant for the influx of ISF and CSF fluid, leading to an enhanced clearance of metabolites. The increase in volume of the interstitial space decreases tissue resistance, thus permitting convective flow and ISF-CSF exchange. 6,7
Causes of Sleep Deprivation
Alcohol/Drug Dependence
Research conducted by Irwin, Bjurstrom and Olmstead (2016) aimed to study the relationship between sleep and cocaine and alcohol use.8 In this study, the participants were individuals who has previously been dependent on these substances but were now in the early stages of abstinence.8 Polysomnographic sleep measures were recorded to determine sleep continuity, Stage 3 sleep and rapid eye movement (REM) sleep.8 In this study, sleep continuity included the total sleep time, sleep latency, which is the time required to transition from full wakefulness to sleep, sleep efficiency and wake sleep onset.8 Moreover, Stage 3 sleep was characterized by slow wave sleep (SWS), which consists of very slow delta waves in combination with smaller, faster waves in the brain.8 These measurements were then compared to the controls, which were patients that had no medical history of any mental illnesses or disorders.8 Although the results of the study indicated sleep continuity is not impacted by drug or alcohol use, the study did show that there was a decrease in Stage 3 sleep among both alcohol and cocaine-dependent patients.8 The results also indicate that loss of Stage 3 sleep occurs at an earlier age among the cocaine-dependent patients, in comparison to the alcohol-dependent patients.8 In addition, the amount of REM sleep increased among both groups of participants in comparison to the controls.8 Therefore, this study demonstrates that alcohol and cocaine have an impact on sleep disturbances.
Mental Disorders
Patients with schizophrenia often experience difficulty sleeping due to the fact that disturbances in sleep are characteristic of the first phase of a psychotic episode, known as the prodormal phase.9 More specifically, these patients either cannot fall asleep or cannot maintain sleep, waking up in at night or early in the morning.9 In addition, the severity of the illness is negatively correlated to the amount of rapid eye movement (REM) sleep patients with schizophrenia get.9 Therefore, depending on the severity of the disease, 30-80% of patients with schizophrenia suffer from sleep deprivation.9
Neurodegenerative Disease
Parkinson’s Disease (PD) is the second most common neurodegenerative disease in the world.10 The pathology of PD affects all parts of the brain and recently, it has been noted that this neurodegenerative disease results in changes in sleep.10 Research conducted by Christensen et al. (2016) has demonstrated that REM sleep is less stable in patients with PD. 10 Since sleep is regulated by mechanisms that include neurons located in the basal brain regions, this research suggests that PD affects these mechanisms and, thus, leads to disturbances in sleep.10 Furthermore, the lower stability of REM sleep in patients with PD can also be attributed to the neurodegenerative nature of this disease.10 More specially, neurodegeneration affects the pre-thalamic fibres in the brain stem, which in turn may impact the neuronal mechanisms of REM sleep.10
Sleeping Disorders
Obstructive Sleep Apnea
Obstructive sleep apnea is a sleeping disorder which is characterized by a complete stop or reduction of air flow during sleep.11 This can be attributed to the complete or partial collapse of the airway.11 Obstructive sleep apnea can significantly decrease the amount and quality of sleep an individual gets due to loud snoring and interruptions in breathing patterns.11 In addition, individuals may awake from their sleep as a result of gasping or choking due to a lack of air.11 These obstructive respiratory events can occur five times during every hour of sleep and therefore, can lead to characteristics of sleep deprivation such as increased daytime sleepiness.11
Insomnia
Insomnia is another sleeping disorder which can cause sleep deprivation since individuals who experience insomnia have difficulties falling asleep or maintaining a state of being asleep.12 Importantly, insomnia leads to effects that are commonly associated with sleep deprivation, such as daytime sleepiness and an inability to focus.12 In addition, insomnia may also lead to an increased risk of worsening mental disorders, such as depression and anxiety.12 Moreover, there are two types of insomnia which can be associated with sleep deprivation. Primary insomnia is associated with difficulty, falling asleep, awakening during the night and difficulty falling back asleep after awakening.12 Secondary insomnia, however, is associated with comorbidities, such as heart disease or other sleeping disorders.12 Insomnia can, therefore, lead to sleep deprivation, decreasing one’s quality of life and functionality.12
What Are The Effects of Sleep Deprivation?
Depression
It is known that those who are experiencing depression can have a very difficult time sleeping but the same does exist for the reverse. Chronic insomnia caused by sleep deprivation has the ability to cause psychiatric disorders, even depression, and is also a prodrome of major depressive episodes, which essentially is a detrimental result of depression that usually occurs past the clinical phases of depression and is also used to indicate long-term illness course and treatment responses.13 For those at risk of depression sleep is psychologically odd.13 This is shown with those who have shortened REM sleep latency is present not only during clinical episodes of depression, but also before the clinical episode in subjects at risk for depressive illness.13 Even though insomnia goes away after one’s depression is treated, there is a chance that it may continue and if this occurs this shows an increased vulnerability to depressive relapse or recurrence.13 The effects of depression on the changed of the mind have a strong relation with the chance of response to psychotherapy which can help determine which patients are likely or unlikely to have success with psychosocial treatments, thus in turn needed somatic therapy to preserve recovery.13 A close relationship between the regulation of sleep and the regulation of mood was discovered and was further highlighted through brain imaging studies of patients with depression undergoing sleep deprivation and normal sleep.13 During therapeutic sleep deprivation (TSD) it was discovered that TSD may serve as both a catalyst of rapid antidepressant activity and as a probe of treatment resistance.13 Essentially, TSD affects the brains metabolic rates, mainly in limbic areas, correlates to loss of sleep and anti-depressant medications.13
Diabetes
There is a greater risk of about 50-150% in contracting Type 2 diabetes for those who are sleep deprived.14 To begin with, obesity is heavily linked with Type 2 diabetes but it is evident that a lack of sleep may impair glucose metabolism which increases the chance of diabetes.14 Sleep deprivation can negatively impact one`s energy balance which can cause weight gain because of an upregulation of appetite, an increase in time to eat and a decline in energy output.14 If an excessive amount of weight is gained there is potential that insulin resistances may increase coupled with a loss in glucose tolerance, which is a condition that increases the risk of developing diabetes potentially causing more weight gain to occur.14 Glucose tolerance is the mechanism that links sleep deprivation and Type 2 diabetes.14 Further research was done to test the effects of sleep restriction on patients rather than patients who incurred sleep disorders.14 The results of the experiments were consistent with the initial hypothesis as sleep loss resulted in an upregulation of appetite and increased Body Mass Index (BMI).14 An increase level of sleepiness and fatigue coupled with a lower level of energy expenditure was also found due to the loss of glucose metabolism that occurred from the lack of sleep, thus justifying the linked causation of diabetes from sleep deprivation.14
Heart Disease
With heart disease there is a 2x increase risk of developing CVD and hypertension for those who are sleep deprived.15 Essentially a loss in sleep will result in an increase in blood pressure as well as a decrease in the sympathetic system (ANS).15 The sympathetic system is the mechanism that links sleep deprivation and heart disease.15 Also, stress hormones are regulated during sleep and with sleep being deprived this can cause a lot of harmful issues with the regulation of blood pressure.16 Sleeping for less than 5 hours on a consistent basis causes high blood pressure and if this occurs during sleep there is a potential risk of myocardial infarction.16 With these combined there is an increased risk of getting heart disease due to sleep deprivation.15
Psychopathological
Most of the psychopathological cases include schizophrenic like tendencies such as irritability, illusions, visual hallucinations and even paranoia.17 It was tested that some acute schizophrenic reactions were seemingly caused by sleep loss and that sleep-deprived subjects were more sensitive to the hallucinogenic effects of lysergic acid diethylamide (LSD a hallucinogen).17 These findings indicated that metabolic changes in this state can potentially require a biological setting that favours the development of the psychosis.17 Further research was done by Koranyi and Lehman (1960) to get more evidence to support this hypothesis by conducting an experiment on 6 sleep-deprived schizophrenic patients.17 After 72 hours, signs of progressive deterioration showed in all patients and for acute schizophrenic psychosis began to manifest again for 5 of the 6 patients, as they were being observed at the time they were admitted to the hospital.17
Research Study Findings
The Effects on Cognition
Frequently disrupted and restricted sleep is a common problem for many people in our modern around-the-clock society.20 Deficits in daytime performance due to sleep loss are experienced universally, and associated with significant effects on the human body. The first known study addressing the negative effects of sleep deprivation was published in the late 1800s. Since then, hundreds of studies have established that sleep loss impairs various cognitive functions and behaviours. Sleep deprivation studies repeatedly indicate a (variable) impact on mood, cognitive performance, and motor function due to destabilization of the body's wake state. It has been shown that specific neurocognitive domains including, executive attention, working memory, and higher cognitive functions (e.g. emotional intelligence and decision making), are particularly vulnerable to sleep loss.18 Recent chronic partial sleep deprivation studies, which more closely mimic the sleep loss experienced in society today, demonstrate that neurocognitive deficits are capable of accumulating over time, due to the body adapting or altering its response to the sensation of sleepiness.18
The Effects on the Neuroendocrine Stress Systems
Along with its effect on cognitive function, it is important to determine how sleep loss affects the stress systems of the body, since these are the systems that help individuals deal with everyday challenges. Sleep has a mild suppressive effect on the basal activity of the major autonomic neuroendocrine stress systems, i.e., the autonomic sympatho-adrenal system and the hypothalamic-pituitary-adrenal axis.20 Studies on both humans and rodents have shown that sleep deprivation raises the activity of these stress systems. The extent to which it raises the activity is dependent upon both the mental load (sensory input, thoughts, emotions) and physical activities (voluntary or forced) that the individual experiences following sleep deprivation. The activity of the stress systems most often rapidly returns to baseline during subsequent recovery sleep. However, if recovery sleep is insufficient, stress systems may display a mild recurrent activation the following day.20 Sleep deprivation may not only affect the basal activity of neuroendocrine systems, but in the long run, it may also affect the reactivity of these systems to new challenges and stressors. Ultimately, this will alter the way an individual responds to the new challenges and stressors. The first sign of this alteration in response, appears at the level of emotional perception. Though most of the effects of acute sleep deprivation on the neuroendocrine stress systems seem to be transient, chronic partial sleep deprivation studies in rodents show that too little sleep may gradually cause fundamental changes in the brain systems, that are involved in the regulation of stress responses.20 For example, chronic partial sleep deprivation can cause a reduction in the number or sensitivity of corticotropin releasing hormone receptors and serotonin receptors. Sleep restriction gradually changes these brain systems in a direction that is similar to what is seen in mood disorders such as depression. This data supports the idea that insufficient sleep, by acting on stress systems, may sensitize individuals to stress-related disorders. However, it is important to note that few controlled studies in humans have been completed, as such, further research in this area is required.20
The "All Nighter": Effects on Academic Performance
The relationship between sleep, memory and learning capacity is well-known. Sleep plays an important role in learning processes and memory consolidation, and studies clearly show that sleep deprivation can impair both.21 Due to this relationship, exploration of the effects of sleep deprivation on student learning ability and academic performance was inevitable. Most studies have been correlative investigations, where sleep schedules were correlated with school and academic achievement.21 For example, a study completed by Thacher19, assessed the correlation between engaging in a single night of total sleep deprivation (SN-TSD), and sleep schedule parameters, circadian preference, academic performance, and depressive symptoms. The study involved 120 university students, of a mean age of 20 years. Measures included the Owl-Lark Scale of circadian preference, the Beck Depression Inventory, Pittsburgh Sleep Quality Index (PSQI), as well as, self-reported usual bedtime, rise time, and total sleep time. Students' cumulative grade point averages (GPAs) were also obtained from the university registrar. Of the 120 students, 60% reported engaging in SN-TSD once or more since coming to university. Engagement in SN-TSD was found to be correlated with later self-reported bedtimes, evening preference, and poorer academic achievement as measured by GPA.19 Some studies, however, have been able to actively manipulate sleep in order to observe neurocognitive and behavioural consequences, such as learning, memory capacity and school performance. The findings from these studies strongly suggest that:
1. Students of different education levels (from school to university) are chronically sleep deprived or suffer from poor sleep quality.21
2. Sleep quality and quantity induce several effects on a student's life: increased day-time sleepiness, impaired mood, neurocognitive deficits, and behavioural changes.21
3. The effects of sleep loss are mainly evident on higher cognitive functions (attention, memory, problem-solving, etc.); as a result, learning capacity and academic performance may seriously be affected.21
One of the most crucial findings of these studies suggests that the negative effects of sleep deprivation can be reversed. Studies in which sleep was actively restricted or optimized showed, respectively, a worsening and an improvement in neurocognitive and academic performance. This indicates the possibility of an improvement in neurocognitive function (and thus of learning capacity and academic performance) as a result of healthy sleep schedules.21
Is it possible for sleep deprivation to be beneficial?
Major depressive disorder (MDD) is the leading cause for illness-related reduction of quality of life worldwide, and current first-line treatments show a long-latency (slow-acting) response. Therapeutic sleep deprivation (SD) is a fast-acting anti- depressant intervention that leads to a rapid decrease of depressive symptoms in 50-60% of patients with MDD. It has been shown to improve the clinical symptomatology that is related to impaired associative synaptic plasticity in MDD. However, the effect is temporary, only lasting until the next time the individual falls asleep.22
Neuronal plasticity or remodeling, is a fundamental process by which the brain acquires information and makes the appropriate adaptive responses in future-related settings. Dysfunction of these fundamental processes could thereby contribute to the pathophysiology of mood disorders. Recovery could occur by the induction of the appropriate plasticity or remodeling. These possibilities are supported by preclinical and clinical studies, demonstrating that there are structural alterations that occur in response to stress and in patients with mood disorders, such as MDD.23
In the case of this study, it is proposed that prolonged wakefulness (sleep deprivation) shifts the initially deficient inducibility of associative synaptic long-term potentiation in patients with MDD, into a more favorable window of associative plasticity.22 In other words, it remediates the deficient neuroplasticity in individuals with MDD.
The synaptic plasticity model of sleep deprivation in MDD suggests a novel framework for a potential mechanism of action of therapeutic sleep deprivation that can be further tested in humans through non-invasive measures, and in animals (i.e. rodents) based on synaptic plasticity studies. Further determining the mechanism of action of sleep deprivation might contribute to the development of novel fast acting treatments for MDD, one of the major health problems world wide.22
Potential underlying molecular mechanisms
Brain Derived Neurotrophic Factor (BDNF): Plays a key role in synaptic plasticity in the adult brain. Decreased BDNF expression is associated with reduced synaptic plasticity and neuronal atrophy, while increased BDNF expression is associated with neuronal survival and differentiation. BDNF levels increase with prolonged periods of wakefulness, facilitating associative synaptic plasticity. This could potentially provide a mechanism for the clinical improvement after therapeutic sleep deprivation in MDD.22
Adenosine: Adenosine is important in sleep regulation, and its absence has also been implicated in a greater risk for depression. Adenosine release is increased the longer you're awake (to a point), making you feel less aroused and more tired, and acting as part of your normal sleep-wake cycle. A beneficial side effect of its release also appears to be an alleviation of depressive symptoms. Several animal studies suggest that activation of adenosine A1 receptors in the brain has an antidepressant effect.22
Monoaminergic: The therapeutic effects of SD are comparable to the rapid onset of mood changes after the treatment with psychostimulants. Psychostimulants increase the release of all monoamines or inhibit the reuptake of these neurotransmitters, leading to the net effect of increased synaptic dopamine, noradrenaline and serotonin. The therapeutic effects of SD may be mimicking the effects of psychostimulants.22
Glutamatergic System: Under physiological conditions, glutamate has a prominent role in synaptic plasticity, learning and memory. Therapeutic sleep deprivation may have various effects on glutamate transmission.22
Treatments
Sleep
Although obvious, the best treatment for sleep deprivation is ultimately more sleep. Being deprived of sleep may be chronic, occurring consistently for a period of time or acute, for example an all-nighter. Everyone is unique in the amount of sleep they need to function efficiently, and our typical requirements fluctuate throughout our lives. It is common for the issue to be the quality of the sleep, such as sleep apnea or insomnia.24 In these situations, despite sleeping adequate times the individual does not receive the same quality of sleep within the 8 hours, thus they don’t awake as energized a normal person would.24 For individuals suffering from acute sleep deprivation, a single night of eight hours of sleep may be adequate to recover. However, for someone suffering from chronic sleep deprivation, they may need to extend their nightly sleep hours as well as taking additional naps during the day.24 Furthermore, it may take younger people slightly longer to recover from sleep deprivation.
Stay Active
The second treatment completely contradicts the first; being more active. During episodes of minor sleep deprivation, periods of activity help individuals stay alert. For example, a five-minute walk has been shown to improve excessive daytime sleepiness based on results from a multiple sleep latency testing (MSLT).24 However, these benefits may be temporary, in addition to having little impact on individuals suffering from profound sleep deprivation. Furthermore, depending on individual activity levels, some people may experience the opposite of the desired effect and have increased fatigue.24
Bright Light
Exposure to bright light has been seen to have an impactful effect on the human body’s circadian rhythm; a pattern of bodily functions timed to the day-night cycle such as sleep and wakefulness.24 Certain conditions such as seasonal affective disorder (SAD) and circadian rhythm sleep disorders can be helped by time-specific exposure to bright light, which may also increase alertness if you are sleep deprived.24 However, the effectiveness of this approach is still debated; some results show that light is effective in shifting circadian rhythms, potentially increasing your sleep latency, or ability to sleep.24 Moreover, some studies have shown that bright light is positively correlated to improved performance.
Noise
Novel stimuli such as noise trigger a response in the brain, which makes us slightly more alert.24 Although this can pose a problem when falling asleep, it is a moderate solution to another common issue faced by those suffering from sleep deprivation, which is staying awake. When we are exposed to background noise for too long (ex. fans, humming from a computer, etc.), the sound eventually fades into the background.24 However, novel sounds tend to capture our attention and thus, can be useful in keeping us awake.
Posture
Similar to how it is more difficult to fall asleep standing or sitting upright, certain postures may improve the quality of ones sleep. Improper sleep posture can intensify fatigue, sleep apnea, headaches, heartburn, backaches and other factors that lead to sleep deprivation.24 For example, for those suffering from sleep apnea or snoring, back sleeping is detrimental while side sleeping is beneficial as it keeps ones airways open.24 With the exception of medical conditions that necessitate certain positions, your natural sleeping position is generally recommended as it based on how well you’re able to breath.24 Thus, it is important to ensure the removal of any factors impacting your ability to sleep in certain positions such as your mattress. With old, worn-out mattresses that sag in the middle, sleeping on your side or stomach becomes difficult which hinders your ability to sleep naturally in a way that feels comfortable.
Caffeine
One of the cheapest, most effective treatments for sleep deprivation is caffeine; a naturally occurring stimulant found in coffee, tea, chocolate and an assortment of other readily available foods and drinks.24 It is widely used, especially in North America where vendors such as Starbucks and Tim Horton’s are common. Caffeine increases ones alertness and is well tolerated with minor side effects such as trembling when excess is consumed or headaches during withdrawal periods.24
Stimulant Drugs
In addition to caffeine, there are additional stimulants available as prescription or over-the-counter drugs, which may help to increase alertness and symptoms of sleep deprivation. Examples include methylphenidate, modafinil and armodafanil.24 Although prescription drugs increase alertness, they also may have hurtful side effects, thus they are generally reserved for conditions such as narcolepsy or attention deficit hyperactivity disorder (ADHD).24
Sleep Hygiene Tips to Combat Sleep Deprivation
- Avoid watching TV, eating, discussing emotional ordeals and other activities aside from sleeping in bed. By doing so, one can mentally associate the bed with these additional activities, making it difficult to fall asleep.25
- Maintain a comfortable temperature, not too warm (above 24C) or too cold (below 13C) in order to keep your body’s homeostasis in check.25
- Keep naps between 15-25 minutes about eight hours after waking up, however, if you find it difficult to fall asleep eliminate them completely.25
- Avoid nicotine prior to bedtime (ex. cigarettes) and cut off caffeine 4-6 hours prior to sleeping. However, be careful to consume small quantities throughout the day, as ingesting large amounts and cutting yourself off can cause headaches and other side effects.25
- Eating a light snack may increase sleepiness, however eating too heavy will interfere with your ability to sleep. Carbohydrates and dairy products are recommended, while proteins should be avoided.25
- If you are aroused by exercise stick to working out in the morning or during the day, as the excitement from late night workouts may hinder your ability to sleep.25
- Avoid sleeping with pets; this may also cause arousal from allergies or movements in bed.25
- If nighttime urination is a problem, or you’re constantly awakened by the need to go to the washroom, avoid the consumption of liquids past 8PM.25
References
1. Zepelin H, Siegel JM, Tobler I. Mammalian sleep. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. 4th ed. Philadelphia: Elsevier/Saunders; 2005. pp. 91–100
2. Altevogt, B. M., & Colten, H. R. (Eds.). (2006). Sleep Disorders and Sleep Deprivation:: An Unmet Public Health Problem. National Academies Press.
3. Taskar, V., & Hirshkowitz, M. (2003). Health effects of sleep deprivation.Clinical Pulmonary Medicine, 10(1), 47-52.
4. McEwen, B. S., & Karatsoreos, I. N. (2015). Sleep deprivation and circadian disruption: stress, allostasis, and allostatic load. Sleep medicine clinics,10(1), 1-10.
5. Aguirre, C. (2015, November 15). What would happen if you didn’t sleep? – Claudia Aguirre [Video File]. Retrieved from http://ed.ted.com/lessons/what-would-happen-if-you-didn-t-sleep-claudia-aguirre
6. Jessen, N. A., Munk, A. S. F., Lundgaard, I., & Nedergaard, M. (2015). The glymphatic system: a beginner’s guide. Neurochemical research, 40(12), 2583-2599.
7. Plog, B. A., Dashnaw, M. L., Hitomi, E., Peng, W., Liao, Y., Lou, N., … & Nedergaard, M. (2015). Biomarkers of traumatic injury are transported from brain to blood via the glymphatic system. The Journal of Neuroscience, 35(2), 518-526.
8. Irwin, M. R., Bjurstrom, M. F., & Olmstead, R. (2016). Polysomnographic Measures of Sleep in Cocaine Dependence and Alcohol Dependence: Implications for Age‐Related Loss of Slow Wave, Stage 3 Sleep. Addiction.
9. Cohrs, S. (2008) Sleep disturbances in patients with schizophrenia: impact and effect of antipsychotics. CNS Drugs, 22, 939–962.
10. Christensen, J. A. E., Jennum, P., Koch, H., Frandsen, R., Zoetmulder, M., Arvastson, L., … & Sorensen, H. B. D. (2016). Sleep stability and transitions in patients with idiopathic REM sleep behavior disorder and patients with Parkinson’s disease. Clinical Neurophysiology, 127(1), 537-543.
11. Epstein, L. J., Kristo, D., Strollo Jr, P. J., Friedman, N., Malhotra, A., Patil, S. P., … & Weinstein, M. D. (2009). Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. Journal of Clinical Sleep Medicine, 5(3), 263-276.
12. Lee-Iannotti, J. K., & Parish, J. M. (2016). Suvorexant: a promising, novel treatment for insomnia. Neuropsychiatric Disease and Treatment, 12, 491–495.
13. Lustberg, L., & Reynolds, C. F. (2000). Depression and insomnia: questions of cause and effect. Sleep medicine reviews, 4(3), 253-262.
14. Knutson, K. L., Spiegel, K., Penev, P., & Van Cauter, E. (2007). The metabolic consequences of sleep deprivation. Sleep medicine reviews,11(3), 163-178.
15. Altevogt, B. M., & Colten, H. R. (Eds.). (2006). Sleep Disorders and Sleep Deprivation:: An Unmet Public Health Problem. National Academies Press.
16. Naitoh, P., Kelly, T. L., & Englund, C. (1990). Health effects of sleep deprivation (No. NHRC-89-46). NAVAL HEALTH RESEARCH CENTER SAN DIEGO CA.
17. Luby, E. D., Grisell, J. L., Frohman, C. E., Lees, H., Cohen, B. D., & Gottlieb, J. S. (1962). Biochemical, psychological, and behavioral responses to sleep deprivation. Annals of the New York Academy of Sciences, 96(1), 71-79.
18. Durmer, J. S., & Dinges, D. F. (2005). Neurocognitive Consequences of Sleep Deprivation. Seminars in Neurology, 25(01), 117-129.
19. Thacher, P. V. (2008). University students and the “All Nighter”: Correlates and patterns of students' engagement in a single night of total sleep deprivation. Behavioral Sleep Medicine, 6(1), 16-31.
20. Meerlo, P., Sgoifo, A., & Suchecki, D. (2008). Restricted and disrupted sleep: effects on autonomic function, neuroendocrine stress systems and stress responsivity. Sleep Medicine Reviews, 12(3), 197-210.
21. Curcio, G., Ferrara, M., & De Gennaro, L. (2006). Sleep loss, learning capacity and academic performance. Sleep Medicine Reviews, 10(5), 323-337.
22. Wolf, E., Kuhn, M., Norman, C., Mainberger, F., Maier, J. G., Maywald, S., … & Riemann, D. (2016). Synaptic plasticity model of therapeutic sleep deprivation in major depression. Sleep Medicine Reviews, 30, 53-62
23. Duman, R. S. (2002). Pathophysiology of depression: the concept of synaptic plasticity. European psychiatry, 17, 306-310.
24. Peters, B. (2016, January 27). What Is the Treatment for Sleep Deprivation? Retrieved March 30, 2016, from http://sleepdisorders.about.com/od/sleepdisorderstreatment/ss/What-Is-The-Treatment-For-Sleep-Deprivation.htm
25. Feature, M. J. (2005, June 29). How to Sleep Better: Sleep Deprivation Solutions. Retrieved March 30, 2016, from http://www.webmd.com/sleep-disorders/features/sleep-hygiene